21. Neurotropic agents of central action, classification. Narcosis (general anesthesia) definition, classification of anesthetics; comparative characteristics of drugs for inhalation anesthesia. Means for non-inhalation anesthesia, their comparative characteristics. The concept of combined anesthesia and neuroleptanalgesia.
Neurotropic agents of central action, classification(?)
Sleeping pills
Antiepileptic drugs
Antiparkinsonian drugs
Painkillers (analgesics)
Analeptics
Antipsychotics
Antidepressants
Anxiolytics
Sedatives
Psychostimulants
Nootropics
Means for anesthesia
Anesthesia is an insensible, unconscious state caused by narcotic drugs, which is accompanied by a loss of reflexes, a decrease in the tone of skeletal muscles, but at the same time, the functions of the respiratory, vasomotor centers and the work of the heart remain at a level sufficient to prolong life. Anesthesia is administered by inhalation and non-inhalation route (into a vein, muscle, rectally). Inhalation anesthetic agents must meet a number of requirements: rapid onset of anesthesia and rapid exit from it without discomfort; the ability to control the depth of anesthesia; adequate relaxation of skeletal muscles; large breadth of anesthetic action, minimal toxic effects.
Anesthesia is caused by substances of various chemical structures - monatomic inert gases (xenon), simple inorganic (nitrogen oxide) and organic (chloroform) compounds, complex organic molecules (haloalkanes, ethers).
Mechanism of action of inhalation drugsGeneral anesthetics change the physicochemical properties of neuronal membrane lipids and disrupt the interaction of lipids with ion channel proteins. At the same time, the transport of sodium ions into neurons decreases, the output of less hydrated potassium ions remains, and the permeability of chloride channels controlled by GABA A receptors increases 1.5 times. The result of these effects is hyperpolarization with increased inhibition processes. General anesthetics inhibit the entry of calcium ions into neurons by blocking H-cholinergic receptors and NMDA-glutamic acid receptors; reduce the mobility of Ca 2+ in the membrane, therefore, they prevent the calcium-dependent release of excitatory neurotransmitters. The classic four stages of anesthesia cause ether:
Analgesia(3 - 8 min) Characterized by clouding of consciousness (disorientation, incoherent speech), loss of pain, then tactile and temperature sensitivity, at the end of the stage amnesia and loss of consciousness occur (depression of the cerebral cortex, thalamus, reticular formation). 2. Excitation(delirium; 1 - 3 minutes depending on the individual characteristics of the patient and the qualifications of the anesthesiologist) There are incoherent speech, motor restlessness with the patient's attempts to leave the operating table, Typical symptoms of arousal are hyperventilation, reflex secretion of adrenaline with tachycardia and arterial hypertension (operation is unacceptable.3 . Surgical anesthesia, consisting of 4 levels (comes in 10 - 15 minutes after the start of inhalation. The level of movement of the eyeballs (light anesthesia).The level of the corneal reflex (pronounced anesthesia) The eyeballs are fixed, the pupils are moderately constricted, corneal, pharyngeal and laryngeal reflexes are lost, skeletal muscle tone is reduced as a result of the spread of inhibition to the basal ganglia, brain stem and spinal cord. Pupil dilation level (deep anesthesia) Pupils dilate, react sluggishly to light, reflexes are lost, skeletal muscle tone is reduced, breathing is shallow, frequent, and becomes diaphragmatic. Awakening Functions are restored in the reverse order of their disappearance. V agonal stage breathing becomes superficial, coordination in the respiratory movements of the intercostal muscles and the diaphragm is disturbed, hypoxia progresses, the blood becomes dark in color, the pupils expand as much as possible, do not react to light. Arterial pressure falls rapidly, venous pressure increases, tachycardia develops, and heart contractions weaken. If you do not urgently stop anesthesia and do not provide emergency care, death occurs from paralysis of the respiratory center. Inhalation anesthetics are volatile liquids and gases.
