(feeding on fermentation products and producing decay products).
Modification of the quantitative ratio and species composition of the normal microflora of an organ, mainly the intestine, accompanied by the development of microbes atypical for it, is called - this is a condition caused by a violation of the intestinal microflora associated with a change in the species composition of bacteria. Most often this happens due to malnutrition. But a violation of the microflora can occur not only due to malnutrition, but also due to the intake of various.
Remember that with dysbacteriosis, probiotics can have a certain effect, but a healthy body most often does not need additional preparations with beneficial bacteria.
Probiotics and prebiotics work differently.
Prebiotics - these are substances that are not absorbed in the small intestine, but stimulate the development of normal intestinal microflora, this is the "food" for our native bacteria. Prebiotics are not afraid of acids and enzymes, so they bypass the stomach without loss and enter the intestine unchanged.
The mechanism of action of prebiotics in the body is quite simple. A person ate a prebiotic preparation or a product with dietary fiber, and they enter the intestines and feed our microflora there. From such a diet, beneficial bacteria begin to multiply, and balance can be restored.
They are taken as a preventive measure and in the early stages of dysbacteriosis, and in advanced cases, prebiotics are not effective. In such situations, you will need to drink a course of special drugs.
Probiotics - these are "useful strangers", microorganisms useful to humans, non-toxic and non-pathogenic living microorganisms, and substances of microbial or other origin, which are contained in some food products, or sold as dietary supplements in a pharmacy, and normally constitute a healthy human biocenosis. The word “probiotics” (probio) literally means “for life” in Latin. Probiotics are divided into two main types: lactobacilli and bifidobacteria. In turn, lactobacilli and bifidobacteria are divided into many strains, each of which can be useful in the treatment of certain conditions.
Live bacteria, according to the descriptions, are in tablets, capsules, and even vaginal suppositories. However, large-scale studies confirming their effectiveness in the treatment of various diseases have not yet been published.
Although the phrase “You are what you eat” is gaining more confident scientific justification. The composition of the intestinal flora changes depending on your diet.
Normal intestinal microflora
The main representatives of the mandatory microflora of the human colon are bifidobacteria, bacteriods, lactobacilli, and enterococci. They make up 99% of all microbes, only 1% of the total number of microorganisms belongs to opportunistic bacteria, such as Proteus, Clostridia, Pseudomonas aeruginosa and others. Pathogenic microflora in the normal state of the intestine should not be, the normal intestinal microflora in humans begins to develop already during the passage of the fetus through the birth canal. Its formation is completely completed by the age of 7-13.
What is the function of the normal intestinal microflora?
The normal intestinal microflora performs numerous interrelated functions to maintain the homeostasis of the body, along with its other organs and systems. One of the main functions of the intestinal normoflora is a barrier, primarily protection from foreign microflora that enters the gastrointestinal tract.
Bacteria live in the gastrointestinal tract, inhabit our skin, mouth and other mucous membranes and take an active part everywhere. Man and microflora are a real superorganism, and we need each other! So it is in your interest to take care of your body and nourish it not only from the outside, but also from the inside.
Bifidobacteria create an acidic environment, releasing organic acids that inhibit the growth and reproduction of pathogenic and putrefactive bacteria. Lactobacilli have antibacterial activity due to their ability to form lactic acid, lysozyme and other antibiotic substances. Lactobacilli in the process of fermentation of carbohydrates form substances with antibiotic activity (lysozyme, acidophilus, etc.), Escherichia - colicins that inhibit the growth of enteropathogenic. Colibacteria antagonistically act on pathogenic flora through immune mechanisms. In addition, on the surface of the cells of the intestinal epithelium, representatives of the normal microflora form the so-called "microbial turf", which mechanically protects the intestine from the penetration of pathogenic microbes. In addition to the protective function, normal microorganisms of the large intestine are involved in the metabolism of the macroorganism. They synthesize, proteins, many vitamins, take part in the exchange. Lactobacilli synthesize enzymes that break down milk proteins, as well as the enzyme histaminase, thereby performing a desensitizing function in the body.
An important function of the microflora is the synthesis of a number of vitamins. The human body receives vitamins mainly from the outside - with food of plant or animal origin. Incoming vitamins are normally absorbed in the small intestine and partially utilized by the intestinal microflora. Microorganisms that inhabit the intestines of humans and animals produce and utilize many vitamins. It is noteworthy that the microbes of the small intestine play the most important role for humans in these processes, since the vitamins they produce can be effectively absorbed and enter the bloodstream, while the vitamins synthesized in the large intestine are practically not absorbed and are inaccessible to humans. Suppression of microflora (for example, by antibiotics) also reduces the synthesis of vitamins. On the contrary, the creation of favorable conditions for microorganisms, for example, by eating a sufficient amount of prebiotics, increases the supply of vitamins to the macroorganism.
Currently, aspects related to the synthesis of folic acid, vitamin B12 and vitamin K by the intestinal microflora are the most studied.
There are a number of social factors that disrupt the microflora. It is primarily acute and chronic. Such "critical" conditions for human health are subject to both adults. Another reason why the microflora suffers is nutrition. Our diet today is high in carbohydrates and low in protein. Simple and healthy food has a beneficial effect on the microflora.
Also, the cause of violations of the intestinal microflora are diseases of the gastrointestinal tract, fermentopathy, active therapy with antibiotics, sulfa drugs, chemotherapy, hormonal therapy. Dysbacteriosis is favored by harmful environmental factors, depletion of the body due to serious illnesses, surgical interventions, illness, and a decrease in the body's immunological reactivity.
Pathogenic bacteria that enter the body from the outside cause acute intestinal infections. Bacteria can enter the human body through contaminated,,,, water or by contact with an already infected person. Another way of infection is insufficient personal.
How can you check the intestinal microflora?
To determine the microflora in humans (normal or not), it is necessary to take a stool test, which detects dysbacteriosis. This is a special research technique that allows you to accurately determine the number of certain microbes that inhabit the intestines.
In patients with polyposis of the large intestine, an increased content of eubacteria is detected in the feces.
If the microflora is disturbed in the small intestine, then this can lead to bloating and flatulence. A breath test helps to determine the failure of the intestines, during which an increase in the concentration of hydrogen is detected. This happens if anaerobic bacteria are overactive.
In cases where there are signs indicating an intestinal infection, a smear is taken from the rectum. For several days, it is grown on a nutrient medium, after which it is examined under a microscope to identify the type of pathogenic microbe that provoked the disease.
How to restore the intestinal microflora
The restoration of microflora is a long process involving the elimination of pathogenic organisms and the settlement of non-pathogenic or other drugs.
Regular consumption of foods that contain a lot of fiber and will help restore the required amount of healthy bacteria. These are fresh fruits, vegetables, as well. But sweet and floury dishes, as well as meat, will have to be abandoned for a while. It is better to stock up on various cereals and coarse grinding, which will help restore normal stools, as well as make the intestinal muscles work and help restore the absorption function of the intestinal mucosa.
All kinds of fermented milk products are very useful for returning a healthy microflora to this body. Once in our body, lactic acid bacteria have a detrimental effect on the putrefactive environment and help beneficial bacteria to recover.
Often, patients categorically refuse to consume fermented milk products, referring to the fact that, for example, they do not like the taste from childhood. In fact, today on the shelves of stores there is a huge selection of various fermented milk drinks, among which ideal anyone can choose for themselves.
You can also easily improve the taste of the usual kefir with fresh berries and fruits. For example, a handful of fresh or frozen strawberries and a spoonful of honey will turn it into a real treat. In a blender, this drink with berries and honey will turn into a delicious healing drink.
If possible, it is better to cook fermented milk products yourself. For example, modern yogurt makers will help you do this without much effort. They are the most useful and effective in the fight against dysbacteriosis.
It will also be very useful to eat one garlic an hour before and dinner. It will also speed up the process of restoring the intestinal microflora. True, this advice will have to be abandoned by all those who have any.
The amount of water you drink every day is also important. Calculate the rate for yourself is based on the calculation of 0.3 liters for every 10 kilograms of weight. Water must be clean and fresh. Not carbonated!
It is very important, restoring the microflora, to stop using all kinds of hormonal and hypnotic drugs, as well as in large quantities and energy . All these funds become a real stress for the body and negatively affect not only the functioning of the intestines, but also many other organs.
If, for example, hormonal drugs are indicated for use by a doctor, then you should finish the course of treatment and then begin to actively restore the intestinal microflora.
Folk remedies for restoring intestinal microflora
There are many folk recipes that will help in restoring the microflora. The most effective and efficient among them:
Before each meal, drink a glass of fresh cabbage pickle. It is best if sauerkraut was cooked on your own at home, and not bought in a store. Before use, the brine must be slightly warmed in a water bath or in a microwave oven.
Add to all from fresh vegetables grated apples (necessarily sour!).
Eat a small amount of lingonberries fresh every day. If there is no way to get fresh berries, you can replace them with dried ones.
Replace coffee, black and green with various herbal decoctions. For example, brew black and raspberry leaves, as well as chamomile and mint. Such useful "tea" will positively affect not only the condition of the human intestines, but also the whole organism as a whole.
In any case, the restoration of the intestinal microflora must be comprehensive. It is not enough to use only folk remedies, they must be combined with a diet.
Prevention of microflora
In order to be in good shape, a person needs to maintain a balance of microflora that supports his immune system. Thus, we help the body resist stress and cope with pathogenic microbes on its own.
You need to take care of your health every day. This should become as common as brushing your teeth in the morning or taking vitamins.
Prevention of violations of microflora is aimed at maintaining beneficial bacteria in the body. As a preventive measure, systematic is extremely useful. This is facilitated by eating foods rich in plant fiber (vegetables, fruits, cereals, wholemeal bread), as well as fermented milk products. Today, on TV screens, we are offered to start the day with a “sip of health”: kefirs and yogurts enriched with bifidobacteria. In this case, the intestinal microflora will be in order and additional drugs will not be needed. However, it must be remembered that the amount of these beneficial elements in products with a long shelf life is quite small in order to stimulate the growth of microflora. In some products, probiotics are easily killed: when they are heated, added, stabilizers, as well as at a high concentration of lactic and other acids in yogurt or kefir.
