Content
According to the ICD, this term is characterized by diffuse inflammatory processes that occur in the bronchi. Chronic obstructive bronchitis can cause serious changes in the structure and functioning of the lungs. Therefore, it is extremely important to detect the disease in time and begin its treatment.
Causes of bronchial obstruction
Chronic obstructive bronchitis can occur as a result of exposure to the following factors:
- Respiratory hazard working conditions. These include working with varnishes and paints, building mixtures, chemicals and other toxic materials. The risk group includes miners, office workers, construction workers, workers in metallurgical plants and people living in large cities.
- Smoking. This bad habit provokes the deposition in the bronchi of a large amount of nicotine, tar and other combustion products.
- Upper respiratory tract infections. The resistance of the lungs and bronchi decreases under the influence of the virus.
- The predisposition is in the genetic code. This cause is characterized by a hereditary deficiency of the alpha1-antitrypsin protein, which performs protective functions in the lungs.
Symptoms of obstructive bronchitis
The main signs of chronic obstructive bronchitis:
- Cough. At the initial stages of the disease, it is dry, accompanied by a whistle. As the disease progresses, sputum develops. There may be traces of blood.
- Dyspnea. At first, this sign appears only during physical exertion, then shortness of breath is also noted in a calm state.
- fatigue. The patient feels tired very quickly, even if his load is minimal.
- Temperature. It does not rise because the reaction of the immune system does not work.

emphysematous type
An emphysematous type of the disease is found in the elderly. It is characterized by the appearance and progression of shortness of breath, which does not cause blue skin. It occurs under stress. Manifestations of the development of this type of chronic bronchitis is a small wet non-allergic cough, there is a decrease in body weight. In the later stages, pulmonary hypertension, hypoxemia, and left ventricular failure may occur. When diagnosing, specialists detect signs of emphysema on the lung.
Bronchitis type
A mild degree of shortness of breath suggests a bronchitis type of disease. At the same time, edema and cyanosis are observed in patients. This type of disease is characterized by a productive cough, wheezing or whistling sounds are found on examination. Chronic obstructive pulmonary disease of this type manifests itself at an early age, contributes to the development of hypoxia. On x-rays, patients can detect signs of fibrosis and an increase in the outlines of the lung pattern.
How to Diagnose Bronchitis
In the initial stages, the clinical picture of an obstructive type of disease does not have specific signs, so research will be aimed at excluding other diseases. To establish a diagnosis, the following procedures are carried out:
- sputum examination for bacterial content;
- inhalation procedures with beta2-adrenergic agonist to exclude asthmatic syndrome;
- radiography;
- examination of the respiratory function of the lungs;
- calculating a smoker's index;
- blood tests;
- bronchoscopy.

Carrying out FVD
The study of the function of external respiration is used to establish pathologies in the lungs and bronchi in case of suspected obstructive bronchitis. It is carried out on an empty stomach, and after the last meal, at least 2 hours should pass. Smoking patients are advised not to resort to a bad habit during the day before the FVD. In addition, you can not drink coffee and strong tea, drink alcoholic beverages. 30 minutes before the start of the study, you need to calm down, exclude physical activity. The FVD rules require the patient to wear something light.
During the procedure, the person should sit in a chair with their hands on the armrests. A special clamp is put on his nose, the patient breathes through his mouth into a special device - a spirometer. This device measures the volume of air that is released during inhalation and exhalation. First you need to take a deep breath. Then, gradually exhale all the air into the apparatus. The next action is similar, but is not performed calmly, but abruptly. At the last stage, you need to inhale as much as possible and exhale quickly. A decrease in indicators means the presence of obstructive bronchitis.
Chest x-ray and fluorography
No changes in the lungs on x-rays with obstructive disease in the initial stage will be detected. Fluorography is done to determine the progression of the disease, which is expressed in complications. In this case, the following indicators may be reflected in the images:
- greater severity of the lung pattern;
- changes in the roots of the lungs;
- signs of emphysema;
- hardening and thickening of smooth muscle.

Treatment of chronic obstructive bronchitis in adults
Various types of treatment are used to stop the symptoms and eliminate the causes of obstructive bronchitis. The basis of therapy is effective medications that should clear the airways of sputum and microbes. In addition to pills, patients with obstructive bronchitis rely on physiotherapy and special exercises, the implementation of which will help restore proper breathing.
Therapy with bronchodilators
To treat COPD, 2 types of bronchodilators are used:
- Bronchodilator drugs. These medications are mandatory. Among them are:
- Ipratropium bromide. The drug is used in the form of inhalations, which can be carried out using a spray can or nebulizer. Berodual combines this substance with beta2-agonists. Such funds are allowed for long-term use.
- Fenoterol (salbutamol, terbutaline) are used during an exacerbation of a chronic illness.
- Salmeterol (formoterol) - inhalations that have a prolonged action. They are prescribed for severe symptoms of obstructive disease.
- Doctors prescribe complex therapy with these drugs in case of a severe course of the disease, accompanied by inflammatory processes.
- Glucocorticoids. Medicines of this group are prescribed in the most serious cases of chronic bronchitis, if the drugs of the first type do not work. Inside it is prescribed to take a dose equal to 30 mg per day. The course of treatment is 1-1.5 weeks. If low efficiency is found, inhalations are prescribed.

