Double-blind, placebo-controlled study
Clinical research- scientific research of the efficacy, safety and tolerability of medical products (including medicines) in humans. The standard for good clinical practice indicates that the term is fully synonymous with this term. clinical trial, which, however, is less preferable due to ethical considerations.
In healthcare clinical trials conducted in order to collect safety and efficacy data for new drugs or devices. Such trials are carried out only after satisfactory information on the quality of the product, on its preclinical safety, has been collected, and the relevant health authority / Ethics Committee of the country where the clinical trial is being carried out has given permission.
Depending on the type of product and its stage of development, researchers enroll healthy volunteers and / or patients initially in small pilot, “sighting” studies, followed by larger patient studies, often comparing this new product to prescribed treatments. As positive safety and efficacy data are collected, the number of patients typically increases. Clinical trials can range in size from a single center in one country to multicenter trials covering centers in many countries.
The need for clinical trials
Every new medical product (drug, device) must undergo clinical trials. Special attention was paid to clinical trials at the end of the 20th century, in connection with the development of the concept of evidence-based medicine.
Authorized control bodies
In most countries of the world, ministries of health have special departments responsible for checking the results of clinical trials carried out on new drugs and issuing approvals for the supply of a medical product (drug, apparatus) to a network of pharmacies.
IN USA
For example, in the United States, such a department is Food and Drug Administration (
In Russia
In Russia, the Federal Service for Surveillance in Healthcare and Social Development (Roszdravnadzor of the Russian Federation) oversees clinical trials conducted in Russia.
Since the beginning of the era of clinical trials (CI) in the early 1990s, the number of studies conducted in Russia has been steadily growing from year to year. This is especially evident in the example of international multicenter clinical trials (IMCTs), the number of which has grown almost fivefold over the past ten years, from 75 in 1997 to 369 in 2007. The share of IMCTs in the total CI in Russia is also growing - if ten years ago they were only 36%, then in 2007 their share increased to 66% of the total CI. This is an important positive indicator of the "health" of the market, reflecting the high degree of trust of foreign sponsors in Russia as an emerging CI market.
Data obtained from Russian research centers is certainly accepted by foreign regulatory authorities when registering new drugs. This applies to both the US Food and Drug Administration (FDA) and the European Agency for the Evaluation of Medicinal Products (EMEA). For example, six out of 19 new molecular substances approved by the FDA in 2007 underwent CT with the participation of Russian research centers.
Another important factor in the increase in the number of IMCTs in Russia is the growth of its commercial attractiveness for foreign sponsors. The growth rate of the retail commercial market in Russia is three to four times higher than the growth rate of the pharmaceutical markets in Europe or the United States. In 2007, the growth in Russia was 16.5%, and the absolute volume of sales of all pharmaceutical products reached 7.8 billion US dollars. This trend will continue in the future due to the effective demand of the population, which, according to the forecasts of specialists from the Ministry of Economy and Trade Development, will grow steadily over the next eight years. This suggests that if, through the joint efforts of market participants, Russia can approach the pan-European deadlines for obtaining CT approvals, then with its good patient enrollment and further stabilization of the political and regulatory climate, it will soon become one of the world's leading markets for clinical trials.
In 2007, Roszdravnadzor of the Russian Federation issued 563 permits for all types of clinical trials, which is 11% more than in 2006. The growth in indicators is mainly attributable to the increase in the number of international multicenter clinical trials (IMCTs) (by 14%) and locally conducted clinical trials (growth by 18% per year). According to the forecasts of Synergy Research Group, which conducts quarterly monitoring of the clinical trials market in Russia (Orange Book), in 2008 the number of new trials will fluctuate at 650, and by 2012 it will reach thousands of new clinical trials per year.
Control practice in other countries
Similar institutions exist in other countries.
International requirements
The basis for conducting clinical trials (trials) is the document of the international organization "International Conference on Harmonization" (ICH). This document is called the Guideline for Good Clinical Practice (GCP Standard Description; Good Clinical Practice translates to Good Clinical Practice).
Typically, in addition to physicians, there are other clinical research specialists working in the clinical research field.
Clinical research must be conducted in accordance with the fundamental ethical principles of the Declaration of Helsinki, the GCP standard and applicable regulatory requirements. Prior to the initiation of a clinical trial, an assessment should be made of the ratio of the foreseeable risk to the expected benefit to the subject and society. At the forefront is the principle of priority of the rights, safety and health of the subject over the interests of science and society. The subject can be included in the study only on the basis of voluntary informed consent(IS) obtained after a detailed acquaintance with the research materials. This consent is certified by the signature of the patient (subject, volunteer).
Clinical research should be scientifically based, detailed and clearly described in the research protocol. Assessment of the risk-benefit ratio, as well as review and approval of the study protocol and other documentation related to the conduct of clinical trials, are the responsibility of the Organization's Expert Council / Independent Ethics Committee (IRB / IEC). After obtaining approval from the ESP / IEC, the clinical trial can begin.
Types of clinical trials
Pilot the research is intended to obtain preliminary data that are important for planning further stages of the research (determining the feasibility of conducting the research in a larger number of subjects, the sample size in the future research, the required research power, etc.).
Randomized a clinical trial in which patients are randomly assigned to treatment groups (randomization procedure) and have the same opportunity to receive the investigational or control drug (comparator or placebo). In a nonrandomized study, the randomization procedure is not performed.
Controlled(sometimes used as a synonym "comparative") a clinical trial in which an investigational drug, the efficacy and safety of which has not yet been fully studied, is compared with a drug whose efficacy and safety are well known (comparator drug). This can be a placebo (placebo-controlled trial), standard therapy, or no treatment at all. In an uncontrolled (noncomparative) study, a control / comparison group (a group of subjects taking a comparison drug) is not used. In a broader sense, controlled research refers to any research in which potential sources of bias are controlled (if possible, minimized or excluded) (that is, it is conducted in strict accordance with the protocol, monitored, etc.).
When conducting parallel study subjects in different groups receive either only the study drug or only the comparison drug / placebo. V cross In studies, each patient receives both drugs being compared, as a rule, in a random sequence.
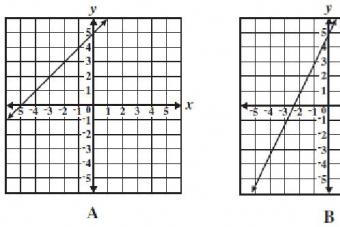
Research can be open when all study participants know which drug the patient is receiving, and blind(disguised) when one (single-blind study) or multiple parties to a study (double-blind, triple-blind, or full-blind study) are kept in the dark about the distribution of patients by treatment group.
Prospective the study is conducted by dividing participants into groups who will or will not receive the study drug before the outcome occurs. In contrast, a retrospective (historical) study examines the outcomes of previous clinical trials, that is, the outcomes occur before the study is started.
Depending on the number of research centers in which research is carried out in accordance with a single protocol, research is single-center and multicenter... If a study is conducted in several countries, it is called international.
V parallel A study compares two or more groups of subjects, one or more of whom are receiving the study drug and one group of which is the control group. Some parallel studies compare different treatments without including a control group. (This design is called independent group design.)
Cohort A study is an observational study in which a selected group of people (cohort) is observed over a period of time. The outcomes of subjects in different subgroups of a given cohort, those who have or have not (or have undergone to varying degrees) treatment with the study drug are compared. V prospective cohort study cohorts are composed in the present and observed in the future. In a retrospective (or historical) cohort study, cohorts are matched from archival records and their outcomes are traced from then to the present. Cohort trials are not used to test drugs, but rather to determine the risk of contributing factors that cannot be controlled or ethically controlled (smoking, being overweight, etc.).
In research case-control(synonym: study of similar cases) comparing people with a particular disease or outcomes ("case") with people in the same population who do not have the disease or who did not have the given outcome ("control"), in order to identify the relationship between the outcome and prior exposure to certain risks; factors. In a case series study, multiple individuals are observed, usually receiving the same treatment, without using a control group. In the description of the case (synonyms: case from practice, history of the disease, description of a single case), a study of treatment and outcome in one person is conducted.
Double-blind, randomized, placebo-controlled trial- a method of testing a medical product (or a treatment technique), in which the influence on the patient of both unknown factors and factors of psychological influence is taken into account and excluded from the results. The purpose of the test is to test the effect of only the drug (or technique) and nothing else.