Therefore, as a preventive measure, it is worth considering fresh and natural fermented milk products (tan, kefir) containing truly “live cultures”. As a rule, these products are sold in pharmacy chains, in farm stores, and their shelf life is limited. It is best to drink yogurts natural and without additives, without sugar, you can always add something at will to ordinary yogurt, for example, fresh fruits or dried fruits. Foods that are high in sugar can feed pathogenic bacteria that won't benefit your microbiota.
Read also:
|
Human organism inhabited (colonized) by more than 500 species of microorganisms that make up the normal human microflora, which are in a state of equilibrium (eubiose) with each other and with the human body. Microflora is a stable community of microorganisms, i.e. microbiocenosis. It colonizes the surface of the body and cavities that communicate with the environment. The habitat of a community of microorganisms is called biotope. Normally, microorganisms are absent in the lungs and uterus. There are normal microflora of the skin, mucous membranes of the mouth, upper respiratory tract, digestive tract and genitourinary system. Among the normal microflora, resident and transient microflora are distinguished. Resident (permanent) obligate microflora is represented by microorganisms that are constantly present in the body. Transient (non-permanent) microflora is not capable of long-term existence in the body.
Microflora of the digestive tract is the most representative in its qualitative and quantitative composition. At the same time, microorganisms live freely in the cavity of the digestive tract, and also colonize the mucous membranes.
In the oral cavity actinomycetes, bacteroids, bifidobacteria, eubacteria, fusobacteria, lactobacilli, hemophilic rods, leptotrichia, neisseria, spirochetes, streptococci, staphylococci, veillonella, etc. live. Fungi of the genus Candida and protozoa are also found. Associates of normal microflora and their metabolic products form plaque.
Microflora of the stomach represented by lactobacilli and yeast, single gram-negative bacteria. It is somewhat poorer than, for example, the intestines, since gastric juice has a low pH value, which is unfavorable for the life of many microorganisms. With gastritis, gastric ulcer, curved forms of bacteria are found - Helicobacter pylori, which are the etiological factors of the pathological process.
In the small intestine there are more microorganisms than in the stomach; bifidobacteria, clostridia, eubacteria, lactobacilli, anaerobic cocci are found here.
The largest number of microorganisms accumulate in colon. 1 g of feces contains up to 250 billion microbial cells. About 95% of all types of microorganisms are anaerobes. The main representatives of the colon microflora are: gram-positive anaerobic rods (bifidobacteria, lactobacilli, eubacteria); gram-positive spore-forming anaerobic rods (clostridia, perfringens, etc.); enterococci; gram-negative anaerobic rods (bacteroids); Gram-negative facultative anaerobic rods (E. coli and similar bacteria.
The microflora of the colon- a kind of extracorporeal organ. It is an antagonist of putrefactive microflora, as it produces lactic, acetic acids, antibiotics, etc. Its role in water-salt metabolism, regulation of intestinal gas composition, metabolism of proteins, carbohydrates, fatty acids, cholesterol and nucleic acids, as well as the production of biologically active compounds - antibiotics, vitamins, toxins, etc. The morphokinetic role of microflora lies in its participation in the development of organs and body systems; it also takes part in the physiological inflammation of the mucous membrane and the change of the epithelium, digestion and detoxification of exogenous substrates and metabolites, which is comparable to the function of the liver. Normal microflora also performs an antimutagenic role, destroying carcinogenic substances.
Representatives of the so-called normal microflora live on the skin, in the urogenital tract, in the pancreas, etc., as well as on the mucous membranes of the upper respiratory tract and perform functions peculiar only to them, which we have already discussed in detail in previous chapters...
Including normal microflora is present in a small amount in the esophagus (this microflora practically repeats the microflora of the upper respiratory tract), in the stomach (the microbial composition of the stomach is poor and is represented by lactobacilli, streptococci, helicobacteria and yeast-like fungi resistant to stomach acid), in the duodenum and in the small intestine, the microflora is not numerous (represented mainly by streptococci, lactobacilli, veillonella), in the sub-air intestine, the number of microbes is higher (E. coli, etc. are added to all of the above microorganisms). But the largest number of microorganisms of normal microflora lives in the large intestine.
About 70% of all microorganisms of normal human microflora are concentrated in the large intestine. If you put together the entire intestinal microflora - all its bacteria, then put it on a scale and weigh it, then you get about three kilograms! We can say that the human microflora is a separate human organ, which is of great importance for human life as well as the heart, lungs, liver, etc.
The composition of the intestinal microflora of a healthy person
99% of the microbes in the intestines are useful human helpers. These microorganisms are permanent inhabitants of the intestine, so they are called permanent microflora. These include:
- The main flora is bifidobacteria and bacteroids, the amount of which is 90-98%;
- Associated flora - lactobacilli, propionobacteria, E. coli, enterococci. Their number is 1-9% of all bacteria.
Under certain conditions, all representatives of the normal microflora, with the exception of bifido-, lactobacilli and propionobacteria, have the ability to cause diseases, i.e. bacteroids, Escherichia coli, enterococci, under certain circumstances, have pathogenic properties (I will talk about this a little later).
- Bifidobacteria, lactobacilli, propionobacteria are absolutely positive microorganisms and under no circumstances will they perform a pathogenic harmful function in relation to the human body.
But in the intestine there is also the so-called residual microflora: staphylococci, streptococci, clostridia, klebsiella, yeast-like fungi, citrobacter, veillonella, proteus and some other “malicious” pathogenic microorganisms ... As you understand, under certain conditions, these microorganisms perform a lot of pathogenic harmful to human functions. But in a healthy state of a person, the number of these bacteria does not exceed 1%, respectively, while they are in the minority, they simply cannot do any harm, but, quite the contrary, they benefit the body, being a conditionally pathogenic microflora and performing an immunogenic function (this function one of the main functions of the microflora of the upper respiratory tract, I already mentioned it in chapter 17).
Microflora imbalance
All these bifidobacteria, lactobacilli and others perform a huge number of different functions. And if the normal composition of the intestinal microflora is shaken, the bacteria will not be able to cope with their functions, then ...
Vitamins from food simply will not be absorbed and assimilated, hence a million diseases.
A sufficient amount of immunoglobulins, interferons, lysozyme, cytokines and other immune factors will not be produced, which will result in a decrease in immunity and endless colds, infectious diseases, acute respiratory infections, acute respiratory viral infections, and influenza. A small amount of the same immunoglobulins, interferons, lysozyme, etc. will also be in mucous secretions, as a result of which the microflora of the respiratory tract will be disturbed and cause a variety of rhinitis, pharyngitis, tonsillitis, bronchitis, etc. The acid balance in the nasal cavity, in the pharynx, in the throat, in the mouth will be disturbed - pathogenic bacteria will continue to increase their populations.
If the renewal of the cells of the intestinal mucosa is disturbed, many different poisons and allergens that must remain in the intestines will now begin to be absorbed into the blood, poisoning the entire body, hence all kinds of diseases arise, including many allergic diseases (bronchial asthma, allergic dermatitis, etc.). ).
Digestive disorders, absorption of decay products of putrefactive microflora can be reflected in peptic ulcer, colitis, gastritis, etc.
If patients with diseases of the gastrointestinal tract, for example, pancreatitis, have intestinal dysfunction, then dysbacteriosis, which successfully develops against the background of this disease, is most likely to blame.
Gynecological diseases (during the transition of microorganisms to the skin of the perineum, and then to the genitourinary organs), purulent-inflammatory diseases (boils, abscesses, etc.), metabolic disorders (menstrual irregularities, atherosclerosis, urolithiasis, gout), etc.
Disorders of the nervous system with various manifestations, etc.
Diseases caused by intestinal dysbacteriosis can be listed for a very, very long time!
The human body is a very fine system that is capable of self-regulation, this system is not easy to unbalance ... But some factors still affect the composition of the intestinal microflora. These may include the nature of nutrition, season, age, but these factors have little effect on fluctuations in the composition of microflora and are quite fixable, the balance of microflora is restored very quickly or a slight imbalance does not affect human health in any way. The question arises differently when, due to serious malnutrition or some other reasons, the biological balance of the intestinal microflora is disturbed and begins to pull along a whole chain of reactions and disturbances in the work of other organs and systems of the body, mainly diseases of the nasal cavity, throat, lungs, frequent colds, etc. That's it then and you need to talk about dysbacteriosis.
and recipes for diseases:
Join, speak up and discuss. Your opinion can be very important for many readers!
Copying materials without written permission and open links is prohibited.
Barrier function - neutralization of various toxins and allergens;
Enzymatic function - the production of a significant amount of digestive enzymes and, above all, lactase;
Ensuring normal motility of the gastrointestinal tract;
Participation in metabolism;
Participation in the body's immune responses, stimulation of defense mechanisms and competition with pathogenic and opportunistic microorganisms.
Obligate - the main or indigenous microflora (it includes bifidobacteria and bacteroids), which make up 90% of the total number of microorganisms;
Optional - saprophytic and conditionally pathogenic microflora (lactobacilli, escherichia, enterococci), which is 10% of the total number of microorganisms;
Residual (including transient) - random microorganisms (citrobacter, enterobacter, proteus, yeast, clostridia, staphylococci, aerobic bacilli, etc.), which is less than 1% of the total number of microorganisms.
Mucosal (M) flora - mucosal microflora interacts with the mucous membrane of the gastrointestinal tract, forming a microbial-tissue complex - microcolonies of bacteria and their metabolites, epithelial cells, goblet cell mucin, fibroblasts, immune cells of Peyer's plaques, phagocytes, leukocytes, lymphocytes, neuroendocrine cells;
Translucent (P) flora - translucent microflora is located in the lumen of the gastrointestinal tract, does not interact with the mucous membrane. The substrate for its life activity is indigestible dietary fiber, on which it is fixed.
Endogenous factors - the influence of the mucous membrane of the digestive canal, its secrets, motility and the microorganisms themselves;
Exogenous factors - influence directly and indirectly through endogenous factors, for example, the intake of a particular food changes the secretory and motor activity of the digestive tract, which transforms its microflora.