Modern anesthetics - volatile liquids (halothane, enflurane, isoflurane, desflurane) are halogen-substituted derivatives of the aliphatic series. Halogens enhance the anesthetic effect. The drugs do not burn, do not explode, have a high evaporation temperature. Surgical anesthesia begins 3-7 minutes after the start of inhalation. Muscle relaxation is significant due to the blockade of H-cholinergic receptors in skeletal muscles. Awakening after anesthesia is fast (in 10-15% of patients, mental disorders, tremor, nausea, vomiting are possible). FLUOROTANE in the stage of surgical anesthesia, it depresses the respiratory center, reducing its sensitivity to carbon dioxide, hydrogen ions and hypoxic stimuli from the carotid glomeruli (blockade of H-cholinergic receptors). Violation of breathing contributes to a strong relaxation of the respiratory muscles. Fluorotan expands the bronchi as a blocker of H-cholinergic receptors of parasympathetic ganglia, which is used to stop severe attacks of bronchial asthma. Fluorotan, weakening heart contractions, reduces cardiac output by 20 - 50%. The mechanism of the cardiodepressive effect is due to the blocking of the entry of calcium ions into the myocardium. Fluorotan causes severe bradycardia, as it increases the tone of the center of the vagus nerve and directly inhibits the automatism of the sinus node (this action is prevented by the introduction of M-anticholinergics). Fluorotan causes severe hypertension due to several mechanisms: it inhibits the vasomotor center; blocks H-cholinergic receptors of the sympathetic ganglia and the adrenal medulla; has an α-adrenergic blocking effect; stimulates the production of endothelial vasodilator factor - nitric oxide (NO); reduces the minute volume of blood. A decrease in blood pressure during halothane anesthesia can be used as a controlled hypotension, however, in patients with blood loss, there is a risk of collapse, and bleeding increases during operations on organs with a rich blood supply. To stop the collapse, a selective -adrenergic agonist mezaton is injected into the vein. Norepinephrine and epinephrine, which have β-adrenomimetic properties, provoke arrhythmia. Other effects of halothane include an increase in coronary and cerebral blood flow, an increase in intracranial pressure, a decrease in oxygen consumption by the brain, despite adequate delivery of oxygen and oxidation substrates with blood; Fluorotan has hepatotoxicity, as it is converted in the liver into free radicals - initiators of lipid peroxidation, and also forms metabolites (fluoroethanol), covalently binding to biomacromolecules. The frequency of hepatitis is 1 case per 10,000 anesthesia in adult patients. ENFLURAN and ISOFLURANE Both drugs strongly depress breathing (during anesthesia, artificial ventilation of the lungs is required), disrupt gas exchange in the lungs, expand the bronchi; cause arterial hypotension; relax the uterus do not damage the liver and kidneys. DESFLURAN evaporates at room temperature, has a pungent odor, strongly irritates the respiratory tract (risk of coughing, laryngospasm, reflex respiratory arrest). Depresses respiration, causes arterial hypotension, tachycardia, does not change blood flow in the brain, heart, kidneys, increases intracranial pressure.
GAS ANESTHESIS Nitrous oxide is a colorless gas, stored in metal cylinders under a pressure of 50 atm in a liquid state, does not burn, but supports combustion, is poorly soluble in blood, but dissolves well in lipids of the central nervous system, so anesthesia occurs very quickly. To obtain deep anesthesia of nitrogen, nitrous oxide is combined with inhalation and non-inhalation anesthetics and muscle relaxants. Application: for induction anesthesia (80% nitrous oxide and 20% oxygen), combined and potentiated anesthesia (60 - 65% nitrous oxide and 35 - 40% oxygen), anesthesia for childbirth, trauma, myocardial infarction, acute pancreatitis (20% nitrous oxide ). Contraindication for hypoxia and severe lung diseases, accompanied by a violation of gas exchange in the alveoli, with severe pathology of the nervous system, chronic alcoholism, alcohol intoxication (danger of hallucinations, arousal). Do not use for pneumoencephalography and operations in otorhinolaryngology.
Xenonit is colorless, does not burn and has no smell, when in contact with the oral mucosa, it creates a sensation of a bitter metallic taste on the tongue. It has a low viscosity and high lipid solubility, it is excreted by the lungs unchanged. The mechanism of the anesthetic effect is the blockade of cytoreceptors of excitatory neurotransmitters - H-cholinergic receptors, NMDA glutamic acid receptors, as well as activation of receptors for the inhibitory neurotransmitter glycine. Xenon exhibits antioxidant and immunostimulant properties, reduces the release of hydrocortisone and adrenaline from the adrenal glands. Anesthesia with xenon (80%) mixed with oxygen (20%)
Awakening after the cessation of xenon inhalation is quick and pleasant, regardless of the duration of anesthesia. Xenon does not cause significant changes in the pulse, the strength of heart contractions, at the beginning of inhalation it increases cerebral blood flow. Xenon can be recommended for anesthesia in patients with a compromised cardiovascular system, in pediatric surgery, during painful manipulations, dressings, for labor pain relief, relief of painful attacks (angina pectoris, myocardial infarction, renal and hepatic colic). Anesthesia with xenon is contraindicated in neurosurgical operations.