When testing a medicinal product or method, experimenters usually do not have sufficient time and ability to reliably establish whether the method under test produces a sufficient effect, therefore, statistical methods are used in a limited clinical trial. Many diseases are very difficult to cure and doctors have to fight for every step towards recovery. Therefore, the test monitors the many symptoms of the disease and how they change when exposed.
A cruel joke can be played by the fact that many symptoms are not strictly associated with the disease. They are not unambiguous for different people and are influenced by the psyche of even an individual person: under the influence of the doctor's kind words and / or the doctor's confidence, the patient's degree of optimism, symptoms and well-being can improve, and objective indicators of immunity often increase. It is also possible that there will be no real improvement, but the subjective quality of life will increase. Symptoms may be influenced by unaccounted for factors, such as the patient's race, age, gender, etc., which will also indicate not the effect of the investigational drug, but something else.
To cut off these and other lubricating effects of the therapeutic method of effects, the following techniques are used:
- research is done placebo controlled... That is, patients are divided into two groups, one - the main one - receives the study drug, and the other, the control group, is given a placebo - a dummy.
- research is done blind(eng. single blind). That is, patients do not realize that some of them are receiving a placebo, not an investigational new drug. As a result, patients in the placebo group also think they are getting treatment, when in fact they are receiving a dummy. Therefore, the positive dynamics from the placebo effect took place in both groups and dropped out when compared.
V double blind In the (double blind) study, not only the patients, but also the doctors and nurses who give the drugs to the patients, and even the clinic's management, themselves do not know what they are giving them - whether it is really the study drug or a placebo. This eliminates the positive impact of confidence on the part of doctors, clinic management and nursing staff.
Ethical Issues and Clinical Research
Drug development and clinical trials are very expensive procedures. Some firms, in an effort to reduce the cost of testing, conduct them first in countries where the requirements and cost of testing are significantly lower than in the country of the company - the developer.
For example, many vaccines were initially tested in India, China and other third world countries. Charitable deliveries of vaccines to countries in Africa and Southeast Asia were also used as the second or third stage of clinical trials.
Randomized controlled clinical trials (RCTs), are carried out in hospitals, less often in other medical institutions in order to assess the potential effectiveness of means, methods and schemes of treatment, diagnostics, diseases.
When assessing the potential efficacy of a drug proposed for the treatment of a disease, the population includes patients with the same clinical course of this disease, comparatively the same sex and age, and other signs that may affect the outcome of the disease.
The sample is formed taking into account certain restrictions, while patients representing the population, are not included in the sample mainly for the following reasons:
non-compliance with selection criteria for factors that may affect the expected effect of experimental treatment;
refusal to participate in the experiment;
the alleged possibility of non-compliance by individuals with the conditions of the experiment (for example, irregular intake of the prescribed drug, violation of the rules of circulation, etc.);
contraindications to experimental treatment.
As a result of such selection, the formed sample may turn out to be small, which will affect the results of assessing the reliability of differences in the frequency of outcomes in the experimental and control groups. In addition, the sample formed can be dramatically displaced and even reliable data will have significant limitations in extending the results to the entire patient population.
Randomization in an RCT should ensure the comparability of groups on various grounds and, most importantly, by signs that affect the outcome of the disease ... However, this can only be achieved with sufficiently large samples, which are not always possible to form. With a small number of patients, the comparability of groups, as a rule, is violated as a result of the fact that some of the persons, for various reasons, drop out of the experiment, which may prevent reliable conclusions from being drawn.
Rice. 7. A randomized controlled trial to evaluate the results of early hospital discharge in patients with myocardial infarction. Source. Fundamentals of Epidemiology. R Bighole et al. WHO, Geneva, 1994.
The data presented (Fig. 7) show how, for various reasons, the number of patients participating in the experiment has sharply decreased. As a result, the results of statistical processing turned out to be unreliable, and according to the data of this study, it can only be very tentatively believed that early discharge (after 3 days) is safe for people who have had myocardial infarction.
Decrease in reliability The randomization methods used in RCTs are most often categorized in the following order:
centralized randomization by telephone by an independent statistician, or a representative of a pharmaceutical company.
the method of coded (numbered) identical containers supplied by a pharmaceutical company, while the code and contents of the containers are unknown to either the patient or the doctors participating in the study;
centralized computer method - a computer program generates a random sequence of distribution of patients into groups, similar to the sequence in a table of random numbers, at the same time, the division of patients into comparison groups is carried out by a specialist who participates only in the randomization process.
the method of opaque, sealed and numbered envelopes. Intervention instructions will be placed in envelopes numbered sequentially according to a table of random numbers. It is extremely important that the envelopes are opened only after the researcher writes the patient's name and other necessary data on them in the admission department;
Regardless of the method, randomization can be simple and stratified (there are other, less commonly used types of randomization). In the case of simple randomization, additional factors are not taken into account, and each patient has a 50/50 chance of getting into one or another group. Stratified randomization (selection of subgroups - strata) is used in cases where it is impossible to create groups with the same prognosis of the outcome of the experience in the subjects. For example, if one of the specified parameters (age, blood pressure level, myocardial infarction, etc.) can affect the research result, patients are first divided into subgroups. Further, in each subgroup, the group is randomized. Some experts consider stratified randomization to be insufficiently correct.
Despite the extreme importance of information about the randomization method for the reader's assessment of the reliability of the study results, different authors give almost the same estimates of studies on this parameter. It was found that in the 80s - 90s only 25 - 35% of reports on RCTs published in specialized journals, and 40 - 50% of reports published in general medical journals, reported the use of the correct method of generating a random sequence of inclusion of participants in groups. ... In almost all of these cases, either a computer generator or a table of random numbers was used. In a 22-year analysis of articles published in a dermatology journal over a period of 22 years, only 1 of 68 RCT reports reported using the correct random sequencing method.
The most important element of the organization of RCT of treatment means is the use of the method of blinding (masking). As noted in the previous section, double and even triple-blind testing is preferred because patients or medical personnel participating in the trial, unwittingly or deliberately, can distort the data and thereby affect the research outcome.
Masking interventions from patients is important, because the outcome of the applied exposure largely depends on the psychological state of the patient. With the openness of information, patients in the experimental group can either unjustifiably hope for a favorable outcome of treatment, or, on the contrary, worry about the fact that they have agreed to be “experimental rabbits”. Patients in the control group may also behave differently, for example, feel deprived, especially if they believe that the treatment process is more successful in the experienced group. A different psychological state of patients can lead to a purposeful search for signs of improvement or, on the contrary, a deterioration in their state of health, which will inevitably affect their own assessment of the state, the changes of which often turn out to be imaginary. Disguise from the medical researcher is necessary, since he can be deliberately convinced of the benefits of the test agent and subjectively interpret changes in the health status of the test subjects.
The need for double masking objectively confirms the "placebo effect". Placebo is a dosage form that is indistinguishable from the study drug in appearance, color, taste, and smell, but does not have a specific effect, or other indifferent intervention used in medical research to simulate treatment in order to eliminate the bias associated with placebo effect. Placebo effect is a change in the patient's condition (noted by the patient himself or the attending physician) associated only with the fact of treatment, and not with the biological effect of the drug.
Numerous studies have found that some patients (depending on the disease up to 1/3), taking a placebo for the medicine, react to it in the same way, or almost in the same way as the patients of the experimental group. The study of the placebo effect allows you to isolate specific components of the new treatment. In addition, if patients do not know which group they belong to, they more closely follow the rules of the experiment.
As mentioned in the previous section, to improve the reliability of the conclusions, introduce third blindness at the stage of statistical data processing, entrusting these actions to independent persons.
"Blind" clinical trials are not used when evaluating the potential effectiveness of surgical interventions, physiotherapy methods, diets, many diagnostic procedures, etc., i.e. in those cases when it is impossible to mask the impact, or it is inappropriate either for patients or for doctors. In such cases, the randomized trials are called open.
After the specified observation time has elapsed, statistical processing of the identified outcomes (effects of exposure) of the disease in the experimental and control groups is carried out. In order to avoid bias, the criteria for the outcome of the disease in the experimental and control groups of patients should be specific and the same. To increase the reliability of the conclusions, the study is often carried out not simultaneously, but over a period, including new patients.
