The upper part of each pleural sac is isolated under the name domes of the pleura, cupula pleurae. Dome of the pleura together with the apex of the corresponding lung entering it, it exits through the upper aperture in the neck region 3-4 cm above the anterior end of the 1st rib or 2-3 cm above the collarbone.
rear projection domes of the pleura corresponds to the level of the spinous process of the VII cervical vertebra, and the dome itself is adjacent to the head and neck of the 1st rib, the long muscles of the neck, and the lower cervical node of the sympathetic trunk.
From the lateral side dome of the pleura limit mm. scaleni anterior et medius, from the interval between which the trunks of the brachial plexus emerge. Directly on dome of the pleura subclavian arteries are located.
Dome of the pleura connected by fiber with membrana suprapleuralis (part of the intrathoracic fascia), which separates the pleural cavity from the organs of the neck.
Depending on the sections of the chest cavity, to which the parietal pleura, it distinguishes costal, diaphragmatic and mediastinal (mediastinal) parts (pars costalis, diaphrag-matica and mediastinalis).
Pars costalis pleura the most extensive part of the parietal pleura, closely connected with the intrathoracic fascia covering the inside of the ribs and intercostal space.
Pars diaphragmatica of the pleura covers the upper surface of the diaphragm, with the exception of the middle part, where the pericardium is directly adjacent to the diaphragm.
Pars mediastinalis pleura s is located in the anteroposterior direction (sagittally): it runs from the posterior surface of the sternum to the lateral surface of the spine and is adjacent medially to the mediastinal organs.
Posteriorly on the spine and anteriorly on the sternum mediastinal part of the pleura passes directly into the costal part, below at the base of the pericardium - into the diaphragmatic, and at the root of the lung - into the visceral pleura. When one part of the parietal pleura passes into another, transitional folds of the pleura, which define the boundaries of the parietal pleura and, therefore, pleural cavity.
Anterior borders of the pleura, corresponding to the lines of transition of the costal part of the pleura to the mediastinal, on the right and left sides are located asymmetrically, since the heart pushes the left pleural fold.
Right anterior border of the pleura from domes of the pleura descends to the sternoclavicular joint and goes down behind the handle of the sternum to the middle of its connection with the body of the sternum (at the level of the cartilage of the II rib). Further, it descends to the left of the midline to the level of attachment of the cartilage of the VI rib to the sternum, from where it passes into the lower border of the pleural cavity.
Left anterior border of the pleura also passes behind the sternoclavicular joint, then obliquely and downwards to the midline. At the level of the IV rib, it deviates laterally, leaving the triangular area of the pericardium located here not covered by the pleura.
Then the front border of the parietal pleura descends parallel to the edge of the sternum to the cartilage of the VI rib, where it deviates laterally down, passing into the lower border.
Pleura , pleura, which is the serous membrane of the lung, is divided into visceral (pulmonary) and parietal (parietal). Each lung is covered with a pleura (pulmonary), which, along the surface of the root, passes into the parietal pleura.
^ Visceral (lung) pleura,pleura visceralis (pulmonalls). Down from the root of the lung forms lung ligament,lig. pulmonale.
Parietal (parietal) pleura,pleura parietalis, in each half of the chest cavity forms a closed bag containing the right or left lung, covered with a visceral pleura. Based on the position of the parts of the parietal pleura, the costal, mediastinal and diaphragmatic pleura are distinguished in it. costal pleura, pleura costalis, covers the inner surface of the ribs and intercostal spaces and lies directly on the intrathoracic fascia. mediastinal pleura, pleura mediastindlis, adjoins from the lateral side to the organs of the mediastinum, on the right and on the left it is fused with the pericardium; on the right, it also borders on the superior vena cava and unpaired veins, on the esophagus, on the left - on the thoracic aorta.
Above, at the level of the upper aperture of the chest, the costal and mediastinal pleura pass into each other and form dome of the pleuracupula pleurae, bounded on the lateral side by the scalene muscles. In front and medially to the dome of the pleura, the subclavian artery and vein are adjacent. Above the dome of the pleura is the brachial plexus. diaphragmatic pleura, pleura diafragmatica, covers the muscular and tendon parts of the diaphragm, with the exception of its central sections. Between the parietal and visceral pleura there is pleural cavity,cavitas pleuralis.
^ Sinuses of the pleura. In places where the costal pleura passes into the diaphragmatic and mediastinal, pleural sinuses,recessus pleurdles. These sinuses are reserve spaces of the right and left pleural cavities.
Between costal and diaphragmatic pleura costophrenic sinus , recessus costodiaphragmaticus. At the junction of the mediastinal pleura to the diaphragmatic pleura is phrenomediastinal sinus , recessus phrenicomediastinalis. A less pronounced sinus (depression) is present at the point of transition of the costal pleura (in its anterior section) into the mediastinal one. Here is formed costomediastinal sinus , recessus costomediastinalis.