Bacteroides (especially Bacteroides fragilis),
Anaerobic lactic acid bacteria (eg Bifidumbacterium),
Clostridia (Clostridium perfringens),
Gram-negative coliform bacteria (primarily Escherichia coli - E.Coli),
Fungi of the genus Candida
Separate types of spirochetes, mycobacteria, mycoplasmas, protozoa and viruses.
Intestinal dysbacteriosis. Causes, symptoms, modern diagnosis and effective treatment
Frequently asked Questions
The site provides background information. Adequate diagnosis and treatment of the disease is possible under the supervision of a conscientious physician.
Anatomy and physiology of the intestine
- The small intestine, which is the initial section of the intestine, consists of loops, longer than the large intestine (from 2.2 to 4.4 m) and smaller in diameter (from 5 to 3 cm). It digests proteins, fats and carbohydrates. The small intestine begins at the pylorus and ends at the ileocecal angle. The small intestine is divided into 3 sections:
- The initial section - the duodenum, starts from the pylorus of the stomach, has the shape of a horseshoe, goes around the pancreas;
- The jejunum is a continuation of the duodenum, it is approximately the initial 6-7 loops of the small intestine, the border between them is not expressed;
- The ileum is a continuation of the jejunum, represented by the following 7-8 loops. It ends with a confluence at a right angle into the initial part of the large intestine (caecum).
- The large intestine is the final part of the digestive tract, where water is absorbed and stool is formed. It is located so that it borders (surrounds) the loops of the small intestine. Its wall forms protrusions (gaustra), which is one of the differences from the wall of the small intestine. The length of the large intestine is about 150 cm and the diameter is from 8 to 4 cm, depending on the department. The large intestine consists of the following sections:
- The caecum with the appendicular process is the initial section of the large intestine, located below the ileocecal angle, its length is from 3 to 8 cm;
- The ascending part of the colon is a continuation of the cecum, occupies the extreme right lateral position of the abdominal cavity, rises from the level of the ilium to the level of the lower edge of the right lobe of the liver, and ends with the right bend of the colon;
- The transverse colon, starts from the right colonic flexure (the level of the right hypochondrium), runs in the transverse direction and ends with the left flexure of the colon (the level of the left hypochondrium);
- The descending part of the colon occupies the extreme left lateral position of the abdominal cavity. It starts from the left bend of the colon, goes down to the level of the left ilium;
- The sigmoid colon, 55 cm long, is a continuation of the previous section of the intestine, and at the level of the 3rd sacral vertebra passes into the next section (rectum). The diameter of the sigmoid colon, compared with the diameter of the other parts of the large intestine, is the smallest about 4 cm;
- The rectum, is the final section of the large intestine, has a length of about 18 cm. It starts from the level of the 3rd sacral vertebra (the end of the sigmoid colon) and ends with the anus.
What is normal intestinal flora?
Normally, the intestinal flora is represented by 2 groups of bacteria:
Symptoms characteristic of the 3rd and 4th degree of intestinal dysbacteriosis:
- Stool disorder:
- Most often it manifests itself in the form of loose stools (diarrhea), which develops as a result of increased formation of bile acids and increased intestinal motility, inhibiting the absorption of water. Later the stool becomes foul-smelling, tainted with blood or mucus;
- With age-related (in the elderly) dysbacteriosis, constipation most often develops, which is caused by a decrease in intestinal motility (due to a lack of normal flora).
- Bloating is caused by increased formation of gases in the large intestine. The accumulation of gases develops as a result of impaired absorption and removal of gases by an altered intestinal wall. Swollen intestines can be accompanied by rumbling, and cause unpleasant sensations in the abdominal cavity in the form of pain.
- Cramping pain is associated with an increase in pressure in the intestines, after the passage of gases or stools, it decreases. With dysbacteriosis of the small intestine, pain occurs around the navel, if the large intestine suffers, the pain is localized in the iliac region (lower abdomen on the right);
- Dyspeptic disorders: nausea, vomiting, belching, loss of appetite, are the result of impaired digestion;
- Allergic reactions, in the form of skin itching and rashes, develop after eating foods that usually did not cause allergies, are the result of insufficient antiallergic action, disturbed intestinal flora.
- Symptoms of intoxication: there may be a slight increase in temperature up to 38 0 C, headaches, general fatigue, sleep disturbance, are the result of accumulation of metabolic products (metabolism) in the body;
- Symptoms that characterize a lack of vitamins: dry skin, seizures around the mouth, pale skin, stomatitis, changes in hair and nails, and others.
Complications and consequences of intestinal dysbacteriosis
- Chronic enterocolitis is a chronic inflammation of the small and large intestines, which develops as a result of long-term action of pathogenic intestinal flora.
- Deficiency of vitamins and microelements in the body leads to the development of iron deficiency anemia, hypovitaminosis of B vitamins and others. This group of complications develops as a result of impaired digestion and absorption in the intestine.
- Sepsis (blood infection) develops as a result of pathogenic flora from the intestines entering the patient's blood. Most often, such a complication develops when the patient does not seek medical help in time.
- Peritonitis develops as a result of the aggressive action of pathogenic flora on the intestinal wall, with the destruction of all its layers and the release of intestinal contents into the abdominal cavity.
- Accession of other diseases, as a result of a decrease in immunity.
- Gastroduodenitis, pancreatitis, develop as a result of the spread of pathogenic intestinal flora along the digestive tract.
- Weight loss of the patient develops as a result of impaired digestion.
Diagnosis of intestinal dysbacteriosis
- With the help of an objective examination, which includes palpation of the abdomen, pain is determined along the course of the small and / or large intestine.
- Microbiological examination of feces: performed to confirm the diagnosis, intestinal dysbacteriosis.
Indications for microbiological examination of feces:
- Intestinal disorders are long-term, in cases where it is not possible to isolate a pathogenic microorganism;
- Long recovery period after acute intestinal infections;
- The presence of purulent-inflammatory foci that are not amenable to antibiotic therapy;
- Impaired bowel function in individuals undergoing radiotherapy or exposure to radiation;
- Immunodeficiency states (AIDS, cancer and others);
- The lag of the infant in physical development and others.
Rules for taking feces for microbiological examination: before taking feces, 3 days before, it is necessary, it is necessary to be on a special diet that excludes products that increase fermentation in the intestines (alcohol, lactic acid products), as well as any antibacterial drugs. Feces are collected in a special sterile container, equipped with a lid, with a screwed-in spoon. In order to correctly evaluate the results, it is recommended to conduct a study 2-3 times, with an interval of 1-2 days.
There are 4 degrees of intestinal dysbacteriosis:
- 1 degree: characterized by a quantitative change in the ischerichia in the intestine, bifidoflora and lactoflora are not changed, most often they are not clinically manifested;
- Grade 2: quantitative and qualitative changes in ischerichia, i.e. a decrease in the amount of bifidoflora and an increase in opportunistic bacteria (fungi and others), accompanied by local inflammation of the intestines;
- Grade 3: change (decrease) in bifidus and lactoflora and the development of opportunistic flora, accompanied by intestinal dysfunction;
- Grade 4: the absence of bifidoflora, a sharp decrease in lactoflora and the growth of conditionally pathogenic flora, can lead to destructive changes in the intestine, followed by the development of sepsis.
Treatment of intestinal dysbacteriosis
Medical treatment
Groups of drugs used in intestinal dysbacteriosis:
- Prebiotics - have a bifidogenic property, i.e. contribute to the stimulation and growth and reproduction of microbes that are part of the normal intestinal flora. Representatives of this group include: Hilak-forte, Dufalac. Hilak-forte is prescribed drop by drop 3 times a day.
- Probiotics (eubiotics), these are preparations containing live microorganisms (i.e. bacteria of the normal intestinal flora), they are used to treat dysbacteriosis of 2-4 degrees.
- 1st generation drugs: Bifidumbacterin, Lifepack probiotics. They are liquid concentrates of lactobacilli and bifidobacteria, they are not stored for a long time (about 3 months). This group of drugs is unstable under the influence of gastric juice or enzymes of the gastrointestinal tract, which leads to their rapid destruction and insufficient concentration of them, the main disadvantage of 1st generation probiotics. Bifidumbacterin is administered orally, 5 doses of the drug 2-3 times a day, 20 minutes before meals;
- 2nd generation drugs: Baktisubtil, Flonivin, Enterol. They contain spores of bacteria of the normal intestinal flora, which secrete enzymes in the intestines of the patient for the digestion of proteins, fats and carbohydrates, stimulate the growth of bacteria of the normal intestinal flora, and also suppress the growth of putrefactive flora. Subtil is prescribed 1 capsule 3 times a day, 1 hour before meals;
- 3rd generation drugs: Bifikol, Lineks. They consist of several types of bacteria of the normal intestinal flora, therefore they are highly effective compared to the previous 2 generations of probiotics. Linex is prescribed 2 capsules 3 times a day;
- 4th generation drugs: Bifidumbacterin forte, Biosorb-Bifidum. This group of drugs is bacteria of the normal intestinal flora in combination with an enterosorbent (with activated charcoal or others). Enterosorbent, necessary to protect microorganisms, when passing through the stomach, it actively protects them from inactivation by gastric juice or enzymes of the gastrointestinal tract. Bifidumbacterin forte is prescribed 5 doses 2-3 times a day, before meals.
- Symbiotics (Bifidobak, Maltodofilus) are combined preparations (prebiotic + probiotic), i.e. at the same time stimulate the growth of normal flora and replace the missing amount of microbes in the intestine. Bifidobak is prescribed 1 capsule 3 times a day, with meals.
- Antibacterial drugs are used for the 4th degree of intestinal dysbacteriosis, to destroy the pathogenic flora. The most commonly used antibiotics are: groups of tetracyclines (Doxycycline), cephalosporins (Cefuroxime, Ceftriaxone), penicillins (Ampioks), nitroimidazoles: Metronidazole is prescribed 500 mg 3 times a day, after meals.