For the statistical processing of the data obtained, the same “two by two” table is used.

Table 11. Layout of the "two by two" table for evaluating the results of experimental studies.
Most of the indicators assessing the effectiveness of experimental exposure in clinical and field trials, although they have different names (as it happened historically), correspond both in the method of calculation and in meaning to the values calculated in cohort studies.
To quantify the effectiveness, various statistical indicators are used, while there is no strict unification of their names.
1.
The indicator of relative efficiency (
performance indicator
):

This value corresponds to the relative risk calculated in cohort studies. ... The performance indicator determines how many times , the frequency of positive outcomes of exposure in the experimental group is higher than their frequency in the control group, i.e. how many times a new method of treatment, diagnosis, etc., better than the commonly used one.
Evaluation criteria are used to interpret the performance indicator. relative risk (see statistical processing of cohort study data). In this case, accordingly, the meaning of the formulations changes, since it is not the risk factor of the disease that is assessed, but the effectiveness of the applied experimental influence.
2. Attributive (additional) effect , corresponds to the attributive (additional) risk determined in cohort studies.

The magnitude of the attributive effect shows how much the effect of the experimental exposure is greater than the effect of exposure in the control group;
3 . The proportion of the effect of the influence (the proportion of the effectiveness) corresponds to the etiological proportion calculated in the analysis of data from cohort studies.

This value shows the proportion of positive outcomes belonging to the experimental effect in the sum of positive effects in the experimental group.
4. an additional quantity called - number of patients to be treated (NNT) to prevent one adverse outcome.

The higher this indicator, the lower the potential effectiveness of the studied impact.
Just as in the processing of data from cohort studies, the reliability of the data obtained in experiments is assessed using the chi-square test or other methods.
In conclusion, we note that, despite all the advantages, randomized clinical trials are fraught with the possibility of bias, especially sampling bias. Consequently, the results of one study, even flawless in organization, cannot be considered as an unconditional recommendation for the use of a new drug in clinical practice. This is why, at present, only the results are considered reliable. multicenter studies the effectiveness of the same intervention (treatment) by several clinics, while it is desirable that the research be conducted in clinics in different countries.
Antineoplastic drugs differ, each of them is carried out for specific purposes and is matched to the necessary parameters for the study of the drug. At the moment, the following types of clinical trials are distinguished:
Open and Blind Clinical Trial
Clinical research can be open and blind. Open research- this is when both the doctor and his patient know which drug is being investigated. Blind exploration divided into simple blind, double-blind and full-blind research.
- Simple blind exploration- this is when one party does not know which drug is being investigated.
- Double blind research and full blind exploration is when two or more parties do not have information about the investigational drug.
Pilot clinical study is carried out to obtain preliminary data that are important for planning further stages of the study. In plain language, one could call it "sighting". With the help of a pilot study, the possibility of conducting a study on a larger number of subjects is determined, the necessary capacities and financial costs for future research are calculated.
Controlled clinical trial is a comparative study in which a new (investigational) drug, the efficacy and safety of which has not yet been fully studied, is compared with a standard treatment method, that is, a drug that has already passed research and entered the market.
Patients in the first group receive study drug therapy, patients in the second receive standard therapy (this group is called control, hence the name of the type of study). The comparison drug can be either standard therapy or placebo.
Uncontrolled clinical trial- This is a study in which there is no group of subjects taking a comparison drug. Usually, this type of clinical research is carried out for drugs with already proven efficacy and safety.
Randomized clinical trial is a study in which patients are randomly assigned to several groups (by type of treatment or drug regimen) and have the same opportunity to receive the study or control drug (comparison drug or placebo). V nonrandomized study the randomization procedure is not carried out, therefore, patients are not divided into separate groups.
Parallel and crossover clinical trials
Parallel clinical trials- These are studies in which subjects in different groups receive either only the studied drug, or only the reference drug. A parallel study compares several groups of subjects, one receiving the study drug and the other being the control group. Some parallel studies compare different treatments without including a control group.
Cross-sectional clinical trials- These are studies in which each patient receives both compared drugs, in a random sequence.
Prospective and Retrospective Clinical Study
Prospective clinical trial- This is the observation of a group of patients for a long time, before the onset of the outcome (a clinically significant event that serves as the object of interest of the researcher - remission, response to treatment, occurrence of relapse, death). Such a study is the most reliable and therefore is carried out most often, and in different countries at the same time, in other words, it is international.
In contrast to the prospective study, retrospective clinical study on the contrary, the outcomes of previous clinical trials are being studied; outcomes occur before the study begins.
Single-center and multicenter clinical trial
If a clinical trial is conducted at one research center, it is called single-center, and if based on several, then multicenter... If, however, the study is conducted in several countries (as a rule, the centers are located in different countries), it is called international.
Cohort Clinical Study Is a study in which a selected group (cohort) of participants is observed over a period of time. At the end of this time, the results of the study are compared in subjects in different subgroups of this cohort. Based on these results, a conclusion is made.
In a prospective cohort clinical study, groups of subjects are composed in the present and observed in the future. In a retrospective cohort clinical study, groups of subjects are selected based on historical data and their results are tracked to the present.

What type of clinical trial will be the most reliable?
Recently, pharmaceutical companies are obliged to conduct clinical trials in which the most reliable data... Most often meets these requirements prospective, double-blind, randomized, multicenter, placebo-controlled study... It means that:
- Prospective- will be monitored for a long time;
- Randomized- patients were randomly assigned to groups (usually this is done by a special computer program, so that in the end the differences between the groups become insignificant, that is, statistically unreliable);
- Double blind- neither the doctor nor the patient knows which group the patient fell into during randomization, therefore, such a study is as objective as possible;
- Multicenter- is performed in several institutions at once. Some types of tumors are extremely rare (for example, the presence of an ALK mutation in non-small cell lung cancer), so it is difficult to find the necessary number of patients in one center who meet the criteria for inclusion in the protocol. Therefore, such clinical trials are carried out at once in several research centers, moreover, as a rule, in several countries at the same time and are called international;
- Placebo controlled- Participants are divided into two groups, some receive the study drug, others a placebo;
Acute respiratory infections (ARI) of viral etiology, including influenza, are widespread throughout the world and cause significant economic damage to both the health care system and the economy as a whole, including through an increase in the number of days of disability. The development of new methods for the prevention, control and treatment of ARI and influenza is an urgent medical problem.
The search for new antiviral agents is carried out in two directions: in the first case, the “target” is the pathogen, in the second, the human body, into which the virus is introduced. The action of drugs with direct antiviral action is aimed at blocking viral enzymes that play a key role in the stages of replication, transcription, and release of viruses. Another group of drugs is characterized by a pathogenetic effect aimed at correcting the processes accompanying virus-induced inflammation in the respiratory tract. In this context, it is worth noting that the current WHO strategy on influenza draws attention to the need for a more detailed study of immunomodulators. Obviously, this interest is due to the peculiarities of the antiviral immune response associated with the interferon system. It is known that adequate induction of interferon genes in the first 4 days of illness contributes to a mild course of influenza, while a severe course of infection is noted with insufficient activation of interferons.
One of the drugs that affect the regulation of antiviral reactions due to the targeted effect on the main molecules involved in the immune response is Ergoferon. The drug contains affinity purified antibodies to interferon gamma, CD4 + receptor and histamine, subjected to technological processing (ultra-high dilutions), as a result of which the active components acquire the ability to modify the activity of their targets by affecting their conformational parameters. As a result, Ergoferon changes the interaction of endogenous molecules with the corresponding receptors, providing a complex antiviral, immunomodulatory, anti-inflammatory and antihistamine effect.
The therapeutic efficacy and safety of the complex antiviral drug Ergoferon in adults and children with ARI and influenza has been shown in randomized clinical trials. The drug significantly reduces the duration of fever, intoxication and catarrhal symptoms, and is also effective in eliminating existing complications of acute respiratory viral infections and influenza. The purpose of this study was to study the safety and efficacy of a new liquid dosage form of the drug in adults with upper respiratory tract acute respiratory infections.