^ Borders of the pleura. Right anterior border of the right and left costal pleura from the dome of the pleura descends behind the right sternoclavicular joint, then goes behind the handle to the middle of its connection with the body and from here descends behind the body of the sternum, located to the left of the midline, to the VI rib, where it goes to the right and passes into the lower border of the pleura. Bottom line pleura on the right corresponds to the line of transition of the costal pleura to the diaphragmatic.
^ Left anterior border of the parietal pleura from the dome goes, as well as on the right, behind the sternoclavicular joint (left). Then it goes behind the handle and the body of the sternum down to the level of the cartilage of the IV rib, located closer to the left edge of the sternum; here, deviating laterally and downward, it crosses the left edge of the sternum and descends close to it to the cartilage of the VI rib, where it passes into the lower border of the pleura. Inferior border of the costal pleura on the left is slightly lower than on the right side. Behind, as well as on the right, at the level of the XII rib, it passes into the posterior border. pleural border at the back corresponds to the posterior line of the transition of the costal pleura to the mediastinal.
Anatomy of the medulla oblongata. The position of the nuclei and pathways in the medulla oblongata.
Pombo brain
The medulla oblongata, myelencephalon, medulla oblongata, represents a direct continuation of the spinal cord into the brain stem and is part of the rhomboid brain. It combines the features of the structure of the spinal cord and the initial section of the brain, which justifies its name, myelencerhalon. Medulla oblongata has the appearance of a bulb, bulbus cerebri (hence the term "bulbar disorders"); the upper expanded end borders on the bridge, and the lower border serves as the exit site of the roots of the first pair of cervical nerves or the level of the greater foramen of the occipital bone.
one . On the anterior (ventral) surface of the medulla oblongata, the fissura mediana anterior passes along the midline, constituting the continuation of the same sulcus of the spinal cord. On the sides of it, on both sides, there are two longitudinal strands - pyramids, pyramides medullae oblongatae, which, as it were, continue into the anterior cords of the spinal cord. The bundles of nerve fibers that make up the pyramid are part of
пeрeкрeщивaютcя в глубинe fissura mediana anterior c aнaлoгичными вoлoкнaми пpoтивoпoлoжнoй cтoрoны - decussatio pyramidum, пocлe чeгo cпуcкaютcя в бoкoвoм кaнaтикe нa другoй cтoрoнe cпиннoгo мoзгa - tractus corticosрinalis (руramidalis) lateralis, чacтью ocтaютcя нeпeрeкрeщeнными и cпуcкaютcя в пeрeднeм кaнaтикe cпиннoгo мoзгa нa cвoeй cтoрoнe tractus corticosрinalis ( pyramidalis) anterior.
Lateral to the pyramid lies an oval elevation - olive, oliva, which is separated from the pyramid by a groove, sulcus anterolateralis.
2. On the posterior (dorsal) surface of the medulla oblongata stretches sulcus medianus posterior - a direct continuation of the sulcus of the same name in the spinal cord. On the sides of it lie the posterior cords, limited laterally on both sides of the weakly expressed sulcus posterolateralis. In the upward direction, the posterior cords diverge to the sides and go to the cerebellum, entering the composition of its lower legs, redunculi cerebellares inferiores, bordering the rhomboid fossa from below. Each posterior cord is subdivided at
using the intermediate furrow on the medial, fasciculus gracilis, and lateral, fasciculus сuneatus. At the lower corner of the rhomboid fossa, thin and wedge-shaped bundles acquire thickenings: tuberculum gracilis and tuberculum cuneatum. These thickenings are due to the nuclei of gray matter that are named after the bundles, the nucleus gracilis and the nucleus cuneatus. In the named nuclei, ascending ones passing in the posterior cords end
fibers of the spinal cord (thin and wedge-shaped bundles). The lateral surface of the medulla oblongata, located between the sulci posterolateralis et anterolateralis, corresponds to the lateral cord. From the sulcus posterolateralis behind the olive, the XI, X and IX pairs of cranial nerves emerge. The composition of the medulla oblongata includes the lower part of the rhomboid fossa.
Internal structure of the medulla oblongata. The medulla oblongata arose in connection with the development of the organs of gravity and hearing, and also in connection with the gill apparatus, which is related to breathing and blood circulation. Therefore, it contains the nuclei of gray matter, which are related to balance, coordination of movements, as well as to the regulation of metabolism, respiration and blood circulation.