- Antifungal drugs (Levorin) are prescribed if there are yeast-like fungi such as Candida in the feces. Levorin is prescribed for 500 thousand units 2-4 times a day.
- Enzymes are prescribed in case of severe digestive disorders. Tablets Mezim 1 tablet 3 times a day, before meals.
- Sorbents are prescribed for pronounced signs of intoxication. Activated charcoal is prescribed 5-7 tablets at a time, for 5 days.
- Multivitamins: Duovit, 1 tablet 1 time per day.
Diet for intestinal dysbacteriosis
Prevention of intestinal dysbacteriosis
In second place in the prevention of intestinal dysbacteriosis is a balanced diet and a rational regimen.
Is there intestinal dysbacteriosis in general? Does such a disease exist?
Western doctors never give their patients such a diagnosis. In Russian health care, dysbacteriosis is mentioned in a document called "Standards (protocols) for the diagnosis and treatment of diseases of the digestive system", approved by order of the Ministry of Health of the Russian Federation No. other bowel diseases.
Surely, when you took a blood test, you heard such terms as “increased leukocytosis”, “increased ESR”, “anemia”. Dysbacteriosis is something similar. This is a microbiological concept, one of the manifestations of the disease, but not the disease itself.
How is intestinal dysbacteriosis indicated in the ICD?
Most often, such doctors use two codes:
- A04 - other bacterial intestinal infections.
- K63 - Other specified diseases of the digestive system.
In none of the two paragraphs does the word "dysbacteriosis" appear. So, the statement of such a diagnosis indicates that the disease is not fully diagnosed.
What diseases can be hidden under the term "dysbacteriosis"? Most often these are intestinal infections and helminthic infestations, celiac disease, irritable bowel syndrome, side effects of treatment with antibiotics, chemotherapy drugs and some other drugs, all kinds of diseases that weaken the immune system. In young children, bowel symptoms may be accompanied by atopic dermatitis.
Sometimes dysbacteriosis is a temporary condition, for example, in travelers, especially if they have poor personal hygiene. A “foreign” microflora enters the intestines, which a person does not encounter at home.
Which doctor treats intestinal dysbacteriosis?
Most often, diseases that lead to a violation of the composition of the intestinal microflora should be treated by an infectious disease specialist or a gastroenterologist. A general practitioner treats a number of diseases in adults, and a pediatrician in children.
What is the best treatment for intestinal dysbiosis?
Although, the relevant recommendations still exist - they are spelled out in the standard OST 91500.11.
But the effectiveness of these drugs in dysbacteriosis has not been proven. In the same OST there is such a phrase: “the degree of persuasiveness of evidence is C”. This means that sufficient evidence is missing. There is no evidence to recommend treatment of dysbacteriosis with these drugs.
Here it is once again appropriate to recall that doctors who work in clinics outside the CIS never make such a diagnosis to their patients, and even more so they do not prescribe treatment against dysbacteriosis.
Is there a link between intestinal dysbacteriosis and thrush?
The infection can develop in any organ. In this regard, candidiasis of the skin and nails, the oral mucosa (just this form is called thrush), intestines, and genital organs are isolated. The most severe form of the disease is generalized candidiasis, or candidal sepsis, when the fungus affects the skin, mucous membranes, and internal organs.
Candida is an opportunistic fungus. They are not always able to cause infection, but only under certain conditions. One of these conditions is a decrease in immunity. Thrush may well be combined with intestinal damage, which leads to dysbacteriosis. In fact, there is a connection between these two states.
In this case, the same reasons lead to the development of thrush and intestinal dysbacteriosis - a decrease in immunity and a fungal infection. They need to be treated.
Is it possible to use folk remedies for the treatment of intestinal dysbacteriosis?
Due to the fact that the topic is inflated and very popular, "remedies against dysbacteriosis" are offered by all kinds of traditional healers, healers, manufacturers of dietary supplements, MLM companies. Food manufacturers are not left out.
As already mentioned above, dysbacteriosis as a disease does not exist, it does not have its own specific symptoms, and it cannot be cured without eliminating the root cause. Therefore, first of all, you need to visit a doctor, undergo an examination, establish the correct diagnosis and begin treatment.
What can an analysis for dysbacteriosis show?
- The concept of "normal microflora" is very vague. Nobody knows the exact rules. Therefore, if you force any healthy person to take an analysis, many will have dysbacteriosis "revealed".
- The content of bacteria in feces is different from their content in the intestines.
- While the stool is delivered to the laboratory, the composition of the bacteria that are present in it may change. Especially if it is incorrectly assembled into a non-sterile container.
- The composition of the microflora in the human intestine can vary depending on different conditions. Even if you take the analysis at different times from the same healthy person, the results can vary greatly.
Profile login
Registration
It will take you less than a minute
Profile login
Intestinal microflora
The intestinal microflora in a broad sense is a combination of various microorganisms. In the human intestine, all microorganisms are in symbiosis with each other. On average, about 500 species of various microorganisms live in the human intestine, both beneficial bacteria (which help digest food and give vitamins and complete protein to a person) and harmful bacteria (which feed on fermentation products and produce decay products).
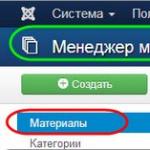
Modification of the quantitative ratio and species composition of the normal microflora of an organ, mainly the intestine, accompanied by the development of microbes atypical for it, is called dysbacteriosis. Most often this happens due to malnutrition.
But a violation of the microflora can occur not only due to malnutrition, but also due to the intake of various antibiotics. In any case, there is a violation of the microflora.
Normal intestinal microflora
The main representatives of the mandatory microflora of the human colon are bifidobacteria, bacteriods, lactobacilli, E. coli and enterococci. They make up 99% of all microbes, only 1% of the total number of microorganisms belongs to opportunistic bacteria such as staphylococci, proteus, clostridia, Pseudomonas aeruginosa and others. Pathogenic microflora in the normal state of the intestine should not be, the normal intestinal microflora in humans begins to develop already during the passage of the fetus through the birth canal. Its formation is completely completed by the age of 7-13.
What is the function of the normal intestinal microflora? First of all, protective. So, bifidobacteria secrete organic acids that inhibit the growth and reproduction of pathogenic and putrefactive bacteria. Lactobacilli have antibacterial activity due to their ability to form lactic acid, lysozyme and other antibiotic substances. Colibacteria antagonistically act on pathogenic flora through immune mechanisms. In addition, on the surface of the cells of the intestinal epithelium, representatives of the normal microflora form the so-called "microbial turf", which mechanically protects the intestine from the penetration of pathogenic microbes.
In addition to the protective function, normal microorganisms of the large intestine are involved in the metabolism of the macroorganism. They synthesize amino acids, proteins, many vitamins, take part in cholesterol metabolism. Lactobacilli synthesize enzymes that break down milk proteins, as well as the enzyme histaminase, thereby performing a desensitizing function in the body. The beneficial microflora of the colon promotes the absorption of calcium, iron, vitamin D, preventing the development of the oncological process.
Causes of violation of microflora
There are a number of social factors that disrupt the microflora. This is primarily acute and chronic stress. Such “critical” conditions for human health affect both children and adults. For example, a child goes to the first grade, respectively, he worries and worries. The process of adaptation in a new team is often accompanied by health problems. In addition, during the learning process, tests, exams, and workload can cause stress.
Another reason why the microflora suffers is nutrition. Our diet today is high in carbohydrates and low in protein. If you remember what the diet of our grandparents included, it turns out that they ate much more healthy food: for example, fresh vegetables, gray bread - simple and healthy food that has a beneficial effect on the microflora.
Also, the cause of violations of the intestinal microflora are diseases of the gastrointestinal tract, fermentopathy, active therapy with antibiotics, sulfa drugs, chemotherapy, hormonal therapy. Dysbacteriosis is favored by harmful environmental factors, starvation, depletion of the body due to serious illnesses, surgical interventions, burn disease, and a decrease in the body's immunological reactivity.
Prevention of microflora
In order to be in good shape, a person needs to maintain a balance of microflora that supports his immune system. Thus, we help the body resist stress and cope with pathogenic microbes on its own. That is why the microflora must be taken care of daily. This should become as common as brushing your teeth in the morning or taking vitamins.
Prevention of violations of microflora is aimed at maintaining beneficial bacteria in the body. This is facilitated by eating foods rich in plant fiber (vegetables, fruits, cereals, wholemeal bread), as well as fermented milk products.
Today, on TV screens, we are offered to start the day with a “sip of health”: kefirs and yogurts enriched with bifidobacteria. However, it must be remembered that the amount of these beneficial elements in products with a long shelf life is quite small in order to stimulate the growth of microflora. Therefore, as a preventive measure, it is worth considering fermented milk products (kefirs, tans, etc.), which contain truly “live cultures”. As a rule, these products are sold in pharmacy chains and their shelf life is limited. And, of course, do not forget about the rules of healthy eating, sports and mental balance - all this helps to maintain immunity at its best!
Walnuts have anticancer properties
Novosibirsk doctors will treat with a transplant of donor feces
- Main page
- About health
- Healthy lifestyle
- beauty and health
- Intestinal microflora
The information presented on the site is offered for review and cannot serve as a substitute for an in-person consultation with a doctor! This resource may contain materials 18+
Normal intestinal microflora
Human evolution proceeded with constant and direct contact with the world of microbes, as a result of which close relationships were formed between macro- and microorganism, characterized by a certain physiological necessity.
The settlement (colonization) of body cavities communicating with the external environment, as well as the skin, is one of the types of interaction of living beings in nature. The microflora is found in the gastrointestinal tract and genitourinary system, on the skin, mucous membranes of the eyes and respiratory tract.
The most important role is given to the intestinal microflora, since it occupies an area of about 2 (for comparison, the lungs are 80 m2, and the skin of the body is 2 m2). It is recognized that the ecological system of the gastrointestinal tract is one of the body's defense systems, and if it is violated in a qualitative and quantitative sense, it becomes a source (reservoir) of pathogens of infectious diseases, including those with an epidemic nature of distribution.
All microorganisms with which the human body interacts can be divided into 4 groups.
■ The first group includes microorganisms that are not capable of a long stay in the body, and therefore they are called transient.