Material and research methods
Study design
A double-blind, placebo-controlled, randomized clinical trial in parallel groups with a 1: 1 ratio (phase III).
Eligibility criteria
The study involved outpatients of both sexes 18-60 years old with manifestations of ARI of the upper respiratory tract (body temperature> 37.8 ° C, the presence of two or more symptoms of moderate severity (2 points) or three or more symptoms of mild severity (1 score) according to the CCQ (Common Cold Questionnaire) scale within ≤ 24 hours from the onset of the disease). The patient was included in the study after signing an informed consent form for participation if the inclusion / exclusion criteria were met based on the results of screening (history, thermometry and physical examination). To assess body temperature, tympanic thermometry using an individual electronic infrared thermometer was used, which is a valid method comparable to measurements in other areas of the body. The study did not include patients with suspected invasive bacterial infection or the presence of severe illness requiring the appointment of antibacterial drugs (including sulfonamides); suspicion of the initial manifestations of diseases with symptoms similar to ARI. In addition, exacerbation or decompensation of chronic diseases served as exclusion criteria; mental illness, impaired glucose tolerance, type 1 and 2 diabetes mellitus; oncological diseases; burdened allergic history, hereditary fructose intolerance (due to the presence of maltitol in the study drug), as well as allergies / intolerance to any of the components of approved drugs, pregnancy, breastfeeding, alcohol abuse, drug use; participation in other clinical trials within the previous 3 months. All study participants used contraceptive methods during the study and for 30 days after its completion.
Randomization
After the screening procedure, the patients included in the study were randomized using a special Interactive Voice System (ICS) based on a random number generator in a 1: 1 ratio into 2 groups: group 1 (Ergoferon) and group 2 (placebo). Block randomization was used with a block size of at least 4 participants. The ICS used ensured uniform inclusion in the study of patients of different age groups, their distribution into groups and the correct prescription of the study therapy.
Description of the intervention
Patients from group 1 received the study drug according to the following scheme: on the first day of treatment, 8 doses (in the first 2 hours, 1 measuring spoon every 30 minutes, then, in the remaining time, 3 more times at regular intervals), with 2 on the 5th day - 1 measuring spoon 3 times a day. Patients from group 2 received placebo according to the Ergoferon regimen. All study participants, if necessary, received symptomatic ARI therapy: drugs for the treatment of cough, vasoconstrictor nasal drops, detoxification therapy and antipyretic drugs (paracetamol 500 mg or Nurofen® 200 mg, provided by the sponsor). For 1 month before and during the study, it was prohibited to take antiviral (except for Ergoferon in the framework of this study), antibacterial, antihistamines, anticancer drugs, drugs with immunotropic action, vaccines, immunoglobulins, sera, etc.
Each patient was observed up to 7 days (screening and randomization - 1st day, treatment - 1-5 days, observation at the end of treatment - up to two days). In total, in the course of treatment and observation, 3 visits were carried out (visit 1, visit 2, visit 3, respectively, on the 1st, 3rd and 7th days of observation). At visits 1 and 3, samples were taken for laboratory research. At Visits 2 and 3, the investigator performed physical examination, including thermometry and assessment of the severity of ARI symptoms using the CCQ scale. General symptoms (fever, chills, muscle pain), symptoms associated with the nose (nasal discharge, sneezing, watery eyes), throat (sore throat) and chest (cough, chest pain) symptoms were assessed in points from 0 up to 3. And also the prescribed and concomitant therapy was monitored, the safety of the treatment was assessed, the patient's diary was checked (in which the patient daily in the morning and in the evening from the first day of treatment noted the values of the tympanic temperature and ARI symptoms according to the WURSS-21 questionnaire (The Wisconsin Upper Respiratory Symptom Survey - 21) This questionnaire allows you to assess the severity of ARI in points from 0 to 7 for each item: the patient's general well-being, the severity of ARI symptoms (“Symptoms” domain), the effect of the disease on the patient's ability to cope with various types of daily activities (“ Ability ").
Blindness
The double-blind study design provided for identical appearance and organoleptic properties of the study drug and placebo, as well as the absence of information about the received therapy (Ergoferon or placebo) in patients, researchers, research center staff and the sponsor's team until the study was completed and the database was closed.
Research endpoints
The average duration of fever (body temperature above 37.0 ° C) according to the patient's diary was used as the primary efficacy criterion. Its completion was considered the absence of temperature> 37.0 ° C for 24 hours or longer. Additionally, we assessed: the dynamics of ARI clinical manifestations according to the physician's objective examination (the sum of CCQ scores on the 1st, 3rd and 7th days of treatment), the dynamics of ARI symptoms according to the patient's daily subjective assessment (total score and domain scores of the WURSS questionnaire -21 according to the patient's diary), the number of antipyretic drugs (on the 1st, 2nd, 3rd, 4th and 5th days of treatment), the proportion of patients with worsening of the course of the disease (the appearance of ARI symptoms of the lower respiratory tract , the development of complications requiring antibiotics or hospitalization). The safety of therapy was assessed taking into account the number and nature of adverse events (AEs), their relationship with the drug intake; deviations of laboratory parameters during treatment.
Sample size calculation
The sample size was calculated taking into account the power of statistical tests equal to 80%, the probability of a type I error less than 5 and the expected effect of the study drug in the form of a reduction in the mean duration of fever compared with placebo. Taking into account the study dropout rate of 1.1, the minimum sample size required was 342.
Features of statistical analysis
As part of the study, it was planned to conduct an interim analysis (with the aim of correcting the sample size or stopping the study early) at 2 stages - including at least 60 and at least 105 patients in each group who received therapy and completed all visits in full accordance with the protocol. In this regard, the critical value of the error of the first kind for the final analysis was established using the rules of the Pocock boundary at the level of α = 0.0221; all results were considered significant only if the "p" value was equal to or less than this value. For data processing, the χ 2 test was used, and for multiple comparisons, the χ 2 test modified by Cochran-Mantel-Haenszel (CMH). Continuous variables were analyzed using the nonparametric Kruskal-Wallis test and χ 2 Median One-Way Analysis. Multivariate analysis of continuous and polynomial variables was performed using the analysis of variance for repeated measurements (Repeated Measures Analysis Of Variance, ANOVA, The MIXED Procedure). Numerical data are presented as mean, standard deviation, as well as median, maximum and minimum values. To compare the severity of the course of the disease in the groups, the Area Under Curve (AUC) model was used for the total score of the CCQ scale and the WURSS-21 questionnaire. This indicator was calculated as the product of the total CCQ / WURSS-21 score by the number of visits / days (n = 3/7) during which symptoms were recorded.
The permission of the Ministry of Health of the Russian Federation No. 835 to conduct the study was obtained on March 30, 2012, 22 research centers were approved - outpatient clinics of medical institutions in Moscow, St. Petersburg, Yaroslavl, Kazan, Chelyabinsk and Voronezh. The study was conducted during the 2012-2015 epidemiological seasons. with the support of OOO NPF Materia Medica Holding. The study design is presented in the world database of clinical trials - ClinicalTrials.gov, CT id: NCT01765920.
Research results
Patient characteristics
Patients were randomized to study drug (group 1; n = 169) and placebo (group 2; n = 173). This sample was used to assess the safety of therapy (all included patients who received at least one dose of the study drug / placebo (Safety population, n = 342). 8 patients dropped out during the study (7 patients were included in error, 1 patient had the code disclosed and data were not available after inclusion), 12 more participants were excluded during data processing due to serious deviations from the protocol (Fig. 1).
Thus, the Intention to treat (ITT) analysis included data from 167 patients in group 1 and 167 patients in group 2; 160 patients of the 1st group and 162 patients of the 2nd group completed their participation in the study in accordance with the procedures of the Per protocol protocol (PP-analysis).
The mean age of all included and randomized patients (n = 342) was 36.3 ± 10.6 years in group 1 and 35.1 ± 10.9 years in group 2 (χ 2 = 0.867, p = 0, 35). The groups did not differ in the sex ratio: 71 (42.0%) men and 98 (58.0%) women versus 58 (33.5%) men and 115 (66.5%) women in the 1st and 2nd groups, respectively (p = 0.119) (data are presented as the mean and its standard deviation).