The use of mucolytics
Expectorants are an important part of the treatment of chronic bronchitis. Their components reduce the viscosity of sputum, restore the ability of mucosal cells to regenerate. In addition, drugs help improve the effectiveness of other drugs. The most popular medicines of the group:
- Lazolvan;
- Bromhexine;
- Carbocysteine;
- Fluimucin.
Correction of respiratory failure
Treatment of chronic obstructive bronchitis in adults is carried out with the use of special breathing exercises and oxygen therapy. The latter type of recovery can be used both in a hospital and at home. Exercises for gymnastics with obstructive bronchitis are selected by the doctor individually for each patient. For home oxygen therapy procedures, non-invasive ventilation devices and oxygen concentrators are suitable.

Antibiotics
Indications for the use of antibiotics for the treatment of obstructive chronic bronchitis:
- secondary microbial infection;
- elderly age;
- severe course of the disease during an exacerbation;
- the appearance of pus among the sputum secreted when coughing;
- if the cause of the disease is a violation in the immune system.
The choice of an anti-inflammatory antimicrobial drug for chronic bronchitis should be carried out by a doctor, based on the testimony of tests and studies, individual characteristics of the body. If these measures have not been taken, broad-spectrum antibiotics are prescribed. These drugs include:
- Augmentin;
- Levofloxacin;
- Amoxiclav;
- Erythromycin.
Video
Did you find an error in the text?
Select it, press Ctrl + Enter and we'll fix it!
How to treat obstructive bronchitis and what is it?
Over time, inflammation in the bronchial wall progresses, bronchospasm and shortness of breath increase, obstructive syndrome and chronic impairment of pulmonary ventilation develop.
What it is?
Obstructive bronchitis is the occurrence of reflex spasms that prevent mucus from coming out. Obstruction may be intermittent, especially in the chronic form. The peculiarity of such bronchitis is that it is able to proceed latently.
Reasons for development
The disease in most cases becomes complicated by the continuation of respiratory viral infections, the influence of factors of external trouble: smoking, unfavorable environmental conditions, harmful production, poor living conditions.
Environmental factors:
- The presence of chemical irritants in the air at work or at home - inorganic and organic dust, acid fumes, ozone, chlorine, ammonia, silicon, cadmium, sulfur dioxide, etc. (see the impact of household chemicals on health).
- Prolonged exposure of the bronchial mucosa to physical irritants in the external environment - allergens, such as the pollen of some plants, house dust, animal hair, etc.
Socio-economic factors:
- alcohol abuse;
- Unfavorable living conditions;
- Smoking, passive smoking (see video of what cigarettes are made of);
- Elderly age.
Medical factors:
- Tumors of the trachea and bronchi;
- Airway hyperreactivity;
- genetic predisposition;
- Tendency to allergic reactions;
- Injuries and burns;
- poisoning;
- Infectious and inflammatory diseases of the respiratory system and impaired nasal breathing, foci of infection in the upper respiratory tract - bronchitis, pneumonia;
- Recurrent viral infections and diseases of the nasopharynx.
Chronic obstructive bronchitis
This is a progressive obstruction of the bronchi in response to various stimuli. Violation of bronchial patency is conventionally divided into: reversible and irreversible.
Signs with which patients usually go to the doctor:
- Violent cough, with scanty mucus in the morning
- Dyspnea, initially only on exertion
- Wheezing, labored breathing
- Sputum can acquire a purulent character during the period of accession of other infections and viruses and is regarded as a recurrence of obstructive bronchitis.
Over time, with an irreversible chronic process, the disease progresses, and the intervals between relapses become shorter.

Symptoms
The clinical picture of obstructive bronchitis is formed by the following symptoms:
- Cough - in the early stages, dry, without sputum, "whistling", mainly in the morning, and also at night, when the person is in a horizontal position. The symptom intensifies in the cold season. Over time, when coughing, sputum, clots appear, in older people there may be traces of blood in the separated secret;
- Difficulty breathing, or shortness of breath (after 7-10 years after the onset of cough) - first appears during physical exertion, then during the rest period;
- With exacerbation - fever, sweating, fatigue, headaches, muscle pain;
- Acrocyanosis - cyanosis of the lips, tip of the nose, fingers;
- Syndrome of "watch glasses", "Hippocratic nail" - deformation of the nail plates, when they become like watch glasses;
- The symptom of "drum sticks" is a characteristic change in the phalanges of the fingers;
- Emphysematous chest - the shoulder blades fit snugly against the chest, the epigastric angle is deployed, its value exceeds 90 °, "short neck", increased intercostal spaces.
It is important to remember that obstructive bronchitis does not make itself felt immediately. Symptoms usually appear when the disease is already in full swing in the body. As a rule, most patients seek help late, after the age of 40 years.
Diagnostics
The diagnosis is usually made on the basis of the patient's complaints, accompanying clinical history, lung auscultation, and heart rate.
The task of differential diagnosis is to exclude the development of such severe pathologies as pulmonary tuberculosis, pneumonia, a tumor of the lung tissue, developing heart failure due to a decrease in cardiac ejection fraction. If the patient has a decrease in cardiac output fraction, a strong incessant cough appears, a suspicion of alveolar edema (pulmonary edema) appears, then the actions of doctors should be lightning fast.
Obstructive bronchitis is characterized by the following:
- listening to percussion sound over the lungs;
- loss of mobility of the lung edge;
- hard breathing;
- on inspiration, wheezing is auscultated;
- the appearance of moist rales with an exacerbation of the disease.
If the patient is a smoker, then the doctor needs to find out the total experience of a bad habit, calculate the index of the smoker. When classifying obstructive bronchitis at the developmental stage, the indicator of forced expiratory volume in 1 min (in the abbreviation FEV) is used in relation to the vital capacity of the lungs (in the abbr. VC). The following stages are distinguished:
- Stage I. FEV = 50% of the norm. At this stage, the patient almost does not know discomfort, and dispensary control in this situation is not needed.
- Stage II. OFI \u003d 34-40% of the norm. The patient is advised to visit a pulmonologist due to a pronounced deterioration in the quality of life.
- Stage III. FEV<33% от нормы. Этот этап заболевания предполагает стационарное либо амбулаторное лечение.
To exclude pneumonia, pulmonary tuberculosis, dilatation of the cardiac sections, a chest x-ray procedure is performed. As additional research methods, laboratory test data (blood, urine, scraping of mucus or sputum) is required. Accurate diagnosis will allow you to quickly identify the underlying disease, stop the symptoms of obstructive bronchitis, and exclude its recurrence in the future.
Complications
When an obstruction develops, the required amount of air stops flowing into the lungs. Inhalations become heavy, the diaphragm does not fully open. Also, we breathe in more than we breathe out.
Some part remains in the lungs and provokes pulmonary emphysema. In severe and chronic forms, pulmonary insufficiency may appear, and this is the reason for mortality. Untreated bronchitis almost always ends in pneumonia, which is much more problematic to treat.