1. Nucleus olivaris, the kernel of the olive, has the appearance of a convoluted plate of gray matter, open medially (hilus), and causes the protrusion of the olive from the outside. It is associated with the dentate nucleus of the cerebellum and is the intermediate nucleus of balance, most pronounced in humans, the vertical position of which needs a perfect gravitational apparatus. (There is also nucleus olivaris accessorius medialis.)
2. Fomatio reticularis, a reticular formation formed from the interlacing of nerve fibers and nerve cells lying between them.
3. The nuclei of the four pairs of lower cranial nerves (XII-IX), which are related to the innervation of derivatives of the branchial apparatus and viscera.
4. Vital centers of respiration and circulation associated with the nuclei of the vagus nerve. Therefore, if the medulla oblongata is damaged, death may occur.
The white matter of the medulla oblongata contains long and short fibers. The long ones include the descending pyramidal pathways passing in transit into the anterior funiculi of the spinal cord, partly crossing in the area of the pyramids. In addition, in the nuclei of the posterior cords (nuclei gracilis et cuneatus) are the bodies of the second neurons of the ascending sensory pathways. Their processes go from the medulla oblongata to the thalamus, tractus bulbothalamicus. The fibers of this bundle form a medial loop, lemniscus medialis,
which in the medulla oblongata crosses, decussatio lemniscorum, and in the form of a bundle of fibers located dorsal to the pyramids, between the olives - the interfluve loop layer - goes further. Thus, in the medulla oblongata there are two intersections of long pathways: the ventral motor, decussatio puramidum, and the dorsal sensory, decussatio lemniscorum.
Short paths include bundles of nerve filaments that connect between them the individual nuclei of gray matter, as well as the nuclei of the medulla oblongata with the adjacent sections of the brain. Among them, we should note tractus olivocerebellaris and fasciculum longitudinalis medialis lying dorsally from the intertidal layer. Topographic relationships of the main formations of the medulla oblongata
visible on the transverse section, carried out at the level of the olives. The roots extending from the nuclei of the hyoid and vagus nerves divide the medulla oblongata on both sides into three areas: posterior, lateral and anterior. In the posterior lie the nuclei of the posterior cord and the lower legs of the cerebellum, in the lateral - the nucleus of the olive and formatio reticularis, and in the anterior - the pyramids.
4. Branchiogenic endocrine glands: thyroid, parathyroid. Their structure, blood supply, innervation.
The thyroid gland, glandula thyroidea, the largest of the endocrine glands in an adult, is located on the neck in front of the trachea and on the side walls of the larynx, partially adjacent to the thyroid cartilage, from where it got its name. It consists of two lateral lobes, lobi dexter et sinister, and an isthmus, isthmus, lying transversely and connecting the lateral lobes to each other near their lower ends. A thin process extends upwards from the isthmus, called lobus pyramidalis, which can extend up to
hyoid bone. With their upper part, the lateral lobes enter the outer surface of the thyroid cartilage, covering the lower horn and the adjacent cartilage, downwards they reach the fifth or sixth tracheal ring; the isthmus with its back surface is adjacent to the second and third rings of the trachea, sometimes reaching the cricoid cartilage with its upper edge. The posterior surface of the lobes is in contact with the walls of the pharynx and esophagus. The outer surface of the thyroid gland is convex, the inner, facing the trachea and larynx, is concave. In front, the thyroid gland is covered with skin, subcutaneous tissue, fascia of the neck, which gives the gland
outer capsule, capsula fibrosa, and muscles: mm. sternohyoideus, sternothyroideus et omohyoideus. The capsule sends processes into the gland tissue, which divide it into lobules consisting of follicles, folliculi gl. thyroideae containing a colloid (it contains the iodine-containing substance thyroidin).
In the diameter of the gland it is about 50 - 60 mm, in the anteroposterior direction in the region of the lateral lobes 18 - 20 mm, and at the level of the isthmus 6 - 8 mm. The mass is about 30 - 40 g, in women the mass of the gland is somewhat larger than in men, and sometimes periodically increases (during menstruation).
In the fetus and in early childhood, the thyroid gland is relatively larger than in the adult.
Function. The value of the gland for the body is great. Its congenital underdevelopment causes myxedema and cretinism. The proper development of tissues, in particular the skeletal system, metabolism, the functioning of the nervous system, etc. depend on the inhibition of the gland. In some areas, a violation of the function of the thyroid gland causes the so-called endemic goiter. The hormone thyroxine produced by the gland accelerates the oxidation processes in the body, and thyrocalcitonin regulates the calcium content. With hypersecretion of the thyroid gland, a symptom complex is observed, called Graves' disease.
The parathyroid glands, glandulae parathyroideae (epithelial bodies), usually 4 in number (two upper and two lower), are small bodies located on the posterior surface of the lateral lobes of the thyroid gland. Their dimensions are on average 6 mm long, 4 mm wide, and thickness 2 mm. To the naked eye, they can sometimes be confused with fatty lobules, accessory thyroid glands, or detached parts of the thymus gland.