Their discovery during the examination is random.
■ The second group - bacteria that are part of the obligate (most permanent) intestinal microflora and play an important role in activating the metabolic processes of the macroorganism and protecting it from infection. These include bifidobacteria, bacteroids, lactobacilli, E. coli, enterococci, catenobacteria. Changes in the stability of this composition, as a rule, lead to a violation of the state of health.
■ The third group - microorganisms, also found with sufficient constancy in healthy people and are in a certain state of equilibrium with the host organism. However, with a decrease in resistance, with a change in the composition of normal biocenoses, these opportunistic forms can aggravate the course of other diseases or act as an etiological factor themselves.
Of great importance is their specific gravity in the microbiocenosis and the ratio with microbes of the second group.
These include staphylococcus, yeast fungi, proteus, streptococci, klebsiella, citrobacter, pseudomonas and other microorganisms. Their specific gravity can be only less than 0.01-0.001% of the total number of microorganisms.
■ The fourth group consists of pathogens of infectious diseases.
The microflora of the gastrointestinal tract is represented by more than 400 species of microorganisms, more than 98% of which are obligate anaerobic bacteria. The distribution of microbes in the gastrointestinal tract is uneven: each of the departments has its own, relatively constant microflora. The species composition of the microflora of the oral cavity is represented by aerobic and anaerobic microorganisms.
In healthy people, as a rule, the same types of lactobadilli are found, as well as micrococci, diplococci, streptococci, spirilla, and protozoa. Saprophytic inhabitants of the oral cavity can be the cause of caries.
Table 41 Criteria for normal microflora
The stomach and small intestine contain relatively few microbes, which is explained by the bactericidal action of gastric juice and bile. However, in a number of cases, lactobacilli, acid-resistant yeast, streptococci are detected in healthy people. In pathological conditions of the digestive organs (chronic gastritis with secretory insufficiency, chronic enterocolitis, etc.), the upper sections of the small intestine are colonized by various microorganisms. At the same time, there is a violation of the absorption of fat, steatorrhea and megaloplastic anemia develop. The transition through the Bauginian valve into the large intestine is accompanied by significant quantitative and qualitative changes.
The total number of microorganisms is 1-5x10 microbes per 1 g of content.
In the microflora of the colon, anaerobic bacteria (bifidobacteria, bacteroids, various spore forms) account for more than 90% of the total number of microbes. Aerobic bacteria, represented by E. Coli, lactobacilli and others, average 1-4%, and staphylococcus, clostridia, Proteus and yeast-like fungi do not exceed 0.01-0.001%. In qualitative terms, the microflora of feces is similar to the microflora of the large intestine cavity. Their number is determined in 1 g of feces (see table 41).
Normal intestinal microflora undergoes changes depending on nutrition, age, living conditions and a number of other factors. Primary colonization by microbes of the intestinal tract of a child occurs during the process of birth with Doderlein sticks, belonging to the lactic flora. In the future, the nature of the microflora significantly depends on nutrition. For children who are breastfed from 6-7 days, bifidoflora is prevailing.
Bifidobacteria are contained in the amount of 0 per 1 g of feces and make up to 98% of the entire intestinal microflora. The development of bifidoflora is supported by lactose contained in breast milk, bifidus factor I and II. Bifidobacteria, lactobacilli are involved in the synthesis of vitamins (group B, PP, folic acid) and essential amino acids, promote the absorption of calcium, vitamin D, iron salts, inhibit the growth and reproduction of pathogenic and putrefactive microorganisms, regulate the motor-evacuation function of the colon, activate local protective bowel reactions. In children of the first year of life who are artificially fed, the content of bifidoflora drops to 106 or less; Escherichia, acidophilus bacilli, enterococci predominate. The frequent occurrence of intestinal disorders in such children is explained by the replacement of bifidoflora by other bacteria.
The microflora of toddlers is characterized by a high content of Escherichia coli, enterococci; aerobic flora is dominated by bifidobacteria.
In older children, the microflora in its composition approaches the microflora of adults.
Normal microflora is well adapted to the conditions of existence in the intestine and successfully competes with other bacteria coming from outside. The high antagonistic activity of bifido-, lactoflora and normal Escherichia coli is manifested in relation to pathogens of dysentery, typhoid fever, anthrax, diphtheria bacillus, vibrio cholerae, etc. Intestinal saprophytes produce a variety of bactericidal and bacteriostatic substances, including antibiotics.
Of great importance for the body is the immunizing property of normal microflora. Escherichia, along with enterococci and a number of other microorganisms, cause constant antigenic irritation of the local immunity system, maintaining it in a physiologically active state (Khazenson JI. B., 1982), which contributes to the synthesis of immunoglobulins that prevent pathogenic enterobacteria from penetrating into the mucous membrane.
Intestinal bacteria are directly involved in biochemical processes, the decomposition of bile acids and the formation of stercobilin, coprosterol, deoxycholic acid in the colon. All this has a positive effect on metabolism, peristalsis, the processes of absorption and formation of feces. When the normal microflora changes, the functional state of the large intestine is disturbed.
The intestinal microflora is in close connection with the macroorganism, performs an important non-specific protective function, helps to maintain the constancy of the biochemical and biological environment of the intestinal tract. At the same time, normal microflora is a highly sensitive indicator system that reacts with pronounced quantitative and qualitative shifts to changes in environmental conditions in its habitats, which is manifested by dysbacteriosis.
Causes of changes in the normal intestinal microflora
Normal intestinal microflora can only be in the normal physiological state of the body. With various adverse effects on the macroorganism, a decrease in its immunological status, pathological conditions and processes in the intestine, changes occur in the microflora of the gastrointestinal tract. They can be short-term and spontaneously disappear after the elimination of an external factor that causes adverse effects, or be more pronounced and persistent.
MICROFLORA GIT
MICROFLORA OF THE GASTROINTESTINAL TRACT
MAIN FUNCTIONS OF THE NORMAL MICROFLORA OF THE INTESTINAL TRACT
Normal microflora (normoflora) of the gastrointestinal tract is a necessary condition for the life of the body. The microflora of the gastrointestinal tract in the modern sense is considered as the human microbiome.
Normoflora (microflora in a normal state) or the Normal state of microflora (eubiosis) is a qualitative and quantitative ratio of various microbial populations of individual organs and systems that maintains the biochemical, metabolic and immunological balance necessary to maintain human health. The most important function of the microflora is its participation in the formation of the body's resistance to various diseases and the prevention of colonization of the human body by foreign microorganisms.
In any microbiocenosis, including intestinal, there are always permanently inhabiting species of microorganisms - 90% related to the so-called. obligate microflora (synonyms: main, autochthonous, indigenous, resident, obligatory microflora), which plays a leading role in maintaining the symbiotic relationship between the macroorganism and its microbiota, as well as in the regulation of intermicrobial relations, and there are also additional (concomitant or facultative microflora) - about 10% and transient (random species, allochthonous, residual microflora) - 0.01%
Those. the entire intestinal microflora is divided into:
- obligate- home or obligatory microflora, about 90% of the total number of microorganisms. The obligate microflora mainly includes anaerobic saccharolytic bacteria: bifidobacteria (Bifidobacterium), propionic acid bacteria (Propionibacterium), bacteroids (Bacteroides), lactobacilli (Lactobacillus);
- optional concomitant or additional microflora, accounts for about 10% of the total number of microorganisms. Optional representatives of the biocenosis: Escherichia (Escherichia coli), Enterococcus (Enterococcus), Fusobacteria (Fusobacterium), Peptostreptococcus (Peptostreptococcus), Clostridia (Clostridium) Eubacteria (Eubacterium) and others, of course, have a number of physiological functions that are important for the biotope and organism as a whole. However, their predominant part is represented by conditionally pathogenic species, which, with a pathological increase in populations, can cause serious complications of an infectious nature.
- residual - transient microflora or random microorganisms, less than 1% of the total number of microorganisms. The residual microflora is represented by various saprophytes (staphylococci, bacilli, yeast fungi) and other opportunistic representatives of enterobacteria, which include intestinal: Klebsiella, Proteus, Citrobacter, Enterobacter, etc. Transient microflora (Citrobacter, Enterobacter, Proteus, Klebsiella, Morganella, Serratia, Hafnia, Kluyvera, Staphylococcus, Pseudomonas, Bacillus, yeast and yeast-like fungi, etc.), mainly consists of individuals brought from outside. Among them, there may be variants with a high aggressive potential, which, when the protective functions of the obligate microflora are weakened, can increase populations and cause the development of pathological processes.
There is little microflora in the stomach, much more in the small intestine and especially in the large intestine. It should be noted that the absorption of fat-soluble substances, the most important vitamins and trace elements occurs mainly in the jejunum. Therefore, the systematic inclusion in the diet of probiotic products and dietary supplements that contain microorganisms that regulate the processes of intestinal absorption becomes a very effective tool in the prevention and treatment of alimentary diseases.
Intestinal absorption is the process of entry of various compounds through a layer of cells into the blood and lymph, as a result of which the body receives all the substances it needs.
The most intensive absorption occurs in the small intestine. Due to the fact that small arteries branching into capillaries penetrate into each intestinal villus, the absorbed nutrients easily penetrate into the liquid media of the body. Glucose and proteins broken down to amino acids are absorbed into the blood only moderately. Blood carrying glucose and amino acids is sent to the liver where carbohydrates are deposited. Fatty acids and glycerin - a product of the processing of fats under the influence of bile - are absorbed into the lymph and from there enter the circulatory system.
In the figure on the left (diagram of the structure of the villi of the small intestine): 1 - cylindrical epithelium, 2 - central lymphatic vessel, 3 - capillary network, 4 - mucous membrane, 5 - submucosal membrane, 6 - muscular plate of the mucous membrane, 7 - intestinal gland, 8 - lymphatic channel.
One of the values of the microflora of the large intestine is that it is involved in the final decomposition of undigested food residues. In the large intestine, digestion ends with the hydrolysis of undigested food residues. During hydrolysis in the large intestine, enzymes that come from the small intestine and enzymes from intestinal bacteria are involved. There is an absorption of water, mineral salts (electrolytes), the breakdown of plant fiber, the formation of feces.