How to treat obstructive bronchitis?
First of all, in the treatment of obstructive bronchitis in adults, it is important to minimize, if possible, completely eliminate contact with irritating factors that may be a prerequisite for the progression of the process in the bronchi and its exacerbations.
It is necessary to give up smoking and other bad habits, stop contact with allergens, which in some cases may require quite radical steps: a change of job or place of residence.
The next step should be treatment at home with effective modern means.
Medical treatment
With obstructive bronchitis, which is caused by a viral infection, antiviral drugs are prescribed:
- Rimantadine (Algirem, Orvirem) has an intense antiviral effect by blocking healthy body cells from viral penetration. The drug is prescribed 100 mg (1 tablet) 1-3 times a day for 3-4 days. Allergic reactions are rare.
- Inosine pranobex (Isoprinosine, Groprinosine) have antiviral (stimulate the death of viral cells) and immunomodulatory (strengthen the immune system) effect. The drugs are prescribed 1-2 tablets 3-4 times a day. The course of treatment is 7-10 days, but can be extended by 1 month according to indications. The drug is well tolerated and usually does not cause allergic reactions.
With obstructive bronchitis caused by a bacterial infection, antibacterial drugs are prescribed, with the help of which the disease can be cured after 5-10 days:
- Macrolides (Clarithromycin, Rovamycin) have a bactericidal effect. Assigned to 500 mg 1 time per day. The course of treatment is 5-7 days. The drug does not cause allergic manifestations;
- Protected penicillins (Augmentin, Flemoxin-solutab) have bacteriostatic (reduce the growth and division of bacterial cells) and bactericidal (promote the death of bacteria) action. The drug is prescribed in tablets of 625 mg 3 times a day or 1000 mg 2 times a day for 7-14 days. With caution, this group of drugs is given to patients with frequent allergic reactions;
- In extremely severe cases of the development of the disease, the drugs of choice are respiratory fluoroquinolones - levofloxacin (Loxof, Leflok) 500 mg 1 time per day or 500–1000 mg in a 100.0 ml vial intravenously drip 1 time per day. This drug may cause acute allergic reactions.
If a cough occurs - mucolytic drugs:
- Ambroxol (Lazolvan, Abrol) has an expectorant effect and stimulates the movement of ciliated epithelium in the bronchi, which contributes to better sputum excretion. It is prescribed 30 mg (1 tablet) 3 times a day or 75 ml (1 tablet) 1 time per day. The course of treatment is 10 days. The drug does not provoke allergic effects;
- Acetylcysteine (ACC) reduces the viscosity of sputum and thereby stimulates its better discharge. Assigned to 400 - 800 mg 1 - 2 times a day for 10 days. Allergic reactions in the form of a skin rash;
- Local anti-inflammatory drugs - Erespal, Inspiron eliminate mucus hyperproduction and reduce swelling of the mucous and submucosal layers of the bronchial tree. Assigned to 1 tablet 2 times a day. The course of treatment is 10 days. Special instructions: causes an increase in heart rate and interruptions in the work of the heart. Allergic reactions are rare.
At elevated body temperature, non-steroidal anti-inflammatory drugs are used - Nimesulide, Ibuprofen - have antipyretic, decongestant and analgesic effects. Assigned to 200 mg 1-2 times a day.
If shortness of breath occurs, the treatment of obstructive bronchitis is supplemented with bronchodilators in aerosols (Salmeterol, Berodual, Ventolin, Salbutamol), which have a bronchodilatory effect and contribute to a better discharge of sputum from the bronchi. 2 breaths are prescribed 3-6 times a day.

Inhalations
With exacerbation of obstructive chronic bronchitis, it is noted:
- increased shortness of breath with a change in the frequency of respiratory movements, the depth of inspiration;
- change in the nature of cough, sputum;
- tightness in the chest.
When these symptoms appear, indicating an exacerbation, bronchodilators of all three groups are prescribed in inhalations. You can read about the properties of these drugs in the article Bronchodilator drugs.
The main cause of obstruction in adults is bronchospasm. To eliminate it, they resort to drugs of short and long action. The drugs of choice for chronic obstructive bronchitis are Atrovent, Troventol, oxytorpium bromide. The effect of their use appears after 30 minutes, lasts up to 6 hours, 3-4 doses are made per day.
With the ineffectiveness of therapy additionally prescribed:
- adrenostimulants - Ventolin, Brikanil, Berotek in inhalations, Clenbuterol Sopharma tablets, Clenbuterol syrup;
- theophylline tablets - Teopek, Teotard.
In acute conditions, inhalations of combined preparations are prescribed that combine the action of a hormonal agent with a bronchodilator. Read more about inhalations for bronchitis in our article Inhalations for bronchitis with a nebulizer.