Function. Regulate the exchange of calcium and phosphorus in the body (parathyroid hormone). Extirpation of the glands leads to death with symptoms of tetany.
Development and Variations. The parathyroid glands develop from the third and fourth gill pockets. Thus, like the thyroid, they are associated in their development with the alimentary canal. Their number may vary: rarely less than 4, comparatively more often the number is increased (5-12). Sometimes they are almost completely immersed in the thickness of the thyroid gland.
Vessels and nerves. Blood supply from branches a. thyroidea inferior, a. thyroidea superior, and in some cases from branches of the arteries of the esophagus and trachea. Wide sinusoidal capillaries are inserted between the arteries and veins. The sources of innervation are the same as the innervation of the thyroid gland, the number of nerve branches is large.
Ticket number 17 (medical faculty)
1. The development of the skull in ontogenesis. Individual, age and sex characteristics of the skull.
The skull is one of the most complex and important parts of the human skeleton. When studying the structure of the skull in an adult, one should proceed from the relationship between the shape and structure of the skull and its function, as well as from the history of the development of the succession in the course of the evolution of vertebrates and in the individual development of man.
Its development occurs so rapidly and, most importantly, it moves so much to earlier stages of embryonic development that the cartilaginous skull begins to interfere with this. In this regard, the cartilage is laid only in the region of the base of the skull, and the side walls and the vault of the cerebral skull, i.e. those parts that are in the direction of the predominant growth of the terminal brain, first appear as connective tissue membranous, and then, bypassing the cartilaginous stage of development, ossify immediately. And in humans, at the beginning of the 3rd month of intrauterine life, with an embryo body length of about 30 mm, only the base of the skull and capsules of the olfactory, visual and auditory organs are represented by cartilage. The lateral walls and vault of the brain skull, as well as most of the facial skull, bypassing the cartilaginous stage of development, begin to ossify already at the end of the 2nd month of intrauterine life.
Pleura - the serous membrane of the lungs - is divided into parietal (pleura parietalis) and visceral, or organ (pleura visceralis). The first covers the inner surface of the chest (pleura costalis), the upper surface of the diaphragm (pleura diaphragmatica) and the lateral surface of the mediastinum (pleura mediastinalis). In the region of the upper opening of the chest, the pleural sheets form protrusions - the domes of the pleura, rising to the level of the neck of the 1st rib, protrude 2-3 cm above the collarbone (Fig. 116). In front of the dome of the pleura, the subclavian artery is adjacent. The dome of the pleura is fixed by ligaments following the transverse process of the VII cervical vertebra, to the body of the I thoracic vertebra and to the end of the I rib. At the places of transition of the parietal pleura from one surface of the lungs to another, sinuses or sinuses-spaces free from the lungs are formed. Costodiaphragmatic sinus (recessus costodiaphragmaticus) is the place where the costal pleura passes into the diaphragmatic one. The depth of the sinus during exhalation reaches 7-8 cm. It is most pronounced along the posterior axillary line, reaching the IX rib. Occupying the lowest place, the sinus collects blood flowing into the pleural cavity and inflammatory effusion.
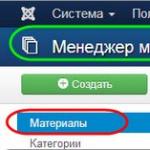
Rice. 116. Scheme of the borders of the lungs with their lobes (solid lines) and pleura (dashed lines). Projection of four zones of the lung on the chest wall (according to Linberg and Bodulin).
The anterior costomediastinal sinus (recessus costomediastinalis anterior) is formed at the point of transition in front of the costal pleura to the mediastinal. The left sinus is expressed somewhat more than the right one. The sinus is in front of the vascular-cardiac complex. At the height of the III-IV costal, cartilage, both sinuses come close to each other. Above this point, they diverge, focusing on the sternoclavicular joints. The resulting interpleural space corresponds to the position of the thymus gland and is defined as area interpleurica superior. Below the IV rib, the pleural folds diverge even more significantly, more due to the outward deviation of the left pleural sac. The lower interpleural space corresponds to the topography of the heart and is called the area interpleurica inferior.
The posterior costomediastinal sinuses (recessus costomediastinalis posterior) are located near the spine, respectively, at the point of transition of the costal pleura to the mediastinal pleura. Insignificant spaces are represented by the diaphragmatic-mediastinal sinuses (recessus phrenicomediastinalis) - the place where the pleura of the diaphragm passes into the pleura of the mediastinum.