The clinical picture of the disease in patients was manifested by fever in combination with symptoms of intoxication and catarrhal manifestations. The mean body temperature at visit 1 was 38.1 ± 0.3 ° C in group 1 and 38.1 ± 0.3 ° C in group 2, p = 0.40 (hereinafter, the data are presented in the form of ITT [PP] samples, respectively). When the physician assessed the initial total score of the severity of ARI symptoms on the CCQ scale - 10.4 ± 3.6 points in the Ergoferon group and 10.7 ± 3.9 points in the placebo group (p = 0.72 [p = 0.59]) ... In the patient's assessment, the initial total score for WURSS-21 was 68.7 ± 25.3 points in the Ergoferon group and 73.4 ± 27.4 points in the placebo group (p = 0.11 [p = 0.07]). The average values of the “Symptoms” domain were registered at the level of 28.3 ± 11.2 and 30.3 ± 11.4 points, for the “Ability” domain - 30.0 ± 15.8 and 32.7 ± 17.2 points in two groups accordingly, without significant differences between groups. Initially, demographic, anthropometric characteristics, the severity of clinical symptoms of ARI of participants excluded from the analysis were within the values of patients whose data were included in the ITT analysis [PP analysis] and did not differ between groups.
Most of the participants in group 1 (92.3%) and group 2 (94.1%) received concomitant drug therapy (p = 0.502 [p = 0.798]). Most often, both groups used vasoconstrictor nasal drops and sprays, antitussive drugs, vitamin-mineral complexes, dental drugs, non-steroidal anti-inflammatory drugs, drugs for the treatment of throat diseases, antiseptics and disinfectants, and analgesics. Single patients took drugs of other pharmacological groups, including angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists, beta-blockers, calcium channel antagonists, diuretics, hemostatic drugs, combined oral contraceptives. There were no statistically significant differences between the groups, as well as patients excluded from the analysis of efficacy in terms of the incidence of concomitant diseases and the use of concomitant therapy drugs.
Safety assessment of therapy
The safety assessment included an analysis of patient complaints, physical examination data, and laboratory tests of all patients who received at least one dose of study drug / placebo (n = 342).
The study drug had no negative effect on vital parameters, including heart rate (HR), systolic (SBP) and diastolic (DBP) blood pressure. The main indicators of the respiratory and circulatory organs in all study participants were within the normal range.
In total, 15 AEs were detected in 13 patients, including 8 AEs in 7 patients of the 1st group and 7 AEs in 6 patients of the 2nd group, without significant differences between the number of patients with AEs in the compared groups (Fisher's exact test; p = 0.784) and the frequency of AEs related to a particular Medical Dictionary for Regulatory Activities (MedDRA) code. In group 1, there were 3 moderate AEs in the form of acute bronchitis (n = 1), sinusitis (n = 1) and acute purulent rhinosinusitis (n = 1), which required the appointment of antibacterial therapy of systemic action; 5 AEs of mild severity in the form of various deviations of laboratory parameters (uraturia (n = 1), neutropenia (n = 1) and lymphocytosis (n = 1), increased levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) (n = 1)) and acute anal fissure (n = 1). All AEs were unrelated or unlikely to be related to study therapy. During participation in the study, 2 patients of the 2nd group showed a worsening of the ARI course in the form of generalization of infection with the development of community-acquired lower lobe right-sided pneumonia (n = 1) and acute bronchitis (n = 1), which required the appointment of antibiotic therapy. The other 5 AEs in the placebo group were represented by abnormalities in laboratory tests - an increase in the number of erythrocytes in urine (n = 1) and the presence of mucus in it (n = 1), an increase in the level of ALT and AST (n = 1), acute allergic reaction in the form of urticaria (n = 1), facial flushing (n = 1).
The average values of laboratory parameters both at baseline and at the end of the course of treatment did not go beyond the reference values. According to statistical analysis, the number of clinically significant deviations from the norm in blood and urine tests in groups 1 and 2 did not differ (p = 1,000).
During the study, no data were obtained on the interaction of the study drug with drugs used as concomitant therapy, no exacerbations of chronic or allergic diseases were recorded in study participants. The treatment was well tolerated by the patients, contributing to their high compliance.
Evaluation of the effectiveness of therapy
The duration of the febrile period of ARI in the 1st group was 3.1 ± 1.2 days, which was significantly less than in the 2nd group - 3.6 ± 1.4 days (p = 0.0174 [p = 0, 0136]) (table). Ergoferon treatment reduced the febrile period by an average of 0.43 ± 1.30 days, 95% CI 0.15-0.71 (or 10.3 hours).
The study drug group was dominated by patients whose fever had stopped during the first days of therapy. Its duration of no more than 1 day was observed in 11 (6.6%) patients of the 1st group versus 3 (1.8%) patients of the 2nd group. The duration of the febrile period up to 2 days inclusive was noted in 42 (25.1%) patients of the 1st group versus 36 (21.7%) of the 2nd group. In addition, patients with fever for more than 6 days were absent in the Ergoferon group. In the 1st group, only 3 (0.9%) patients had a fever on the 6th day of the study, while in the 2nd group, 20 (12.0%) patients had fever for 6 days or more.
According to an objective examination by a doctor on the 3rd day of treatment with Ergoferon, the average value of the total CCQ score from the initial 10.4 ± 3.6 points decreased by more than 50%, amounting to 4.7 ± 2.9 points versus 5.3 ± 3, 1 point in the placebo group (p = 0.06 [p = 0.03]). By the 3rd visit, clinical manifestations of ARI were practically absent in patients of both groups and amounted to 0.6 ± 1.1 points in the 1st group and 1.0 ± 1.6 points in the second. When comparing the severity of the course of the disease in the groups using the AUC for the total CCQ score, a tendency towards a lighter course for the 1st group was shown - 25.7 ± 12.0 y. e. versus 28.5 ± 13.9 c.u. i.e. in the 2nd group (p = 0.0719).
According to the patient's daily subjective assessment, the severity of the ARI course (AUC for the total score WURSS-21) in the study drug group was lower - 201.6 ± 106.1 s. i.e. against 236.2 ± 127.9 c.u. e. in the placebo group; p = 0.02 [p = 0.015] (Fig. 2).
The results of the analysis of the area under the curve for the scores of the "Symptoms" domain of the WURSS-21 questionnaire showed a lesser severity of ARI symptoms in the group of the study drug - 85.2 ± 47.6 c. i.e. against 100.4 ± 54.0 c.u. ie, when taking placebo, p = 0.0099 [p = 0.0063] (Fig. 3).
.gif)
The decrease in the "Ability" domain indicators by the end of treatment reflected the restoration of the patient's ability to perform daily activities. The results of the analysis of the area under the curve for this indicator illustrated the trend of more pronounced dynamics in the 1st group (p = 0.037 [p = 0.029]). Pairwise comparison of the mean values of the total score of the WURSS-21 questionnaire and its individual domains showed a lesser severity of ARI symptoms in the group of the study drug, mainly on days 2-5 of treatment.
When assessing the need for the use of antipyretic drugs, it was noted that in the overwhelming majority of patients, the number of antipyretics doses did not exceed 1 time per day (mainly on 1-2 days of illness). In this connection, the analysis according to this criterion was carried out by comparing the proportions of patients taking antipyretic drugs. On the 1st day of observation, 36.5% of patients in the 1st group and 43.4% of patients in the 2nd group used antipyretics. On the 2nd day, the proportion of patients in both groups decreased to 16.2% and 20.5% (1st and 2nd, respectively). Despite the fact that there were no intergroup differences in the use of antipyretic drugs, the normalization of body temperature in patients of group 1 was faster, as described above. The results obtained confirm the effective effect of the study drug on the course of the infectious-inflammatory process in the respiratory tract in ARI.
When comparing the proportion of patients with worsening of the course of the disease, there were no differences between the groups (p = 0.68 [p = 1.00]). The onset of ARI symptoms in the lower respiratory tract and paranasal sinuses requiring antibiotic therapy, noted in 5 study participants (n = 3 in group 1 and n = 2 in group 2), are described above as AE. In patients who completed the full course of treatment with the study drug, there was no worsening of the course of the disease, the occurrence of complications or hospitalizations during treatment and follow-up.