Physiotherapy
The patient's condition will improve physiotherapy. One of its means is massage (percussion, vibration, back muscles). Such manipulations help to relax the bronchi, eliminate secretions from the respiratory tract. Apply modulated currents, electrophoresis. The state of health is stabilized after sanatorium treatment in the southern resorts of Krasnodar and Primorsky Krai.
Nutrition and diet
The diet during an exacerbation of the disease is aimed at eliminating the edema of the bronchial tree, stimulating the immune system, and replenishing protein reserves. Food should be high-calorie, at least 3000 calories / day with a predominance of proteins.
Healthy foods:
- fruits with vitamin C: orange, lemon, raspberry, grapefruit;
- dairy products: cheese, milk, cottage cheese;
- foods containing magnesium: nuts, bananas, sesame seeds, pumpkin seeds, rye bread, buckwheat, olives, tomatoes;
- products with omega-3 acids: fish oil, cod liver;
- vitamins A and E: green peas, beans, spinach, peach, avocado, carrots.
At the time of treatment of relapse, it is necessary to reduce the consumption of sugar and salt, limit the intake of allergenic foods (tea, chocolate, coffee, cocoa). Spicy, spicy, smoked foods contribute to the development of bronchospasm, so they should also be excluded from the diet or eaten in small quantities.

Prevention
Prevention of obstructive bronchitis also involves:
- refusal of addiction - smoking;
- dust reduction at home by carrying out wet cleaning. You can replace pillows filled with feathers with hypoallergenic fillers. You can also remove carpets and soft toys, which are the first accumulators of dust particles;
- adherence to a hypoallergenic diet, during which all foods that can increase coughing attacks are excluded;
- taking vitamins of groups B and C to maintain immunity. For this purpose, you can use herbal teas, which also contribute to the removal of mucus from the bronchi;
- during the period of pollination of plants, you can organize a stay in a comfortable microclimate, where any allergens are excluded.
Patients with obstructive asthmatic bronchitis first of all need to carry out hardening procedures, perform therapeutic respiratory complexes.
Obstructive bronchitis is an inflammatory disease of the bronchial tree, which is characterized by the occurrence of an unproductive cough with sputum, shortness of breath and, in some cases, broncho-obstructive syndrome, which is similar in its etiology to bronchial asthma.

The figure shows a bronchus in obstructive bronchitis.
The disease is common throughout the world, but is more common in regions with a humid and cold climate, where the average annual temperature does not rise above 15–17 0 C. This temperature, in combination with high humidity, promotes the reproduction of viral agents and pathological microorganisms, which, getting upper respiratory tract, provoke the development of the pathological process.
The prognosis for the disease is uncertain.
When a diagnosis such as acute obstructive bronchitis is established, recovery occurs within 7-14 days.
When establishing a diagnosis such as chronic obstructive bronchitis, the prognosis is unfavorable because the disease is constantly progressing and is accompanied by a gradual increase in respiratory failure, which negatively affects the entire body.
What can cause a pathological process in the bronchial tree?

The structure of the bronchial tree is shown on the left in the figure.
A disease such as obstructive bronchitis can be caused by many reasons, among which the most significant are:
- Bacteria:
- Pneumococci;
- Staphylococci;
- Streptococci;
- Pseudomonas aeruginosa;
- Legionella.
- Viruses:
- Flu;
- Rhinoviruses;
- Adenoviruses;
- Herpes;
- Cytomegalovirus.
- The simplest microorganisms:
- Chlamydia;
- Proteus;
- Mycoplasmas.
The infection is transmitted by airborne droplets after contact with a sick person or a carrier of the infection.
With obstructive bronchitis, the etiology of which is a bacterial infection, a person is contagious 3-5 days after the onset of the disease.
With obstructive bronchitis, the cause of which is a viral infection, the patient is contagious 1-2 days after the onset of the disease.
In obstructive bronchitis caused by a protozoal infection, an affected person is contagious for 4 to 6 days after onset.
Predisposing factors to the development of pathology: 
- reduced immunity due to chronic diseases of internal organs, after operations, frequent viral infections, etc.;
- persons with impaired functioning of the thermoregulation center (when the body temperature is constantly higher than normal);
- persons diagnosed with HIV (human immunodeficiency virus) or AIDS (acquired immunodeficiency syndrome);
- smoking;
- alcoholism;
- addiction;
- living in dusty and gassed areas or regions;
- labor that is associated with the mining, metallurgical, woodworking, pulp and paper or chemical industries.
The pathogenesis of obstruction in bronchitis (the mechanism of origin, development of the disease and its individual symptoms).
The pathogenesis is based on the summation of predisposing factors and causes of obstructive bronchitis, which lead to the development of an inflammatory process, which gradually involves bronchi of medium and small caliber. There are 4 components of pathogenesis:
- Violation of the movement of cilia of the ciliated epithelium of the bronchial mucosa, which helps to cleanse the bronchial tree.
- Replacement of the ciliated epithelium with goblet cells, which begin to produce a large amount of mucus.
- A decrease in bronchial secretions due to its amount of immune cells that fight infection that enters the bronchi with inhalation.
- Spasm of the smooth muscles of the bronchi.
Classification