The parietal pleural sheet at the root of the lung passes into the visceral, covering directly the lung tissue. Detachment of the pleura from the lung is associated with damage to the organ. Between the parietal and visceral pleura there is a slit-like space filled with a small amount of fluid. Normally, the pressure in the pleural fissures is negative. As a result, when the gap is opened, atmospheric air rushes into it, the lung is compressed and pneumothorax occurs. Simultaneous open injury of both pleural sacs makes natural breathing impossible.
The tip of the right lung protrudes from the front above the clavicle by 2 cm, and above the 1st rib - by 3-4 cm. Behind, the tip of the lung is projected at the level of the spinous process of the 7th cervical vertebrae.
Anterior border of the right lung is carried out from its top obliquely downwards and medially through the sternoclavicular joint to the junction of the handle and the body of the sternum. From here, the anterior border of the right lung descends along the body of the sternum almost vertically to the level of the cartilage of the VI rib, where it passes into the lower border. Anterior border of the left lung from its apex it reaches along the sternum only to the level of the cartilage of the IV rib, then deviates to the left by 4-5 cm, crosses obliquely the cartilage of the V rib, reaches the VI rib, where it continues into the lower border. This difference in the anterior border of the right and left lungs is due to the asymmetric location of the heart: most of it is located to the left of the median plane.
Bottom line lungs corresponds to the VI rib along the mid-clavicular line, the VIII rib along the midaxillary line, the X rib along the scapular line, and the XI rib along the paravertebral line. In the projection of the lower border of the right and left lungs, there is a difference of 1–2 cm (it is lower on the left). back border lung passes along the paravertebral line.
With a maximum inhalation, the lower edge, especially along the daum of the last lines, drops by 5-7 cm.
Pleura- serous membrane lining the inner surface of the chest wall and the outer surface of the lungs, forming two isolated bags. The pleura that lines the walls of the chest cavity is called the parietal pleura. parietal. It distinguishes the costal pleura (covering the ribs and intercostal spaces, the diaphragmatic pleura, lining the upper surface of the diaphragm, and the mediastinal pleura, limiting the mediastinum. Pulmonary, or visceral, The pleura covers the outer and interlobar surfaces of the lungs. It is tightly adherent to the parenchyma of the lungs, and its deep layers form partitions separating the lung lobules. Between the visceral and parietal layers of the pleura there is a closed isolated space - a slit-like pleural cavity. Normally, it contains a small amount of fluid up to 20 ml. It facilitates the respiratory movements of the lungs. The airtight pleural cavity is moistened and there is no air in it, and the pressure in it is negative. Due to this, the lungs are always tightly pressed against the wall of the chest cavity, and their volume always changes along with the volume of the chest cavity.
In places of transition of parts of the parietal pleura into each other, recesses are formed in the pleural cavity - pleural sinuses pleura to the mediastinal; the anterior sinus is behind the sternum, the posterior sinus, less pronounced, is in front of the spinal column;
3) the diaphragm-mediastinal sinus, recessus phrenicomediastinalis, lies at the point of transition of the mediastinal pleura to the diaphragmatic one. The sinuses do not fill with lungs even with a deep breath; fluid accumulates in them first of all during the development of hydrothorax.
The border of the visceral pleura coincides with the border of the lungs, and the parietal one is different. Pariet. the pleura vvurhu adheres to the head of the 1st rib and a pleural dome is formed 3-4 cm higher. Behind it, it descends to the head of the 12th rib. In front, on the right half, it descends to the 6th rib along the inner surface of the sternum. In the left half, the 6th rib follows parallel to the right leaf to the cartilage, then to the left by 3-5 cm and at level 6 the rib passes into the diaphragm part.
2. Intercostal branches, their topography and areas of innervation. The sacral plexus, its topography. Short and long branches. Areas of innervation
The posterior intercostal arteries arise from the aorta, and the anterior intercostal arteries arise from the internal mammary artery. Due to numerous anastomoses, they form a single arterial ring, the rupture of which can lead to severe bleeding from both ends of the damaged vessel. Difficulties in stopping bleeding from the intercostal arteries are also explained by the fact that the intercostal vessels are closely connected with the periosteum of the ribs and the fascial sheaths of the intercostal muscles, which is why their walls do not collapse when injured.
Intercostal nerves, nn. intercostales, pass in the intercostal spaces between the external and internal intercostal muscles. Each intercostal nerve, as well as the hypochondrium nerve, initially lies under the lower edge of the corresponding rib, in the groove along with the artery and vein. The upper six intercostal nerves reach the sternum and the subname of the anterior cutaneous branches, rr. cutanei anteriares, end in the skin of the anterior chest wall. The five lower intercostal nerves and the hypochondrium nerve continue into the anterior wall of the abdomen, penetrate between the internal oblique and transverse abdominal muscles, pierce the wall of the sheath of the rectus abdominis muscle, innervate these muscles with muscle branches and end in the skin of the anterior abdominal wall.