Discussion
A study conducted under a double-blind placebo control showed the efficacy of a liquid dosage form of a complex antiviral drug in the treatment of ARI of the upper respiratory tract in adults.
It is known that the main criterion for resolving an infectious and inflammatory process in the respiratory tract is temperature normalization. It was found that the use of Ergoferon leads to a reduction in the duration of fever by an average of 10 hours. The average duration of the febrile syndrome when it was taken was 3 days. There was a greater number of cases with an abortive course of a febrile period (1-2 days) compared with placebo. In the placebo group, more than 10% of patients had fever for 6-8 days. And in the Ergoferon group, there were no cases of fever duration more than 6 days.
The study showed that the use of Ergoferon contributed to a decrease in the severity of an acute infectious and inflammatory process and led to a faster and more effective recovery from ARI. The effective effect of the study drug on the course of the disease was manifested by a positive effect not only on fever, but also on other symptoms of ARI from the nose / throat / chest. According to a medical examination with a CCQ score on the 3rd day of therapy, the severity of ARI symptoms in patients of the Ergoferon group decreased by more than 50%. The obtained objective data coincided with the subjective assessment of the patients in the WURSS-21 questionnaire. Patients receiving antiviral therapy noted a significant improvement in well-being, a decrease in ARI symptoms and a restoration of daily activity at the very beginning and in the midst of the disease (on days 2-5). The results obtained are of particular interest due to the fact that during this period, as a rule, the maximum severity of the disease is noted in the absence of adequate treatment. It is worth noting that the use of symptomatic therapy, including antipyretics, did not differ between the patients of the two groups. Participants who completed the full course of therapy with Ergoferon and completed their participation in the study in accordance with all procedures of the protocol did not experience any worsening of the course of the disease or the appearance of complications that required the appointment of antibiotic therapy.
The effectiveness of the drug is explained by its complex composition, which has a targeted effect on target molecules: interferon gamma, CD4 + receptor and histamine receptors. The modulating effect of one of the components of the drug on interferon gamma consists in changing the conformation of the molecule and increasing its functional activity, which improves the ligand-receptor interaction of interferon gamma with the receptor, increases the expression of interferon gamma / alpha / beta and interleukins associated with them, and restores the cytokine status; normalization of the concentration and functional activity of natural antibodies to interferon gamma; stimulation of interferon-dependent biological processes. Another component of the drug, acting on the cytoplasmic domain of the CD4 + receptor, causes the activation of T-lymphocytes by increasing the activity of lymphocytkinase and promotes the recognition of antigens by T-helper cells together with the molecules of the major histocompatibility complex (MHC) class II, which, in turn, triggers the cellular and humoral immune response. The third component of the drug modifies the histamine-dependent activation of peripheral and central histamine receptors, which leads to a decrease in capillary permeability, a decrease in edema of the mucous membrane of the respiratory tract, and suppression of histaminoliberation from mast cells and basophils.
Taking into account the effectiveness of drugs with immunotropic action in the treatment of ARVI and influenza, it should be noted that the positive effect of Ergoferon on the main clinical manifestations of ARI - fever, intoxication and respiratory symptoms - is due to a combination of nonspecific antiviral activity and anti-inflammatory, antihistamine effects.
conclusions
The study found that taking a liquid dosage form of Ergoferon helps the patient recover from ARI faster and facilitates the course of the disease, starting from the very first days of treatment. Based on the results of the study, the following conclusions can be drawn:
- The therapeutic efficacy of Ergoferon in the treatment of ARI in adults is manifested by a significant decrease in the duration of the febrile period; the time to complete normalization of body temperature (≤ 37.0 ° C) is on average about 3 days.
- On the 3rd day of treatment with Ergoferon, the severity of symptoms of acute respiratory infection in patients decreases by more than 50%.
- The use of Ergoferon makes it possible to more effectively stop the severity of symptoms of acute respiratory infection (results of analysis by the "Symptoms" domain), and also leads to a faster recovery of patients' daily activity (results of analysis by the "Ability" domain of the WURSS-21 questionnaire).
- The safety of the drug was confirmed by the absence of registered adverse events that have a reliable connection with the study therapy, the absence of deviations from the normal values of biochemical and general clinical parameters of blood and urine.
- There were no cases of negative interaction of Ergoferon with drugs of various classes, including antipyretics, decongestants, antitussives, ACE inhibitors, angiotensin II receptor antagonists, beta-blockers, calcium channel antagonists, diuretics, hemostatics, combined hormonal mineral contraceptives, vitamins, local antiseptics.
- The significant efficacy of Ergoferon in the treatment of acute respiratory infections, compared with placebo therapy, is noted in the absence of differences in the use of symptomatic therapy drugs, including antipyretics.
- Patients tolerate the drug in liquid dosage form well and demonstrate a high level of adherence to therapy.
Thus, the liquid dosage form of Ergoferon is a safe and effective agent in the treatment of acute respiratory infections in adults.
Literature
- Ferkol T., Schraufnagel D. The global burden of respiratory disease // Ann. Am. Thorac. Soc. 2014, 11, 404-406. DOI: 10.1513 / AnnalsATS.201311-405PS.
- World Health Organization. Influenza (Seasonal). Available online at: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal) (accessed January 25, 2019).
- Behzadi M. A., Leyva-Grado V. H. Overview of Current Therapeutics and Novel Candidates Against Influenza, Respiratory Syncytial Virus, and Middle East Respiratory Syndrome Coronavirus Infections // Front Microbiol. 2019; 10: 1327. DOI: 10.3389 / fmicb.2019.01327.
- Nikiforov V.V. et al. Influenza and acute respiratory viral infections: modern etiotropic and pathogenetic therapy. Algorithms for providing medical care to patients. Guidelines. M .: Spetskniga; 2019.32 p.
- Kotey E., Lukosaityte D., Quaye O., Ampofo W., Awandare G., Iqbal M. Current and novel approaches in influenza management // Vaccines (Basel). 2019; Jun 18; 7 (2). DOI: 10.3390 / vaccines7020053.
- Jin Y., Lei C., Hu D., Dimitrov D. S., Ying T. Human monoclonal antibodies as candidate therapeutics against emerging viruses // Front. Med. 2017, 11, 462-470. DOI: 10.1007 / s11684-017-0596-6.
- Nicholson E. G., Munoz F. M. A review of therapeutics in clinical development for respiratory syncytial virus and influenza in children // Clin Ther. 2018, Aug; 40 (8): 1268-1281. DOI: 10.1016 / j.clinthera.2018.06.014. Epub 2018 Aug 2.
- Shaw M. L. The Next Wave of Influenza Drugs // ACS Infect. Dis. 2017, 3, 691-694.
- Ashraf U., Tengo L., Le Corre L. et al. Destabilization of the human RED-SMU1 splicing complex as a basis for host-directed antiinfluenza strategy // Proc Natl Acad Sci USA. 2019, May 28; 116 (22): 10968-10977. DOI: 10.1073 / pnas. 1901214116.
- Global influenza strategy 2019-2030. Geneva: World Health Organization; 2019. Available at: https://apps.who.int/iris/handle/10665/311184.
- Dunning J., Blankley S., Hoang L. T. et. Al. Progression of whole blood transcriptional signatures from interferon-induced to neutrophil-associated patterns in patients with severe influenza // Nat Immunol. 2018, June; 19 (6): 625-635. DOI: 10.1038 / s41590-018-0111-5.
- Epstein O. The spatial homeostasis hypothesis // Symmetry. 2018. Vol. 10 (4). 103. DOI: 10.3390 / sym10040103.
- Instructions for the medical use of the drug Ergoferon.
- Rafalskiy V. V., Averyanov A. V., Bart B. Ya. et al. Efficacy and safety of Ergoferon compared to oseltamivir in the outpatient treatment of seasonal influenza virus infection in adult patients: a multicenter open-label randomized clinical study // Spravochnik poliklinicheskogo vracha. 2016; (6): 24-36.
- Verevshchikov V.K., Borzunov V.M., Shemyakina E.K. Optimization of etiopathogenetic therapy of influenza and acute respiratory viral infections in adults with the use of ergoferon // Antibiotics and chemotherapy. 2011; 56 (9-10): 23-26.