On the left is a normal bronchus, on the right is an inflamed bronchus.
Establishing a diagnosis such as obstructive bronchitis involves determining the severity and stage of the process.
The severity of obstructive bronchitis, which is directly proportional to shortness of breath:
Grade 1 - shortness of breath begins to bother the patient with a long rise or with a fairly fast walk.
Grade 2 - shortness of breath begins to force the patient to move at a lower speed, in relation to healthy people.
Grade 3 - shortness of breath forces the patient to stop when walking slowly every 80–100 m.
Grade 4 - shortness of breath occurs when talking, eating, turning in bed.
The stages of the disease, which are determined depending on the results of spirometry (measurement of speed and volume indicators of breathing) and the main symptoms of the disease:
| Components (indicators) | Stage I - easy | Stage II - moderate | Stage III - severe | Stage IV - extremely severe |
|---|---|---|---|---|
| Tiffno index | Less than 70% | Less than 70% | Less than 70% | Less than 70% |
| FEV1 | 80% | 80% | Less than 50% | Less than 30% |
| Temperature | Not | Not | There is | Might not be |
| Dyspnea | Not | It happens | There is | There is |
| Sputum | Not | Not | There is | Might not be |
| Cough | Not | There is | There is | There is |
Main symptoms
Obstructive bronchitis in adults occurs with alternating periods of exacerbation and remission.
The period of exacerbation of the disease (during this period, a sick person is contagious to others):
- Broncho-obstructive syndrome, which is manifested by obstruction of the bronchi:

- Symptoms of damage to other internal organs and systems directly related to bronchial obstruction:
- Headache;
- Dizziness;
- Nausea;
- Vomit;
- Violation of consciousness;
- Chills;
- Increased heart rate;
- Increase in blood pressure figures.
The period of remission of the disease is characterized by slight sweating, moderate shortness of breath and the presence of a wet cough only in the morning, after waking up.
There is a special form of the disease - often recurrent obstructive bronchitis, which is characterized by almost constant periods of exacerbation with the presence of short remissions. This form of the disease most often leads to complications.
Diagnostics
Establishing the diagnosis of obstructive bronchitis in doctors usually does not cause difficulties. You can seek primary care from a general practitioner, pulmonologist or family doctor.
A preliminary diagnosis is made on the basis of the collected symptoms of the patient, his complaints and examination, which includes percussion of the chest with the identification of a characteristic box sound and auscultation of the lungs, during which weakened breathing and many dry wheezing are heard.

Auscultation of the lungs
The final diagnosis is made after the delivery of laboratory tests and the passage of an instrumental examination, taking into account the identification of changes characteristic of obstructive bronchitis in them:
- Laboratory examination:

- Instrumental examination:
Spirometry is an examination of the volume and speed indicators of inhalation and exhalation using a device - a spirograph. The main criteria for assessing the severity of the disease are indicators such as:
- VC - vital capacity of the lungs;
- FEV1 - forced expiratory volume in 1 second;
- Tiffno index - the ratio of VC to FEV1;
- POS - peak space velocity.
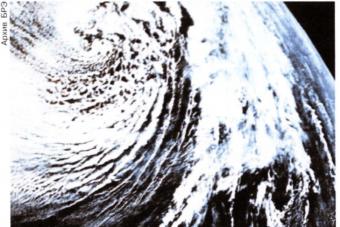
X-ray of the chest (thoracic organs), on which you can see dilated bronchi and a uniform increase in the airiness of the lung fields.
The differential diagnosis of obstructive bronchitis should be carried out after the main examination with a disease such as bronchial asthma. Since an asthma attack is very similar to obstructive bronchitis.
Differential diagnosis is carried out according to the following criteria:

Methods of modern therapy

- Antibacterial drugs:
- Macrolides (Azithromycin, Erythromycin, Rovamycin, Clarithromycin) have a pronounced antibacterial and bacteriostatic (inhibit the processes of division and growth of a bacterial cell) action. This drug can also be used for infection with protozoa. It is prescribed 500 mg 1-2 times a day. The course of treatment is 3-7 days.
- 2nd generation cephalosporins (Norfloxacin, Ciprofloxacin, Cefuroxime) have bacteriostatic and antiprotozoal (effective against protozoan microorganisms) action. Taking the drug can give allergic complications in predisposed individuals. It is prescribed after meals, 1 tablet (200 mg) 2 times a day. The course of treatment is 7-14 days.


During treatment, it is necessary to observe bed rest, walking is strictly prohibited. Doses of drugs, frequency of administration and duration of administration are decided individually by your doctor.
Consequences
- Often recurrent obstructive bronchitis.
- Respiratory failure.
- Emphysema of the lungs.
- Frequent complications associated with the cardiovascular system: cor pulmonale, tricuspid valve insufficiency, pulmonary hypertension, circulatory failure.
Disease prevention
- Exclude communication with contagious people, especially in the autumn-winter period.
- Refusal of bad habits and, first of all, smoking.
- With an increase in body temperature and the appearance of symptoms of damage to the respiratory system and ENT organs, you should immediately consult a doctor and begin treatment.
- Being outdoors, walking in the forest, walking along the coast.
- Leisure.
- Balanced diet.
Video: Bronchitis, bronchitis in children, acute bronchitis in children
Content
This is an insidious form of inflammation of the bronchi. Obstructive bronchitis gives dangerous complications. It is important to identify and eliminate the pathological process in time, otherwise the disease will become a severe chronic illness that will have to be treated for the rest of your life.
What is obstructive bronchitis
It is known that obstruction is a narrowing of the lumen of the bronchi, which becomes an obstacle to the free flow of air into the lungs, the release of sputum. Is there a difference in the diagnoses of "acute bronchitis" and "acute obstructive bronchitis"? What these diseases have in common is the presence of an inflammatory process. The essential difference is that in the first case, the mucous membranes of the bronchi do not suffer, and in the second they are severely damaged.
What's happening? The walls of the bronchi swell, thicken. The lumen of the respiratory vessels is filled with sputum, which loses its bactericidal properties and becomes thick, viscous mucus, fertile for the propagation of infection. The bronchi are covered with spasms: they either sharply narrow, then return to their original state. However, as the disease progresses, the respiratory vessels lose their ability to expand.
This pathology manifests itself in acute and chronic forms. Acute obstructive process is characterized by the rapid development of inflammation of the bronchi. Adults suffer mainly from chronic bronchitis, which periodically worsens. This is its distinguishing feature. Obstructive pathology in acute form is typical for children. Infants, in which the respiratory system is still imperfect, suffer more often.