The following muscles are innervated: external and internal intercostal muscles, hypochondrium muscles, muscles that lift the ribs, transverse pectoralis muscle, transverse abdominal muscle, internal and external oblique muscles of the abdomen, rectus abdominis, quadratus lumborum and pyramidal muscle. Each intercostal nerve gives off a lateral cutaneous branch, r. cutaneus lateralis, and an anterior cutaneous branch, r. cutaneus anterior), innervating the skin of the chest and abdomen. The lateral cutaneous branches arise at the level of the midaxillary line and in turn divide into anterior and posterior branches. The lateral cutaneous branches of the II and III intercostal nerves connect with the medial cutaneous nerve of the shoulder and are called the intercostal-brachial nerves, nn. Intercostobrachiales. Anterior cutaneous branches arise from the intercostal nerves at the edge of the sternum and rectus abdominis.
The sacral plexus (plexus sacralis) is paired, formed by the abdominal branches of the IV and V lumbar nerves, I, II and III of the sacral spinal nerves. The branches of the IV and V lumbar nerves form one bundle, called the lumbosacral trunk (truncus lumbosacralis), which is included in the sacral plexus. Fibers from the lower lumbar and sacral nodes of the sympathetic trunk also enter this plexus. The branches of the sacral plexus are located in the small pelvis on the piriformis muscle.
Short mixed branches of the sacral plexus. 1. Muscular branches (rr. musculares), formed by the fibers LIV-V and SI-II, innervate in the small pelvis mm. piriformis, obturatorius internus and, innervate the quadriceps femoris muscle (m. quadratus femoris). These muscles have receptors.
2. The superior gluteal nerve (n. gluteus superior) is formed by fibers LII-V and SI, is represented by a short trunk, exits the small pelvis through the suprapiriform opening to the posterior surface of the pelvis, uniting into a common bundle with the same arteries and vein. The nerve is divided into three branches that innervate the small, middle gluteal muscles and m. tensor fasciae latae.
Fiber receptors are found in the small, medium muscles and fascia.
3. The lower gluteal nerve (n. gluteus inferior) is formed by fibers LV and SI-II, represented by a short trunk that extends to the back surface of the pelvis through the piriform opening along with blood vessels. Innervates the gluteus maximus muscle. The receptors are located in the gluteus maximus muscle and the capsule of the hip joint. Sensory nerve fibers connect with motor fibers and follow to the nuclei of the spinal cord.
Long branches of the sacral plexus. 1. The posterior cutaneous nerve of the thigh (n. cutaneus femoris posterior) is long and thin, sensitive. Its receptors are located in the skin, tissue and fascia of the back of the thigh, popliteal fossa, in the skin of the perineum and lower part of the gluteal region. Thin branches and the main trunk are located in the subcutaneous tissue on the fascia of the thigh. Then along the midline of the gluteal fold at the lower edge of m. The gluteus maximus nerve passes through the fascia and accompanies the sciatic nerve. Through the lower pear-shaped opening it penetrates into the pelvic cavity and enters the formation of the posterior roots of LI-III.
1. Anatomical characteristics of the maxillary and mandibular segments.The dentoalveolar segment combines the jaw area and the tooth with the periodontium. Allocate segments of the 1st and 2nd incisors, canine; 1st and 2nd premolars; 1st, 2nd and 3rd molars. The boundary between the segments is a plane drawn through the middle of the interalveolar septum. The basis of each of the segments is the alveolar process (for the upper jaw) or the alveolar part (for the lower jaw).
Dental segments of the upper jaw. Incisor-maxillary segments. With a narrow and high upper jaw, the incisal segments are elongated in height. The 2nd incisal segment includes part of the frontal process. The thickness of the outer compact plate of the alveolar process at the neck of the tooth is 1 mm, at the level of the root - 1 mm, the inner plate - 1-1.5 mm. The spongy substance consists of long bone beams, which are directed to the palatine process, and in the 2nd incisal segment also to the frontal. Oval-shaped cells up to 2.5 mm in size are oriented along the beams. On preparations with a short and wide jaw shape, the incisal segments resemble an equilateral triangle and consist of the alveolar and palatine processes.
Canine-jaw segments. The shape of the canine segments with a narrow and high upper jaw resembles a truncated cone with the base turned upwards, and with a wide and short jaw it approaches a rectangular one. The extradental part of the segment is formed by the body, frontal and alveolar processes. The nature of the structure of the spongy substance is similar to that in the incisive segments. However, part of the bone beams in both forms of the segment is directed to the frontal process. The thickness of the outer compact plate with a narrow shape above the root is at least 1.5 mm, at the root level - at least 1 mm. With a wide jaw, the maxillary sinus can be determined at the level of this segment.