- Selkova E.P., Kostinov M.P., Bart B.Ya., Averyanov A.V., Petrov D.V. Treatment of acute respiratory viral infections in adults: results of a randomized, double-blind, placebo-controlled clinical trial // Pulmonology. 2019; 29 (3): 302-310. https://doi.org/10.18093/0869-0189-2019-29-3-302-310 .
- Geppe N. A., Kondyurina E. G., Melnikova I. M. et al. Release-active antiviral drug Ergoferon in the treatment of acute respiratory infections in children. The effectiveness of the liquid dosage form of Ergoferon: results of a randomized, double-blind, placebo-controlled clinical trial // Pediatrics. 2019; 98 (1): 87-94.
- Averyanov A. V., Babkin A. P., Bart B. Ya. Et al. Ergoferon and oseltamivir in the treatment of influenza - the results of a multicenter comparative randomized clinical trial // Antibiotics and chemotherapy. 2012; 57 (7-8): 23-30.
- Spassky A.A., Popova E.N., Ploskireva A.A. The use of Ergoferon in the treatment of acute respiratory viral infections and influenza in adult patients with various concomitant diseases // Therapy. 2018; 6 (24): 157-161.
- Shestakova NV, Zagoskina NV, Samoilenko EV et al. Efficiency and safety of Ergoferon in the complex therapy of community-acquired pneumonia // Doctor.ru. 2012; 8 (76): 44-47.
- Radtsig E. Yu., Ermilova NV, Malygina LV et al. Etiotropic therapy of inflammatory diseases of the upper respiratory tract - complications of acute respiratory infection // Questions of modern pediatrics. 2014; 13 (6): 113-116.
- Powell H., Smart J., Wood L. G. et al. Validity of the Common Cold Questionnaire (CCQ) in Asthma Exacerbations // PLOS ONE. 2008, 3 (3): e1802. https://doi.org/10.1371/journal.pone.0001802.
- Chue A. L., Moore R. L. et al. Comparability of tympanic and oral mercury thermometers at high ambient temperatures // BMC Research Notes. 2012, 5: 356-361.
- Gasim G. I., Musa I. R., Abdien M. T., Adam I. Accuracy of tympanic temperature measurement using an infrared tympanic membrane thermometer // BMC Research Notes 2013, 6: 194-198.
- Barrett B., Brown R. L., Mundt M. P., Safdar N., Dye L., Maberry R., Alt J. The Wisconsin Upper Respiratory Symptom Survey is responsive, reliable, and valid // Journal of Clinical Epidemiology. 2005; 58 (6): 609-617.
- Sherstoboev E. Yu., Masnaya NV, Dugina Yu. L. et al. Ultra-low doses of antibodies to interferon gamma affect the Th1 / Th2 balance. M .: 5th congress "Modern problems of allergology, immunology and immunopharmacology", 2002. 281 p.
- Epshtein OI, Belsky Yu. P., Sherstoboev E. Yu., Agafonov VI, Martyushev AV Mechanisms of immunotropic properties of potentiated antibodies to human interferon-γ // Bul. expert. biol. 2001; 1: 34-36.
- Epshtein O.I., Dugina Yu.L., Kachanova M.V., Tarasov S.A., Kheifets I.A., Belopolskaya M.V. Antiviral activity of ultra-low doses of antibodies to interferon gamma // Bulletin of the International Academy of Sciences (Russian Section). 2008; 2: 20-23.
- Emelyanova A.G., Grechenko V.V., Petrova N.V., Shilovsky I.P., Gorbunov E.A., Tarasov S.A., Khaitov M.R., Morozov S.G., Epshtein O I. Influence of release-active antibodies to the CD4 receptor on the level of lck-kinase in the culture of human peripheral blood mononuclear cells // Bulletin of Experimental Biology and Medicine. 2016; 162 (9): 304-307.
- Zhavbert E.S., Dugina Yu.L., Epshtein OI Anti-inflammatory and anti-allergic properties of antibodies to histamine in a release-active form: a review of experimental and clinical studies // Children's infections. 2014, 1: 40-43.
- Kostinov M. P. http://orcid.org/0000-0002-1382-9403
- Kostinov M.P. A new drug for the treatment of influenza and acute respiratory viral infections // Infectious Diseases. 2011.9 (4): 29-34.
- Kostinov M.P. Immunocorrection in Pediatrics / A Practical Guide for Physicians. M .: "Medicine for all", 1997. 111 p.
- Afinogenova V.P., Lukachev I.V., Kostinov M.P. Immunotherapy: mechanism of action and clinical use of immunocorrective drugs // Attending physician. 2010.4: 9.
- Federal guidelines for the use of medicines (formulary system, reference edition). Issue XVI. Ed. A.G. Chuchalina (editor-in-chief), V.V. Yasnetsova. M .: "Echo", 2015.1016 p.
- Guide to Clinical Immunology in Respiratory Medicine / Ed. M.P. Kostinova, A.G. Chuchalina. 1st ed. Moscow: ATMO, 2016.128 p.
- Respiratory medicine. Management. / Ed. A.G. Chuchalin, (2nd ed., Revised and supplemented). M .: Litterra, 2017; T. 2.544 p.
M. P. Kostinov *, 1,
R. F. Khamitov **,Doctor of Medical Sciences, Professor
A.P. Babkin ***, Doctor of Medical Sciences, Professor
E. S. Minina ****, Candidate of Medical Sciences
B. Ya. Bart #, Doctor of Medical Sciences, Professor
M.P. Mikhailusova #, Doctor of Medical Sciences, Professor
M. E. Yanovskaya ##,Candidate of Medical Sciences
A. O. Sherenkov ###,Candidate of Medical Sciences
D. V. Petrov ####, Candidate of Medical Sciences
D. N. Alpenidze &, Candidate of Medical Sciences
Yu. S. Shapovalova &&, Candidate of Medical Sciences
M. V. Chernogorova &&&,Doctor of Medical Sciences, Professor
E. F. Pavlysh @, Candidate of Medical Sciences
R. T. Sardinov @@, Candidate of Medical Sciences
* FGBNU NIIVS them. I. I. Mechnikov RAS, Moscow
** FSBEI HE Kazan State Medical University of the Ministry of Health of Russia, Kazan
*** BUZ VO VGKP No. 4, Voronezh
**** FGBU PC No. 3 UDP RF, Moscow
# FGBOU IN RNIMU them. N.I. Pirogova, Ministry of Health of Russia, Moscow
## GBUZ YAO OKB, Yaroslavl
### SPb GBUZ VFD Krasnogvardeisky District, Saint Petersburg
#### FGBOU VO YSMU of the Ministry of Health of Russia, Yaroslavl
& SPb GBUZ GP No. 117, Saint Petersburg
&& NUZ DKB at the Chelyabinsk station of JSC Russian Railways, Chelyabinsk
&&& BUZ MO Podolskaya GB No. 3, Podolsk
@ SPb GBUZ GP Nevsky District, Saint Petersburg
@@ FGBUZ PK No. 1 RAS, Moscow
DOI: 10.26295 / OS.2019.29.30.015
Treatment of acute respiratory infection in adults: results of a multicenter, randomized, double-blind, placebo-controlled clinical trial / M.P. Kostinov, R.F. Khamitov, A.P. Babkin, E.S. Minina, B. Ya. Bart, M. P. Mikhailusova, M. E. Yanovskaya, A. O. Sherenkov, D. V. Petrov, D. N. Alpenidze, Yu. S. Shapovalova, M. V. Chernogorova, E. F. Pavlysh, R. T. Sardinov
For citation: Attending physician No. 10/2019; Page numbers in the issue: 72-79
Tags: influenza, viral infection, antiviral treatment, immune response.
UDC 614 (072).
A.M. Raushanova
Kazakh National Medical University named after S.D. Asfendiyarova
A prerequisite for a well-designed pilot study is randomization. The literal translation from English "random" means "made or chosen at random, random, random." The reference design of clinical trials is a randomized controlled trial.
Keywords: randomizedcontrolled research, randomization, gold standard.