In children
The younger the child, the faster the inflammatory processes progress in the delicate, very sensitive bronchi. Types of disease in children:
- acute bronchitis, in which there is no decrease in the lumen of the respiratory vessels;
- acute obstructive bronchitis - inflammation with swelling, narrowing, spasms of the bronchi and excess mucus;
- bronchiolitis - a very serious disease of narrowed bronchioles, often affects babies up to 3 years of age, especially infants.
The disease in a child develops much more often if the state of his health predisposes to the development of this disease. High risk group:
- children with weak immunity;
- premature babies;
- passive smokers;
- babies with congenital pathologies.
In adults
Since this ailment in a chronic form complicates the life, as a rule, of the elderly, it proceeds more severely. Diseases of worn vessels and heart, age-related decrease in immunity affect. Inflammation of the bronchial tree can develop very sluggishly and manifest itself with erased symptoms, therefore it is often detected when the disease is severely advanced and difficult to treat.
Chronic obstructive process aggravates very easily. This traditionally occurs in the rainy autumn-winter period and cold spring. Activation of inflammation of the bronchi is often caused by hypothermia, SARS, influenza, inhalation of vapors of toxic substances. With an exacerbation of the disease, its symptoms become pronounced, and the course - rapid.

Why does bronchial obstruction occur?
The most common reasons:
- frequent viral infections;
- smoking;
- occupational diseases due to chemically contaminated working conditions;
- hereditary predisposition.
Children are also more likely to be affected by a viral infection than a bacterial one. In addition, today a rare baby does not suffer from allergies. This is a powerful factor that predisposes to irritation and inflammation of the bronchi. Respiratory vessels react to allergens with hyperreactivity - spasms, which are pathological failures in their physiological mechanism. The next stage is acute bronchitis in a child.
Symptoms of bronchitis in adults and children
The disease is manifested by bright signs. Symptoms of acute bronchitis in adults are:
- severe, debilitating cough, wheezing in the lungs;
- shortness of breath even with little physical effort;
- fast onset fatigue;
- rise in temperature.
In children with acute obstructive bronchitis, almost the same symptoms appear. Dry, incessant cough often worse at night. The child breathes noisily, wheezing. In babies, at the same time, the wings of the nose expand, the muscles of the neck tense, and the shoulders rise. In acute obstructive bronchitis, the vast majority of children suffer from shortness of breath. Weakness, fatigue, headaches are either absent or do not significantly affect the child's condition.

Treatment of obstructive bronchitis in children and adults
Young children are strictly prohibited from inhaling with essential oils, rubbing their chest or back with ointments, cough balms. Instead of benefit, it often brings great harm. The child is better to be hospitalized. In the hospital, complex drug therapy is prescribed, which includes:
- drugs that relieve spasms of the bronchi and expand them (No-shpa, Papaverine, Salbutamol);
- expectorants (Lazolvan, Doctor MOM, ACC);
- antibiotics (Erythromycin, Amoxiclav, Azithromycin) - in the presence of a bacterial infection;
- antihistamines (Loratadin, Erius), if the child is allergic;
- general strengthening preparations (vitamin-mineral complexes).
In addition, appointed:
- light vibration massage of the collar zone;
- physiotherapy procedures (electrophoresis, amplipulse);
- physiotherapy;
- hypoallergenic diet.
Treatment of obstructive bronchitis in adults leads to a complete recovery only when the acute disease has not yet had time to turn into a chronic form. Bed rest is required. Treatment pursues the main goal: to slow down the progression of the disease. For this, drugs of the same pharmacological groups are used in the form of tablets, injections and droppers, herbal decoctions according to traditional medicine recipes, inhalations, and massage. An extremely important condition for successful therapy is smoking cessation.