Microflora plays a significant (!) role in peristalsis, secretion, absorption and cellular composition of the intestine. The microflora is involved in the decomposition of enzymes and other biologically active substances. Normal microflora provides colonization resistance - protection of the intestinal mucosa from pathogenic bacteria, suppressing pathogenic microorganisms and preventing infection of the body. Bacterial enzymes break down fiber fibers that are not digested in the small intestine. The intestinal flora synthesizes vitamin K and B vitamins, a number of essential amino acids and enzymes necessary for the body. With the participation of microflora in the body, the metabolism of proteins, fats, carbons, bile and fatty acids, cholesterol occurs, procarcinogens (substances that can cause cancer) are inactivated, excess food is utilized and feces are formed. The role of normoflora is extremely important for the host organism, which is why its violation (dysbacteriosis) and the development of dysbiosis in general leads to serious metabolic and immunological diseases.
The composition of microorganisms in certain parts of the intestine depends on many factors: lifestyle, nutrition, viral and bacterial infections, as well as drug treatment, especially antibiotics. Many diseases of the gastrointestinal tract, including inflammatory diseases, can also disrupt the intestinal ecosystem. The result of this imbalance is common digestive problems: bloating, indigestion, constipation or diarrhea, etc.
The intestinal microflora is an extraordinarily complex ecosystem. One individual has at least 17 families of bacteria, 50 genera, species, and an indeterminate number of subspecies. The intestinal microflora is divided into obligate (microorganisms that are constantly part of the normal flora and play an important role in metabolism and anti-infective protection) and facultative (microorganisms that are often found in healthy people, but are conditionally pathogenic, i.e. capable of causing disease when reduced microorganism resistance). The dominant representatives of the obligate microflora are bifidobacteria.
Table 1 shows the most well-known functions of the intestinal microflora (microbiota), while its functionality is much wider and still being studied.
BARRIER ACTION AND IMMUNE PROTECTION
It is difficult to overestimate the importance of microflora for the body. Thanks to the achievements of modern science, it is known that the normal intestinal microflora takes part in the breakdown of proteins, fats and carbohydrates, creates conditions for the optimal flow of digestion and absorption in the intestine, takes part in the maturation of immune system cells, which enhances the protective properties of the body, etc. . The two main functions of the normal microflora are: barrier against pathogenic agents and stimulation of the immune response:
BARRIER ACTION. The intestinal microflora has a suppressive effect on the reproduction of pathogenic bacteria and thus prevents pathogenic infections.
The process of attachment of microorganisms to epithelial cells includes complex mechanisms. Bacteria of the intestinal microbiota inhibit or reduce adherence of pathogenic agents by competitive exclusion.
For example, bacteria of the parietal (mucosal) microflora occupy certain receptors on the surface of epithelial cells. Pathogenic bacteria that could bind to the same receptors are eliminated from the intestines. Thus, intestinal bacteria prevent the penetration of pathogenic and opportunistic microbes into the mucous membrane (in particular, propionic acid bacteria P. freudenreichii have fairly good adhesive properties and attach to intestinal cells very reliably, creating the mentioned protective barrier. Also, bacteria of a constant microflora help maintain intestinal motility and the integrity of the intestinal mucosa.So, b actors - commensals of the large intestine during the catabolism of indigestible carbohydrates in the small intestine (the so-called dietary fiber) form short-chain fatty acids ( SCFA, short-chain fatty acids), such as acetate, propionate and butyrate, which support the barrier functions of the mucus mucin layer (increase the production of mucins and the protective function of the epithelium).
IMMUNE SYSTEM OF THE INTESTINE. More than 70% of immune cells are concentrated in the human intestine. The main function of the intestinal immune system is to protect against the penetration of bacteria into the blood. The second function is the elimination of pathogens (pathogenic bacteria). This is provided by two mechanisms: innate (inherited by the child from the mother, people from birth have antibodies in the blood) and acquired immunity (appears after foreign proteins enter the blood, for example, after suffering an infectious disease).
Upon contact with pathogens, the body's immune defenses are stimulated. When interacting with Toll-like receptors, the synthesis of various types of cytokines is triggered. The intestinal microflora affects specific accumulations of lymphoid tissue. This stimulates the cellular and humoral immune response. Cells of the intestinal immune system actively produce secretory immunolobulin A (LgA) - a protein that is involved in local immunity and is the most important marker of the immune response.
ANTIBIOTIC-LIKE SUBSTANCES. Also, the intestinal microflora produces many antimicrobial substances that inhibit the reproduction and growth of pathogenic bacteria. With dysbiotic disorders in the intestine, there is not only an excessive growth of pathogenic microbes, but also a general decrease in the body's immune defenses. Normal intestinal microflora plays a particularly important role in the life of the body of newborns and children.
Thanks to the production of lysozyme, hydrogen peroxide, lactic, acetic, propionic, butyric and a number of other organic acids and metabolites that reduce the acidity (pH) of the environment, bacteria of normal microflora effectively fight pathogens. In this competitive struggle of microorganisms for survival, antibiotic-like substances such as bacteriocins and microcins occupy a leading place. Below in the figure Left: Colony of acidophilus bacillus (x 1100), Right: Destruction of Shigella flexneri (a) (Shigella Flexner - a type of bacteria that causes dysentery) under the action of bacteriocin-producing cells of acidophilus bacillus (x 60000)
HISTORY OF STUDYING THE COMPOSITION OF THE GIT MICROFLORA
The history of the study of the composition of the microflora of the gastrointestinal tract (GIT) began in 1681, when the Dutch researcher Anthony van Leeuwenhoek first reported his observations on bacteria and other microorganisms found in human feces and put forward a hypothesis about the coexistence of different types of bacteria in the gastrointestinal tract. -intestinal tract.
In 1850, Louis Pasteur developed the concept of the functional role of bacteria in the fermentation process, and the German physician Robert Koch continued research in this direction and created a technique for isolating pure cultures, which makes it possible to identify specific bacterial strains, which is necessary to distinguish between pathogenic and beneficial microorganisms.
In 1886, F. Esherich, one of the founders of the theory of intestinal infections, first described E. coli (Bacterium coli communae). Ilya Ilyich Mechnikov in 1888, working at the Louis Pasteur Institute, argued that a complex of microorganisms lives in the human intestine, which have an “autointoxication effect” on the body, believing that the introduction of “healthy” bacteria into the gastrointestinal tract can modify the action of the intestinal microflora and counteract intoxication . The practical implementation of Mechnikov's ideas was the use of acidophilic lactobacilli for therapeutic purposes, which began in the USA in 1920-1922. Domestic researchers began to study this issue only in the 50s of the XX century.
In 1955 Peretz L.G. showed that E. coli of healthy people is one of the main representatives of the normal microflora and plays a positive role due to its strong antagonistic properties against pathogenic microbes. Started more than 300 years ago, studies of the composition of the intestinal microbiocenosis, its normal and pathological physiology, and the development of ways to positively influence the intestinal microflora continue to this day.
HUMAN AS A BACTERIA HABITAT
The main biotopes are: gastrointestinal tract (oral cavity, stomach, small intestine, large intestine), skin, respiratory tract, urogenital system. But the main interest for us here are the organs of the digestive system, because. the bulk of various microorganisms lives there.
The microflora of the gastrointestinal tract is the most representative, the mass of intestinal microflora in an adult is more than 2.5 kg, the number is up to CFU / g. It was previously believed that the microbiocenosis of the gastrointestinal tract includes 17 families, 45 genera, more than 500 species of microorganisms (the latest data is about 1500 species) are constantly being corrected.
Taking into account the new data obtained in the study of the microflora of various biotopes of the gastrointestinal tract using molecular genetic methods and the method of gas-liquid chromatography-mass spectrometry, the total genome of bacteria in the gastrointestinal tract has 400 thousand genes, which is 12 times the size of the human genome.
Parietal (mucosal) microflora of 400 different sections of the gastrointestinal tract, obtained during endoscopic examination of various sections of the intestines of volunteers, was analyzed for homology of the sequenced 16S rRNA genes.
As a result of the study, it was shown that the parietal and luminal microflora includes 395 phylogenetically isolated groups of microorganisms, of which 244 are absolutely new. At the same time, 80% of the new taxa identified in the molecular genetic study belong to non-culturable microorganisms. Most of the proposed new phylotypes of microorganisms are representatives of the genera Firmicutes and Bacteroides. The total number of species is close to 1500 and requires further clarification.
The gastrointestinal tract through the system of sphincters communicates with the external environment of the world around us and at the same time through the intestinal wall - with the internal environment of the body. Due to this feature, the gastrointestinal tract has created its own environment, which can be divided into two separate niches: chyme and mucous membrane. The human digestive system interacts with various bacteria, which can be referred to as "endotrophic microflora of the human intestinal biotope". Human endotrophic microflora is divided into three main groups. The first group includes eubiotic indigenous or eubiotic transient microflora useful for humans; to the second - neutral microorganisms, constantly or periodically sown from the intestine, but not affecting human life; to the third - pathogenic or potentially pathogenic bacteria ("aggressive populations").
Cavity and wall microbiotopes of the gastrointestinal tract
In microecological terms, the gastrointestinal biotope can be divided into tiers (oral cavity, stomach, intestines) and microbiotopes (cavitary, parietal and epithelial).
The ability to apply in the parietal microbiotope, i.e. histadhesiveness (the ability to fix and colonize tissues) determines the essence of transient or indigenous bacteria. These signs, as well as belonging to a eubiotic or aggressive group, are the main criteria characterizing a microorganism interacting with the gastrointestinal tract. Eubiotic bacteria are involved in the creation of colonization resistance of the body, which is a unique mechanism of the system of anti-infective barriers.
The cavity microbiotope throughout the gastrointestinal tract is heterogeneous, its properties are determined by the composition and quality of the contents of one or another tier. Tiers have their own anatomical and functional features, so their contents differ in composition of substances, consistency, pH, speed of movement, and other properties. These properties determine the qualitative and quantitative composition of cavity microbial populations adapted to them.