Randomized controlled study- the most accurate way to identify causal relationships between treatment and the outcome of the disease, as well as to determine the cost-effectiveness of treatment. According to some reports, today about 20% of articles published in leading medical journals in the world contain the results of randomized trials. Randomization refers to a procedure that randomly assigns patients to experimental and control groups. It should be emphasized that randomization is carried out after the patient is included in the trial in accordance with the protocol of the clinical trial. Specialists dealing with this problem emphasize that random, or randomized, separation is not synonymous with random, in which the separation process defies mathematical description. Randomization is considered poorly organized when patients are divided into groups by medical history number, insurance policy, or date of birth. It is best to use a random number table, the envelope method, or a centralized computerized distribution of treatment options. Unfortunately, the mention of the randomization process does not imply correct implementation. Very often, the articles do not indicate the method of randomization, which casts doubt on the good organization of the study.
Some researchers prefer to divide patients into subgroups with the same prognosis before starting the trial and only then randomize them separately to each subgroup (stratification randomization). The correctness of stratification randomization is not recognized by everyone.
In randomized controlled trials (RCTs), participants are randomly assigned to groups using a process similar to a coin toss. Some patients fall into the experimental group (for example, the treatment group), while others fall into the control group (for example, the placebo group). Both groups are monitored over time and analyzed for outcomes reported at the start of the study (eg, death, myocardial infarction, serum cholesterol concentration, etc.). Since, on average, the groups are identical (with the exception of the intervention), in theory any change in outcome should be influenced by the intervention being studied. However, in practice, things are not so smooth.
Studies can be single-center or multicenter. It is very difficult to form a sample that is homogeneous in all prognostic signs (single-center) in one medical institution in a short time, therefore, trials often include several institutions (multicenter studies), multicenter RCTs, when studies using the same protocol are carried out in several medical centers at once. However, large multicenter clinical trials are required in the following situations:
- When the benefit of treatment is small or difficult to isolate from the spontaneous natural variability in the evolution of the disease.
- When groups of patients undergoing pharmacotherapy are heterogeneous and only for a relatively small fraction of them, pharmacotherapy will be effective.
Randomized studies can be open or blind (masked). A randomized trial is considered open if both the patient and the doctor immediately after randomization know what kind of treatment will be applied to the patient. In a blind study, the patient is not informed about the type of treatment used, and this point is discussed with the patient in advance when obtaining informed consent for the study. The doctor will know which treatment option the patient will receive after the randomization procedure. In a double-blind study, neither the doctor nor the patient knows which intervention is being applied to a particular patient. In a triple-blind study, the type of intervention is unknown to the patient, the doctor, and the researcher (statistician) who processes the study results.
Experts dealing with randomized trials note their difficulties. One of the major problems is the complexity of patient selection (usually, studies, no matter how large they are, can include only 4-8% of patients from the entire population with this disease). This leads to a decrease in the generalizability of the results to the population, i.e. the results proven in the study can only be generalized to patients identical in characteristics to those included in the randomized trials. Consequently, the results of one clinical practice cannot always be recommended for use in other settings without verification by new experimental research. It should be noted that the very principle of randomized trials does not exclude the receipt of erroneous results in the analysis and the possibility of statistical manipulations.
The results of several randomized trials on a given problem may be pooled. A quantitative analysis of the pooled results of several clinical trials of the same intervention is called meta-analysis. By increasing the sample size, meta-analysis provides more statistical power than any individual trial. It is important, however, to remember that an incorrectly conducted meta-analysis can be misleading due to the lack of comparability of patient groups and treatment settings in different studies.
RCT is the "gold standard" in medical research. However, this is only true for certain types of clinical questions. Typically all of these questions are about interventions, usually therapeutic or prophylactic measures. It should be borne in mind, however, that even with medical interventions (and especially if they are not carried out), RCTs have a number of important disadvantages.
RCT is expensive and time-consuming, so in practice:
many trials are either not conducted at all or performed on too small a group of patients or for too short a period of time;
Most trials are paid for by large research institutes, universities, government or pharmaceutical companies, which ultimately dictate the direction of research;
surrogate endpoints (indirect criteria) are often used instead of clinical outcomes.
Latent systematic errors that arise during RCTs can arise as a result of the following reasons:
imperfect randomization
the lack of randomization of all patients eligible for the study (the researcher includes in the trial only those patients who, in his opinion, will respond well to the intervention);
the researchers (contrary to the plan) are aware of which group a particular patient is in (i.e., no blinding is performed).
A clear assessment of a single variable (for example, the effect of a drug versus placebo) in a well-defined group of patients (for example, menopausal women aged 50-60)
Prospective design (i.e. data is accumulated after you decide to conduct research)
Hypothetical-deductive approach (i.e. an attempt to falsify, and not confirm your own hypothesis;)
Potential elimination of error by comparing two otherwise identical groups
Possibility of subsequent meta-analysis (combining quantitative results from several similar studies).
Summarizing what has been said, it should be noted that at present, in world practice, randomized controlled (prospective) trials with double or triple blind control are considered the "gold standard". These studies belong to the so-called class I studies. The materials of these tests and the meta-analysis carried out on their basis should be used in medical practice as the source of the most reliable information.
In order for the results of evidence-based studies to be put into practice, the categories of patients whose treatment was studied should be clearly described. Readers should compare them with the patients they have to treat. To solve this problem, a detailed description and strict adherence to the criteria for including patients in the study and exclusion from it is mandatory. It is desirable that these criteria be assessed by the means that are available in everyday practice.
BIBLIOGRAPHY
1 Brazzi L., Bertolini G., Minelli C. Meta-analysis versus randomized controlled trials in intensive care medicine // Intens. Care Med. - 2000 - Vol. 26. - P. 239-241.
2 Epstein A.E., Bigger J.T., Wyse B.J. et al. Preliminary report: Effect of encainid and flecainid on mortality in a randomized suppression after myocardial infarction // N. Engl. J. Med. 1989. Vol. 321. - P. 406-412.
3 Graf J., Doig G.S., Cook D.J., Vincent J.-L., Sibbald W.J. Randomizes, controlled clinical trials in sepsis: Has methodological quality improved over time? // Crit. Care Med.– 2002. – Vol. 30, No 2.– P. 461-472.
4 Healy D.P. New and emerging therapies for sepsis // Ann. Pharmacother. 2002. Vol. 36, No 4. - P. 648-654.
5 Hébert P.C., Cook D.J., Wells G., Marshall J. The design of randomized clinical trials in critically ill patients // Chest.– 2002.– Vol. 121.– P. 1290-1300.
6 Kanji S., Devlin J.W., Piekos K.A., Racine E. Recombinant human activated protein C, drotrecogin alfa (activated): A novel therapy for severe sepsis // Pharmacotherapy. – 2001.– Vol. 21, No. 11. - P. 1389-1402.
7 Samorodskaya I.V. Clinical trials: controlled and randomized // News of Science and Technology. Ser. The medicine. Issue Reanimatology. Intensive therapy. Anesthesiology .– 2002.– No. 2.– P. 19-22.
8 Stupakov I.N., Samorodskaya I.V. Randomized Studies - Problems and Prospects // Byull. NTSSSH them. A.N. Bakuleva RAMN - 2001.– Volume 2, No. 5.– P. 12-15.
9 Bolyakina G.K., Zaks I.O. Examples of randomized trials in intensive care (based on the materials of the journal "Critical Care Medicine" // Science and Technology News. Ser. Medicine. Issue. Reanimatology. Intensive care. Anesthesiology .– 2002.– No. 2.– P. 22-28.
A.M.Raushanova
RKZ - medicineқ zertteuler kezinde "altyn standard"
Tү yin: Zhosparlangan experimentaldyқ zertteu mindet sharty ol randomized zhurgizu. Akylshyn tilinen "random" sozbe-soz audarylymy ol "Istelgen nemese tauekeldep saylauli, kezdeison, retsiz" degen manynany bildiredi. Clinicsқ zertteu etalondyқ designs randomizirlyқ baқylanbaly zertteu.
Tү yindi withө zder: randomizirlyқ baқylanbaly zertteu, randomization, "Altyn standard".
A.M. Raushanova
RCT - "gold standard" in medical research.
Resume: Obligatory condition well-designed experimental study is to provide randomization. The literal translation of English "random" means "made or chosen at random, casual, messy." Reference design of clinical trials is a randomized controlled study.
Keywords: a randomized controlled trial, randomization, the "gold standard."