How is bronchial obstruction diagnosed?
The main methods for diagnosing pathology:
- chest x-ray;
- sputum culture;
- bronchoscopy;
- general, biochemical, immunological examination of blood.
What is dangerous bronchitis with obstruction
The consequence of the disease after discharge from the hospital is often a residual cough, which may not go away for a long time. Obstructive bronchitis is dangerous with severe complications. Among them:
- emphysema;
- bronchial asthma;
- the occurrence of a pulmonary (increased in size) heart;
- bronchiectasis;
- pulmonary hypertension.
- quit smoking;
- regularly walk in the fresh air;
- harden the body from colds;
- avoid dusty and chemically aggressive air environment;
- systematically carry out wet cleaning in the house;
- get vaccinated against the flu every year.
Video
Chronic obstructive bronchitis is a disease of the bronchi and lungs, characterized by a partially irreversible restriction of airflow in the bronchopulmonary system, which is constantly progressing. The main symptoms of this pathology in the lungs are shortness of breath and cough with viscous sputum.
Chronic obstructive bronchitis is common throughout the world and occurs on average in 250-330 persons per 100,000 population.
The lowest incidence of reported cases is less than 110 per 100,000 and covers countries such as Canada, Alaska, southwestern South America, France, Germany, Bulgaria, the Arabian Peninsula, Asian Russia and Japan.
The United States, Argentina, Uruguay, Brazil, Great Britain, Norway, Poland, the Czech Republic, Slovakia, and African countries are average in terms of the spread of the disease, where the incidence rate is 110-550 per 100,000 population.
The highest incidence of chronic obstructive bronchitis occurs in Europe (Ukraine, Belarus, Russia), Asia (China, Mongolia, Tibet, Nepal, India, Indonesia, Iran, Iraq), Australia, Oceania and is 550–1350 or more per 100,000 population.
More often people of middle and old age get sick, in men chronic obstructive bronchitis occurs 3-4 times more often than in women.
The prognosis for working capacity and life is unfavorable. As the pathological process progresses in the lungs, efficiency is gradually lost. Adequate, timely treatment started only for a short time stops the course of the disease. Death occurs from complications (cor pulmonale, emphysema, etc.).
Chronic obstructive bronchitis in adults occurs due to many negative effects on the lungs, both from the environment and directly from the body, and therefore the causes of the disease are conventionally divided into two groups:
- External factors:

High risk occupations: 
- mining industry;
- builders;
- miners;
- metallurgists;
- workers in the pulp and paper industry;
- railroad workers;
- pharmaceutical industry workers.
- Frequent SARS (acute respiratory viral infections);
- adenovirus infection;
- Chronic deficiency of vitamin C;
- Previously transferred mononucleosis.
- Internal factors:
- Hereditary predisposition, which is based on a deficiency of alpha1-antitrypsin - a substance that blocks enzymes that break down protein in the bronchial tree and thereby prevent the destruction of lung tissue;
- Prematurity - the lungs fully develop only by 38-39 weeks of pregnancy (9 months);
- HIV infection (human immunodeficiency virus);
- Bronchial asthma, which is accompanied by an increase in the level of class E immunoglobulin;
- Bronchial hyperreactivity is a persistent increase in the formation of mucus in the bronchial tree.
Disease classification
Severity based on symptoms: 
- 0 degree - no severity - shortness of breath occurs with an intense load on the body;
- 1 degree - mild severity - shortness of breath occurs when lifting or when walking relatively fast;
- Grade 2 - moderate severity - shortness of breath forces patients to move at a slower speed compared to healthy people of the same age group;
- Grade 3 - severe - shortness of breath requires patients to stop during normal walking every 100 m;
- Grade 4 - very severe - shortness of breath occurs when eating, changing clothes or turning in bed. Such patients do not leave the room.
The stages of the disease, depending on the study of the function of external respiration by spirometry - the measurement of volume and speed parameters of respiration. (This method will be described in detail in the section "Modern methods of examination", i.e. the diagnosis of the disease).
Stage I is easy.
- Tiffno index less than 70%;
- FEV 1 more than 80%;
- The absence of the main symptoms of the disease - sputum, shortness of breath and cough.
II stage - medium.
- Tiffno index less than 70%;
- FEV 1 less than 80%;
- The presence or absence of the main symptoms of the disease - sputum, shortness of breath and cough.
III stage - heavy.
- Tiffno index less than 70%;
- FEV 1 less than 50%;
Stage IV is extremely difficult.
- Tiffno index less than 70%;
- FEV 1 less than 30%;
- Chronic respiratory failure;
- The presence of the main symptoms of the disease - sputum, shortness of breath and cough.
Symptoms of the disease
 Chronic obstructive bronchitis occurs with a constant alternation of 2 phases of the disease - exacerbation and remission, depending on the phase, the symptoms also differ.
Chronic obstructive bronchitis occurs with a constant alternation of 2 phases of the disease - exacerbation and remission, depending on the phase, the symptoms also differ.
Signs in the period of exacerbation:
- slight increase in body temperature;
- general weakness;
- headaches;
- dizziness;
- nausea;
- aches, chills, increased sweating;
- decrease in working capacity;
- shortness of breath with minimal exertion;
- cough with the release of viscous purulent sputum (yellow).
Symptoms in remission:
- shortness of breath with increased exertion;
- cough, mainly in the morning, sputum is serous in nature (clear or white).
Concomitant symptoms of damage to other organs from oxygen starvation, resulting from damage to the bronchopulmonary system:
- Signs of damage to the cardiovascular system - an increase in blood pressure, an increase in heart rate, pain in the heart, a feeling of palpitations, cyanosis of the nose, lips, fingertips;
- Signs of damage to the urinary system - pain in the lumbar region, swelling of the lower extremities;
- Signs of damage to the central nervous system - impaired consciousness, shallow breathing, decreased memory and attention, impaired vision, hallucinations;
- Signs of damage to the digestive system - yellowness of the skin, lack of appetite, bloating, abdominal pain.
Modern methods of examination
 Adult patients with a disease such as chronic obstructive bronchitis are observed at the place of residence or work by a general practitioner. When contacting the clinic for diagnosis and treatment, they can be observed by local therapists, family doctors or pulmonologists. In case of inpatient treatment, they should be in specialized pulmonology departments.
Adult patients with a disease such as chronic obstructive bronchitis are observed at the place of residence or work by a general practitioner. When contacting the clinic for diagnosis and treatment, they can be observed by local therapists, family doctors or pulmonologists. In case of inpatient treatment, they should be in specialized pulmonology departments.
The algorithm for examining such patients:
- Diagnostic survey and collection of complaints;
- Diagnostic examination of the patient, including percussion (tapping) and auscultation (listening) of the chest.
With percussion, a box sound appears, which means increased airiness of the lungs.
On auscultation, hard breathing and dry, whistling or buzzing rales are observed.
- Diagnostic laboratory examination:
- Complete blood count, which will be characterized by an increase in leukocytes, a shift in the leukocyte formula to the left and an increase in ESR (erythrocyte sedimentation rate);
- General urinalysis, in which there will be an increase in squamous cells and leukocytes in the field of view, as well as the possible appearance of mucus and traces of protein;
- General sputum analysis, which will be characterized by the presence of a large number of neutrophils and leukocytes.
- Diagnostic instrumental examination:

The patient is asked to breathe into a tube connected to a computer program that immediately displays a graph of inhalation and exhalation. During the examination, the doctor gives commands to patients, which consist in changing the speed and depth of breathing.
The main indicators that can be determined using spirometry:
- VC (vital capacity) is the total amount of air inhaled and exhaled from the lungs during calm deep breathing;
- FVC (forced vital capacity) is the total amount of air inhaled and exhaled from the lungs during deep, rapid breathing;
- FEV 1 (forced expiratory volume in 1 second) - the volume of air during a sharp exhalation after a calm deep breath;
- Tiffno index - the ratio of FEV 1 to VC. This parameter is a diagnostic criterion for determining the severity of the disease;
- POS (Peak Volume Velocity) is the maximum airflow velocity achieved with a sudden exhalation after a deep inhalation.
- X-ray of the organs of the chest cavity, which is characterized by the presence of dilated bronchi and increased airiness of the lung tissue.
Main types of treatment
For a disease such as chronic obstructive bronchitis, treatment is prescribed only by qualified specialists in a hospital or outpatient setting. Therapy should be combined, i.e. medical treatment must necessarily be supplemented with physiotherapy, which includes aromatherapy, inhalations, massages, warming up and exercise therapy (therapeutic exercises).
Medical treatment

The main goals of treatment are to prevent frequent exacerbations of chronic obstructive bronchitis, alleviate the symptoms of the disease, improve exercise tolerance on the body and reduce mortality.
Bronchodilators - drugs that dilate the bronchi:
- M-cholinergic blockers (ipratropium bromide) - Atrovent, Ipravent have a bronchodilator effect by blocking m-cholinergic receptors in the smooth muscles of the bronchi. The drug is prescribed for adults in the form of an aerosol of 40 mcg (2 breaths) 4-6 times a day;
- Short-acting beta2-agonists (salbutamol) - Salbuvent, Volmas, Ventolin - have a bronchodilatory effect by stimulating beta2-adrenergic receptors, which are located in the bronchial wall. For adults, the drug is prescribed by inhalation, 2-4 mg (1-2 breaths) up to 6 times a day;
- Long-acting beta2-agonists (formoterol) - Atimos, Foradil have a pronounced bronchodilatory effect. Assigned to adults 2 breaths 2 times a day (morning and evening).
Glucocorticosteroids (hormonal drugs):

Combined preparations containing long-acting beta2-agonists and glucocorticosteroids:

Antibacterial drugs act on chronic foci of infection in the bronchi due to the accumulation of copious amounts of sputum, which serves as a nutrient medium for them. These drugs are prescribed only in the period of exacerbation of the disease.
- 2nd generation cephalosporins (cefuroxime, cefamandol);
- 3rd generation cephalosporins (cefotaxime, ceftriaxone);
- 2nd generation fluoroquinolones (ciprofloxacin, ofloxacin);
- Respiratory fluoroquinolones (levofloxacin);
- Aminoglycosides (amikacin).
Mucolytic drugs - drugs that stimulate the discharge of sputum from the bronchial tree:
- Bromhexine (Solvin, Bronchostop) has antitussive, mucolytic and expectorant effects. It is prescribed in tablets of 8-16 mg 3-4 times a day;
- Ambroxol (Abrol, Ambrotard) stimulates the thinning of sputum by lowering the viscosity, which contributes to its better excretion. It is prescribed 30 mg (1 tablet) 3 times a day;
- Acetylcysteine (ACC) has antitussive and mucolytic effects. It is prescribed 200-400 mg 2-3 times a day or 800 mg 1 time per day.
Physiotherapy treatment

Essential oils used in aromatherapy include:
- pine oil;
- eucalyptus;
- juniper;
- sandalwood;
- tea tree;
- bergamot.
Complications of the disease
- Emphysema is an increased airiness of the lung tissue, in which the elasticity of the bronchi is completely lost. With this complication, inhalation is easy, and in order to exhale it is necessary to make a significant effort;
- Pulmonary heart - in conditions of oxygen starvation of the body, the myocardium (heart muscle) begins to contract more intensively in order to improve the blood supply to the internal organs and deliver the necessary amount of oxygen. Over time, the myocardium wears out, the chambers of the heart increase, the muscle layer becomes thin, which leads to disruption of the heart;
- Pulmonary hypertension - an increase in pressure in the bronchi and alveoli due to the narrowing of blood vessels;
- Lungs' cancer.
Disease prevention
- giving up bad habits, and especially smoking;
- moving to ecologically clean areas of cities;
- the fight against occupational hazards or the transition to work that is not related to heavy industry in conditions of high dust content in the air;
- balanced diet;
- playing sports;
- timely diagnosis and treatment of diseases of the respiratory system;
- annual preventive examinations with mandatory FLG (fluorography).
Video: Program "Live healthy", topic: "COPD - chronic obstructive pulmonary disease"