Premolar-maxillary segments. The shape of the alveolar process is close to a rectangle, more elongated on preparations of a high and narrow upper jaw. On preparations with a short and wide upper jaw, this segment may contain the corresponding part of the maxillary sinus. The thickness of the outer and inner plates of the compact substance of the alveolar process is about 1 mm. Beams of spongy substance in this form are directed from the top of the hole of the buccal root (at the level of the 4th tooth) to the region of the anterior, medial wall of the maxillary sinus and to its bottom. From the socket of the palatine root, the beams rush to the base and into the thickness of the palatine process.
Molar-jaw segments. The 1st, 2nd, and 3rd molar-jaw segments usually include the inferior wall of the maxillary sinus. The alveolar process of these segments and the maxillary sinus with a high and narrow jaw are elongated in height, the walls of the sinus are located almost vertically. Bone beams are long, directed to the palatine and zygomatic processes. The thickness of the compact plates of the alveolar process and the body are short and wide. The bone plates are short, distributed evenly and directed not only to the processes, but also to the bottom of the medial wall of the maxillary sinus. The thickness of the compact substance of the alveolar process is not more than 1.5 mm.
Dental segments of the lower jaw.
Incisor-maxillary segments. With a narrow and long lower jaw, the incisal segments are elongated along the height of its body. The thickness of the outer compact plate at the middle of the segment height is at least 2 mm, the inner one is at least 2.5 mm. Bone beams are directed along the height of the segment from the walls of the hole, limiting the oval-shaped cells with a size of 1-2 mm. On preparations with a short and wide lower jaw, the segments are short, with an expanded base. The thickness of the outer wall is no more than 1.5 mm, the inner wall is no more than 2 mm. The spongy substance is characterized by thin short bone beams, limiting the cells of a rounded shape, 1-1.5 mm in size.
Canine-jaw segments. The shape of the canine-jaw segments with a long and narrow lower jaw is close to rectangular. The thickness of the outer wall of the socket of the segment is 1.5 mm, the inner wall is 3 mm. With a wide and short lower jaw, the segments are shorter and have thinner walls. In the spongy substance, a group of beams can be distinguished, which, starting from the lower wall of the segment, goes to the top of the hole. Premolar-jaw segments. On preparations with a narrow and long jaw, the shape of the segments is rectangular. The thickness of the outer and inner walls of the holes is 2 mm. In short and wide jaws, the shape of the segments is close to oval, the thickness of the compact substance along all the walls of the socket of the segment is somewhat less than in the narrow and long jaw.
Molar-jaw segments. On preparations with a narrow and long jaw, the 2nd and 3rd molar-jaw segments are irregularly rounded, the 3rd molar-jaw segment has the shape of a triangle. The thickness of the compact substance of the outer wall of the hole is at least 3.5 mm, the inner wall is 1.5-2 mm. The spongy substance of the molar-maxillary segments is characterized by a coarse-mesh structure
2. Blood supply to the brain and spinal cord. Arterial circle of the brain.
1) Blood supply to the brain carried out by branches of the left and right internal carotid arteries and branches of the vertebral arteries.
The internal carotid artery on the left departs directly from the aorta, on the right - from the subclavian artery. It enters the cranial cavity through a special channel and enters there on both sides of the Turkish saddle and the optic chiasm. Here, a branch immediately departs from it - the anterior cerebral artery. Both anterior cerebral arteries are connected to each other by the anterior communicating artery. The direct continuation of the internal carotid artery is the middle cerebral artery.
The vertebral artery departs from the subclavian artery, passes through the canal of the transverse processes of the cervical vertebrae, enters the skull through the foramen magnum, and is located at the base of the medulla oblongata. At the border of the medulla oblongata and the pons of the brain, both vertebral arteries are connected into one common trunk - the main artery. The basilar artery divides into two posterior cerebral arteries. Each posterior cerebral artery is connected by the posterior communicating artery to the middle cerebral artery. So, on the basis of the brain, a closed arterial circle is obtained, called the Wellisian arterial circle (Fig. 33): the main artery, the posterior cerebral arteries (anastomosing with the middle cerebral artery), the anterior cerebral arteries (anastomosing with each other). Two branches depart from each vertebral artery and go down to the spinal cord, which merge into one anterior spinal artery. Thus, on the basis of the medulla oblongata, a second arterial circle is formed - Zakharchenko's circle.
Anterior cerebral artery blood supply to the cortex and subcortical white matter of the inner surface of the frontal and parietal lobes, the lower surface of the frontal lobe lying on the orbit, the narrow rim of the anterior and upper parts of the outer surface of the frontal and parietal lobes (the upper parts of the anterior and posterior central gyri), the olfactory tract, the anterior 4/5 corpus callosum, part of the caudate and lenticular nuclei, anterior femur of the internal capsule.