The parietal microbiotope is the most important structure that limits the internal environment of the body from the external one. It is represented by mucous overlays (mucous gel, mucin gel), glycocalyx located above the apical membrane of enterocytes and the surface of the apical membrane itself.
The parietal microbiotope is of the greatest (!) interest from the standpoint of bacteriology, since it is in it that interaction with bacteria that is beneficial or harmful to humans occurs - what we call symbiosis.
It should be noted that in the intestinal microflora there are 2 types of it:
- mucosal (M) flora - mucosal microflora interacts with the mucous membrane of the gastrointestinal tract, forming a microbial-tissue complex - microcolonies of bacteria and their metabolites, epithelial cells, goblet cell mucin, fibroblasts, immune cells of Peyer's plaques, phagocytes, leukocytes, lymphocytes, neuroendocrine cells;
- luminal (P) flora - luminal microflora is located in the lumen of the gastrointestinal tract, does not interact with the mucous membrane. The substrate for its life activity is indigestible dietary fiber, on which it is fixed.
To date, it is known that the microflora of the intestinal mucosa differs significantly from the microflora of the intestinal lumen and feces. Although every adult has a specific combination of predominant bacterial species in the gut, the composition of the microflora can change with lifestyle, diet, and age. A comparative study of the microflora in adults who are genetically related to one degree or another revealed that genetic factors influence the composition of the intestinal microflora more than nutrition.
The number of microorganisms of mucosal and luminal microflora in different parts of the digestive tract.
Note to the figure: FOG - fundus of the stomach, AOG - antrum of the stomach, duodenum - duodenum (
Normal gut microbes- These are colonies of bacteria that inhabit the lumen of the lower parts of the digestive tract and the surface of the mucous membrane. They are needed for high-quality digestion of chyme (food bolus), metabolism and activation of local protection against infectious pathogens, as well as toxic products.
Normal intestinal microflora- this is the balance of various microbes of the lower parts of the digestive system, that is, their quantitative and qualitative ratio necessary to maintain the biochemical, metabolic, immunological balance of the body and maintain human health.
- protective function. Normal microflora has a pronounced resistance against pathogenic and opportunistic microorganisms. Beneficial bacteria prevent the colonization of the intestines by other infectious pathogens that are not characteristic of it. In the event of a decrease in the amount of normal microflora, potentially dangerous microorganisms begin to multiply. Purulent-inflammatory processes develop, bacterial infection of the blood (septicemia) occurs. Therefore, it is important not to allow a decrease in the amount of normal microflora.
- digestive function. The intestinal microflora is involved in the fermentation of proteins, fats, high molecular weight carbohydrates. Beneficial bacteria destroy the main mass of fiber and chyme residues under the action of water, maintain the necessary level of acidity (pH) in the intestines. The microflora inactivates (alkaline phosphatase, enterokinase), participates in the formation of protein breakdown products (phenol, indole, skatole) and stimulates peristalsis. Also, the microorganisms of the digestive tract regulate the metabolism and bile acids. Contribute to the transformation of bilirubin (bile pigment) into stercobilin and urobilin. Beneficial bacteria play an important role in the final stages of cholesterol conversion. It produces coprosterol, which is not absorbed in the large intestine and is excreted in the feces. Normoflora is able to reduce the production of bile acids by the liver and control the normal level of cholesterol in the body.
- Synthetic (metabolic) function. Beneficial bacteria of the digestive tract produce vitamins (C, K, H, PP, E, group B) and essential amino acids. Intestinal microflora promotes better absorption of iron and calcium, and therefore prevents the development of diseases such as anemia and rickets. Due to the action of beneficial bacteria, there is an active absorption of vitamins (D 3 , B 12 and folic acid), which regulate the hematopoietic system. The metabolic function of the intestinal microflora is also manifested in their ability to synthesize antibiotic-like substances (acidophilus, lactocidin, colicin, and others) and biologically active compounds (histamine, dimethylamine, tyramine, etc.), which prevent the growth and reproduction of pathogenic microorganisms.
- detoxification function. This function is associated with the ability of the intestinal microflora to reduce the amount and remove dangerous toxic products with feces: salts of heavy metals, nitrites, mutagens, xenobiotics, and others. Harmful compounds do not linger in body tissues. Beneficial bacteria prevent their toxic effects.
- immune function. The normal flora of the intestine stimulates the synthesis of immunoglobulins - special proteins that increase the body's defenses against dangerous infections. Also, beneficial bacteria contribute to the maturation of a system of phagocytic cells (nonspecific immunity), capable of absorbing and destroying pathogenic microbes (see).

Members of the intestinal microflora
The entire intestinal microflora is divided into:
- normal (basic);
- conditionally pathogenic;
- pathogenic.
Among all representatives there are anaerobes and aerobes. Their difference from each other lies in the features of existence and life activity. Aerobes are microorganisms that can live and reproduce only in conditions of constant oxygen supply. Representatives of the other group are divided into 2 types: obligate (strict) and facultative (conditional) anaerobes. Both those and others receive energy for their existence in the absence of oxygen. For obligate anaerobes, it is destructive, but not for facultative ones, that is, microorganisms can exist in its presence.
Normal microorganisms
These include gram-positive (bifidobacteria, lactobacilli, eubacteria, peptostreptococci) and gram-negative (bacteroids, fusobacteria, veillonella) anaerobes. This name is associated with the name of the Danish bacteriologist - Gram. He developed a special method for staining smears using aniline dye, iodine and alcohol. Under microscopy, some of the bacteria have a blue-violet color and are Gram-positive. Other microorganisms are discolored. To better visualize these bacteria, a contrast dye (magenta) is used, which stains them pink. These are Gram-negative organisms.
All representatives of this group are strict anaerobes. They form the basis of the entire intestinal microflora (92-95%). Beneficial bacteria produce antibiotic-like substances that help to expel pathogens of dangerous infections from the habitat. Also, normal microorganisms create a zone of "acidification" (pH=4.0-5.0) inside the intestine and form a protective film on the surface of its mucous membrane. Thus, a barrier is formed that prevents the colonization of foreign bacteria that have entered from the outside. Beneficial microorganisms regulate the balance of opportunistic flora, preventing its excessive growth. Participate in the synthesis of vitamins.
These include gram-positive (clostridia, staphylococci, streptococci, bacilli) and gram-negative (escherichia - Escherichia coli and other members of the enterobacteria family: Proteus, Klebsiella, Enterobacter, Citrobacter, etc.) facultative anaerobes. 
These microorganisms are opportunistic pathogens. That is, with well-being in the body, their influence is only positive, as in normal microflora. The impact of adverse factors leads to their excessive reproduction and transformation into pathogens. It develops with diarrhea, a change in the nature of the stool (liquid mixed with mucus, blood or pus) and a deterioration in general well-being. The quantitative growth of opportunistic microflora can be associated with weakened immunity, inflammatory diseases of the digestive system, malnutrition and the use of drugs (antibiotics, hormones, cytostatics, analgesics and other drugs).
The main representative of enterobacteria is with typical biological properties. It is able to activate the synthesis of immunoglobulins. Specific proteins interact with pathogenic microorganisms from the Enterobacteriaceae family and prevent their penetration into the mucous membrane. In addition, E. coli produces substances - colicins with antibacterial activity. That is, normal Escherichia are able to inhibit the growth and reproduction of putrefactive and pathogenic microorganisms from the Enterobacteriaceae family - Escherichia coli with altered biological properties (hemolyzing strains), Klebsiella, Proteus and others. Escherichia are involved in the synthesis of vitamin K.
The conditionally pathogenic microflora also includes yeast-like fungi of the genus Candida. They are rarely found in healthy children and adults. Their detection in the feces, even in small quantities, should be accompanied by a clinical examination of the patient in order to exclude (excessive growth and reproduction of yeast-like fungi). This is especially true in young children and patients with reduced immunity.
pathogenic microorganisms
These are bacteria that enter the digestive tract from the outside and cause acute intestinal infections. Infection with pathogenic microorganisms can occur when eating contaminated food (vegetables, fruits, etc.) and water, in violation of the rules of personal hygiene and contact with the patient. Normally, they are not found in the intestine. These include pathogenic pathogens of dangerous infections - pseudotuberculosis and other diseases. The most common representatives of this group are shigella, salmonella, yersinia, etc. Some pathogens (Staphylococcus aureus, Pseudomonas aeruginosa, atypical E. coli) can occur among medical personnel (carriers of a pathogenic strain) and in hospitals. They cause serious nosocomial infections.
All pathogenic bacteria provoke the development of intestinal inflammation by type or with a disorder of the stool (diarrhea, mucus in the feces, blood, pus) and the development of intoxication of the body. Beneficial microflora is suppressed.
Bacteria content in the intestines
Beneficial bacteria
| Normal microorganisms | Children over 1 year old | adults | ||
|---|---|---|---|---|
| bifidobacteria | 10 9 –10 10 | 10 8 –10 10 | 10 10 –10 11 | 10 9 –10 10 |
| lactobacilli | 10 6 –10 7 | 10 7 –10 8 | 10 7 –10 8 | >10 9 |
| eubacteria | 10 6 –10 7 | >10 10 | 10 9 –10 10 | 10 9 –10 10 |
| Pepto-streptococci | <10 5 | >10 9 | 10 9 –10 10 | 10 9 –10 10 |
| Bacteroids | 10 7 –10 8 | 10 8 –10 9 | 10 9 –10 10 | 10 9 –10 10 |
| Fusobacteria | <10 6 | <10 6 | 10 8 –10 9 | 10 8 –10 9 |
| Waylonelles | <10 5 | >10 8 | 10 5 –10 6 | 10 5 –10 6 |
CFU/g is the number of colony forming units of microbes in 1 gram of feces.
Opportunistic bacteria
| Opportunistic pathogens | Children under 1 year of age are breastfed | Children under 1 year old on artificial feeding | Children over 1 year old | adults |
|---|---|---|---|---|
| Escherichia coli with typical properties | 10 7 –10 8 | 10 7 –10 8 | 10 7 –10 8 | 10 7 –10 8 |
| Clostridia | 10 5 –10 6 | 10 7 –10 8 | < =10 5 | 10 6 –10 7 |
| Staphylococci | 10 4 –10 5 | 10 4 –10 5 | <=10 4 | 10 3 –10 4 |
| streptococci | 10 6 –10 7 | 10 8 –10 9 | 10 7 –10 8 | 10 7 –10 8 |
| bacilli | 10 2 –10 3 | 10 8 –10 9 | <10 4 | <10 4 |
| Mushrooms of the genus Candida | missing | missing | <10 4 | <10 4 |
Beneficial gut bacteria
Gram-positive strict anaerobes:

Gram-negative strict anaerobes:
- Bacteroids- polymorphic (having a different size and shape) sticks. Together with bifidobacteria, they colonize the intestines of newborns by the 6-7th day of life. When breastfeeding, bacteroids are detected in 50% of children. With artificial nutrition, they are sown in most cases. Bacteroides are involved in digestion and the breakdown of bile acids.
- Fusobacteria- polymorphic rod-shaped microorganisms. Characteristic of the intestinal microflora of adults. Often they are sown from pathological material with purulent complications of various localization. Able to secrete leukotoxin (a biological substance with a toxic effect on leukocytes) and platelet aggregation factor, which is responsible for thromboembolism in severe septicemia.
- Waylonelles- coccal microorganisms. In children who are breastfed, they are detected in less than 50% of cases. In babies on artificial nutrition, mixtures are sown in high concentrations. Waylonellas are capable of large gas production. With their excessive reproduction, this distinctive feature can lead to dyspeptic disorders (flatulence, belching and diarrhea).
How to check the normal microflora?
 A bacteriological examination of feces should be carried out by inoculation on special nutrient media. The material is taken with a sterile spatula from the last portion of the feces. The required amount of feces is 20 grams. The material for research is placed in a sterile dish without preservatives. It is necessary to take into account the fact that anaerobic microorganisms must be reliably protected from the action of oxygen from the moment of fecal sampling to its inoculation. It is recommended to use test tubes filled with a special gas mixture (carbon dioxide (5%) + hydrogen (10%) + nitrogen (85%)) with a tightly ground lid. From the moment of material sampling to the beginning of bacteriological examination, no more than 2 hours should pass.
A bacteriological examination of feces should be carried out by inoculation on special nutrient media. The material is taken with a sterile spatula from the last portion of the feces. The required amount of feces is 20 grams. The material for research is placed in a sterile dish without preservatives. It is necessary to take into account the fact that anaerobic microorganisms must be reliably protected from the action of oxygen from the moment of fecal sampling to its inoculation. It is recommended to use test tubes filled with a special gas mixture (carbon dioxide (5%) + hydrogen (10%) + nitrogen (85%)) with a tightly ground lid. From the moment of material sampling to the beginning of bacteriological examination, no more than 2 hours should pass.
This analysis of feces allows you to detect a wide range of microorganisms, calculate their ratio and diagnose visible disorders - dysbacteriosis. Disturbances in the composition of the intestinal microflora are characterized by a decrease in the proportion of beneficial bacteria, an increase in the number of opportunistic flora with a change in its normal biological properties, as well as the appearance of pathogens.
Low content of normal microflora - what to do?
The imbalance of microorganisms is corrected with the help of special preparations:
- contribute to the colonization of the intestine by the main microflora due to the selective stimulation of the growth and metabolic activity of one or more groups of bacteria. These drugs are not medicines. These include undigested food ingredients that are a substrate for beneficial bacteria and are not affected by digestive enzymes. Preparations: “Hilak forte”, “Duphalak” (“Normaze”), “Calcium Pantothenate”, “Lysozyme” and others.
- – These are living microorganisms that normalize the balance of intestinal bacteria and compete with conditionally pathogenic flora. Beneficial effect on human health. They contain beneficial bifidobacteria, lactobacilli, lactic streptococcus, etc. Preparations: “Acilact”, “Linex”, “Bactisubtil”, “Enterol”, “Kolibacterin”, “Lactobacterin”, “Bifidumbacterin”, “Bifikol”, “Primadophilus " and others.
- Immunostimulating agents. They are used to maintain normal intestinal microbiocenosis and increase the body's defenses. Preparations: “KIP”, “Immunal”, “Echinacea”, etc.
- Drugs that regulate the transit of intestinal contents. Used to improve digestion and evacuation of food. Preparations:, vitamins, etc.
Thus, the normal microflora with its specific functions - protective, metabolic and immunostimulating - determines the microbial ecology of the digestive tract and is involved in maintaining the constancy of the internal environment of the body (homeostasis).
In the gastrointestinal – In the human intestinal tract, there are obligate (main microflora), facultative (conditionally pathogenic and saprophytic microflora) and transient microflora (microorganisms that accidentally enter the gastrointestinal tract).
In the esophagus and stomach, transient microflora is usually determined, which enters them with food or from the oral cavity. Despite the ingestion of a large number of microbes into the stomach, healthy people normally have a small amount of microorganisms in the stomach (less than 10 3 CFU / ml). This is due to the acidic pH of the contents of the stomach and the bactericidal properties of gastric juice, which reliably protects a person from the penetration of pathogenic and opportunistic bacteria into the intestines. Mostly acid-fast bacteria are found in gastric juice. – lactobacilli, yeast fungi. Some people have streptococci in it, S. ventriculus, B. subtilis, anaerobic Gram-positive cocci.
Veillonella anaerobes, bacteroids, peptococci are found in the thickness of the gastric mucosa.
In a study of healthy children aged 8 – For 15 years, staphylococci, streptococci, enterococci, corynebacteria, peptococci, lactobacilli and propionibacteria were detected in the mucous membrane of the antrum of the stomach. Microbiological examination of the contents of the stomach is carried out relatively rarely.
The number and composition of microbes in the small intestine varies depending on the section of the intestine. The total number of microbes in the small intestine is no more than 10 4 – 10 5 cfu/ml content. The low concentration of microbes is due to the action of bile, the presence of pancreatic enzymes, intestinal peristalsis, which ensures the rapid removal of microbes to the distal intestine; the production of immunoglobulins by mucosal cells, the state of the intestinal epithelium and mucus secreted by intestinal goblet cells containing microbial growth inhibitors. The microflora of the small intestine is represented mainly by gram-positive facultative – anaerobic and anaerobic bacteria (enterococci, lactobacilli, bifidobacteria), yeast-like fungi, less common bacteroids and veillonella, extremely rarely enterobacteria. After eating, the number of microbes in the small intestine may increase significantly, but then in a short time it quickly returns to its original level. In the lower parts of the small intestine (in the ileum), the number of microbes increases and can reach 10 7 CFU / ml of content.
In the large intestine, the gram-positive flora changes to gram-negative. The number of obligate anaerobes begins to exceed the number of facultative anaerobes. Representatives of microbes characteristic of the large intestine appear.
The growth and development of microbes in the large intestine is facilitated by the absence of digestive enzymes, the presence of a large amount of nutrients, the prolonged presence of food, the structural features of the mucous membrane and, in particular, the mucous overlays of the large intestine. They determine the organ tropism of some types of anaerobic bacteria, which, as a result of their vital activity, form products used by the facultative anaerobic flora, which in turn create conditions for the life of obligate anaerobes.
In the human large intestine there are more than 400 species of various microbes, and the number of anaerobes in 100 – 1000 times the number of facultative anaerobes. Obligate anaerobes make up 90-95% of the total composition. They are represented by bifidobacteria, lactobacilli, bacteroids, veillonella, peptostreptococci, clostridia and fusobacteria (Fig. 1)
Other microorganisms account for 0.1 – 0.01% is the residual microflora: enterobacteria (Proteus, Klebsiella, serrations), enterococci, staphylococci, streptococci, bacilli, yeast fungi (Fig. 3). Opportunistic amoebas, Trichomonas, some types of intestinal viruses can live in the intestines.
|
B |
In the human large intestine, M-mucosal microflora is isolated - microbes that live in the thickness of the mucous membrane. The number of microbes in the thickness of the mucosa is 10 8 CFU per gram of intestinal tissue. Some authors call the mucosal microflora – "bacterial sod".
Microbes that live in the human intestinal lumen are called P – microflora (luminal or cavitary). The number of microbes in human feces reaches 10 12 CFU / g. contents and makes up 1/3 of human fecal masses. Facultative anaerobes account for 5-10% of the microflora of the large intestine. It consists of: Escherichia coli and enterococci (Fig. 2)
The obligate permanent human intestinal microflora is represented mainly by bifidobacteria, lactobacilli, E. coli and enterococci. Facultative flora is less common, it is represented by other anaerobic and facultative – anaerobic bacteria.
Dysbacteriosis (dysbiosis, dysmicrobiocenosis) of the intestine – qualitative and quantitative changes in microflora. Dysbacteriosis is accompanied by a decrease in the obligate anaerobic flora (bifidobacteria and lactobacilli) and an increase in conditionally pathogenic microflora, which are normally absent or found in small quantities (staphylococci, pseudomonads, yeast-like fungi, proteas, etc.). The appearance of dysbacteriosis can lead to immunological disorders with the possible development of gastrointestinal disorders.
The development of dysbacteriosis in humans is facilitated by exogenous and endogenous factors: infectious diseases of the digestive system, diseases of the gastrointestinal tract, liver, oncological pathology, and allergic diseases. Changes in the microflora are facilitated by the use of antibiotics, hormones, immunosuppressants, cytostatics, psychotropic, laxative and contraceptive drugs, exposure to industrial poisons and pesticides. The composition of microflora is greatly influenced by the season of the year, human nutrition, stress, smoking, drug addiction, and alcoholism.
The appearance of dysbacteriosis in newborns may be due to bacterial vaginosis and mastitis in the mother, resuscitation, late breastfeeding, prolonged stay in the maternity hospital, immaturity of intestinal motor function, breast milk intolerance, and malabsorption syndrome.
In infancy, the development of dysbacteriosis is promoted by: early artificial feeding, frequent acute respiratory viral infections, rickets, anemia, malnutrition, allergic and neuropsychiatric diseases.