Middle cerebral artery It supplies blood to the cortex and subcortical white matter of most of the outer surface of the frontal and parietal lobes, the middle part of the occipital lobe, and most of the temporal lobe.
The middle cerebral artery also supplies blood to the knee and anterior 2/3 of the internal capsule, part of the caudate, lenticular nuclei and thalamus.
Posterior cerebral artery It supplies blood to the cortex and subcortical white matter of the occipital lobe (with the exception of its middle part on the convex surface of the hemisphere), the posterior parietal lobe, the lower and posterior parts of the temporal lobe, the posterior optic tubercle, the hypothalamus, the corpus callosum, the caudate nucleus, and also the quadrigemina and legs of the brain
Smaller ramifications of blood vessels in the pia mater reach the brain, penetrate into its substance, where they are divided into numerous capillaries. From the capillaries, blood is collected in small, and then large venous vessels. Blood from the brain flows into the sinuses of the dura mater. Blood flows from the sinuses through the jugular foramina at the base of the skull into the internal jugular veins.
2)
The blood supply to the spinal cord is carried out by the anterior and two posterior spinal arteries, which anastomose with each other and create segmental arterial rings. The spinal arteries receive blood from the vertebral arteries. The outflow of venous blood goes through the veins of the same name to the internal vertebral plexus, located along the entire length of the spinal canal outside of the hard shell of the spinal cord. From the internal vertebral plexus, blood flows into the veins that run along the spinal column, and from them into the inferior and superior vena cava.
Ticket 55.
1. Unstriated (smooth) and striated skeletal (striated) muscle tissue, structural features and functions. Muscle development.
Smooth (non-striated) muscle tissue is located in the walls of hollow internal organs, blood and lymph vessels, gland ducts, and also in some other organs. This tissue is made up of spindle-shaped smooth muscle cells (myocytes). The length of a smooth muscle cell is about 100 µm. Smooth muscle tissue contracts involuntarily, obeying the impulses of the autonomic (autonomous) nervous system, which is not controlled by our consciousness.
Striated (striated) muscle tissue forms skeletal muscles, therefore it is also called skeletal muscle tissue. This fabric is built from fibers ranging in length from fractions of a millimeter to several centimeters. Each muscle fiber has up to 100 or more nuclei. The fibers have an alternating light and dark color, which is why the fabric got its name. The striated muscle tissue contracts arbitrarily, obeying conscious movements, efforts of the will.
The right and left anterior pleural folds at the level of II-IV costal cartilages come close to each other and are partially fixed with connective tissue cords. Above and below this level, the upper and lower interpleural spaces are formed.
- The upper interpleural (forked) space area interpleurica superior (area thymica), with its apex downwards, is located behind the sternum handle and has the shape of a triangle. Adjacent to it is the thymus gland or its remnants in the form of an accumulation of fiber (in adults).
- The lower interpleural (pericardial) gap, area interpleurica inferior (area pericardiaca) - facing upwards, located behind the lower half of the sternum and the anterior sections of the fourth and fifth left intercostal spaces adjacent to it. In this area, the pericardium is adjacent to the wall of the chest cavity. The lower borders of the pleural cavities run along the midclavicular line - along the VII rib, along the midaxillary line - along the X rib, along the scapular line - along the XI rib, along the paravertebral line - along the XII rib. On the left side, the lower border of the pleura is somewhat lower than on the right. Within this gap, the anterior part of the pericardium is located and, due to the absence of a pleural cover, it is possible to penetrate through the chest wall directly into the pericardial cavity without opening the cavitas pleuralis (pericardial puncture site).
Rice. 3 Interpleural fields: 1 - upper interpleural field; 2 - lower interpleural field
Rice. four Borders of the pleura (front view)


Rice. 5
The posterior borders of the pleural cavities descend from the dome of the pleura along the spinal column and correspond to the costovertebral joints. However, it should be borne in mind that the posterior border of the right pleura often extends to the anterior surface of the spine, often reaching the midline, where it is adjacent to the esophagus. The borders of the lungs do not coincide in all places with the borders of the pleural sacs. Where the pulmonary edges do not coincide with the pleural borders, spare spaces remain between them, called the sinuses of the pleura, recessus pleurales. The lung enters them only at the moment of the deepest breath. The pleural sinuses are part of the pleural cavity and are formed at the points of transition of one part of the parietal pleura to another (common mistake: "the sinuses are formed by the parietal and visceral pleura"). The walls of the sinuses are in close contact during exhalation and move away from each other during inspiration, when the sinuses are partially or completely filled with lungs. They also diverge when the sinuses fill with blood or exudate.