Non-inhalation anesthetics are injected into a vein, into muscles and intraosseously .
non-inhalation anesthetics are divided into three groups: Short acting preparations (3 - 5 min)
· PROPANIDIDE(SOMBREVIN)
· PROPOFOL (DIPRIVAN, RECOFOL)
Intermediate-acting preparations (20 - 30 min)
· KETAMINE(CALYPSOL, KETALAR, KETANEST)
· MIDAZOLAM(DORMIKUM, FLORMIDAL)
· HEXENAL(HEXOBARBITAL-SODIUM)
· THIOPENTAL-SODIUM (PENTOTAL) Long-acting drugs (0.5 - 2 hours)
· SODIUM OXYBUTYRATE
PROPANIDIDE- an ester, chemically similar to novocaine. When injected into a vein, it has an anesthetic effect for 3-5 minutes, as it undergoes rapid hydrolysis by blood pseudocholinesterase and is redistributed into adipose tissue. It blocks the sodium channels of neuronal membranes and disrupts depolarization. Turns off consciousness, in subnarcotic doses it has only a weak analgesic effect.
Propanidide selectively stimulates the motor areas of the cortex, and therefore causes muscle tension, tremors, and increases spinal reflexes. Activates the vomiting and respiratory centers. During anesthesia with propanidide, hyperventilation is observed in the first 20–30 s, which is replaced by respiratory arrest for 10–15 s due to hypocapnia. Weakens heart contractions (until cardiac arrest) and causes arterial hypotension by blocking β - adrenergic receptors of the heart. When prescribing propanidide, there is a risk of allergic reactions due to the release of histamine (anaphylactic shock, bronchospasm). Cross-allergy with novocaine is possible.
Propanidide is contraindicated in shock, liver disease, kidney failure, is used with caution in violation of coronary circulation, heart failure, arterial hypertension.
PROPOFOL.He is the antagonistNMDAglutamic acid receptors, enhances GABAergic inhibition, blocks voltage-dependent calcium channels of neurons. It has a neuroprotective effect and accelerates the recovery of brain functions after hypoxic damage. Inhibits lipid peroxidation, proliferation T-lymphocytes, their release of cytokines, normalizes the production of prostaglandins. In the metabolism of propofol, an extrahepatic component plays a significant role, inactive metabolites are excreted by the kidneys.
Propofol induces anesthesia after 30 seconds. Severe pain is possible at the injection site, but phlebitis and thrombosis are rare. Propofol is used for induction anesthesia, maintaining anesthesia, providing sedation without turning off consciousness in patients who are undergoing diagnostic procedures and intensive care.
During the induction of anesthesia, skeletal muscle twitches and convulsions sometimes appear, respiratory arrest develops within 30 s, due to a decrease in the sensitivity of the respiratory center to carbon dioxide and acidosis. Oppression of the respiratory center is potentiated by narcotic analgesics. Propofol, by dilating the peripheral vessels, briefly lowers blood pressure in 30% of patients. Causes bradycardia, reduces cerebral blood flow and oxygen consumption by brain tissue. Awakening after anesthesia with propofol is fast, occasionally there are convulsions, tremors, hallucinations, asthenia, nausea and vomiting, increased intracranial pressure.
Propofol is contraindicated in allergies, hyperlipidemia, disorders of cerebral circulation, pregnancy (penetrates the placenta and causes neonatal depression), children under the age of one month. Anesthesia with propofol is carried out with caution in patients with epilepsy, pathology of the respiratory, cardiovascular systems, liver and kidneys, hypovolemia.
KETAMINEcauses anesthesia when injected into a vein for 5-10 minutes, when injected into muscles - for 30 minutes. There is experience of epidural use of ketamine, which prolongs the effect up to 10-12 hours. The metabolite of ketamine - norketamine has an analgesic effect for another 3-4 hours after the end of anesthesia.
Anesthesia with ketamine is called dissociative anesthesia: the anesthetized person has no pain (it is felt somewhere to the side), consciousness is partially lost, but reflexes are preserved, and the tone of skeletal muscles increases. The drug disrupts the conduction of impulses along specific and non-specific pathways to the associative zones of the cortex, in particular, interrupts the thalamo-cortical connections.
The synaptic mechanisms of action of ketamine are diverse. It is a non-competitive antagonist of the excitatory brain mediators glutamic and aspartic acids in relation to NMDA-receptors ( NMDA-N-methyl- D-aspartate). These receptors activate sodium, potassium, and calcium channels in neuronal membranes. When the receptors are blocked, depolarization is disturbed. In addition, ketamine stimulates the release of enkephalins and β-endorphin; inhibits neuronal uptake of serotonin and norepinephrine. The latter effect is manifested by tachycardia, an increase in blood pressure and intracranial pressure. Ketamine dilates the bronchi.
When leaving ketamine anesthesia, delirium, hallucinations, and motor agitation are possible (these adverse events are prevented by the introduction of droperidol or tranquilizers).
An important therapeutic effect of ketamine is neuroprotective. As is known, in the first minutes of brain hypoxia, excitatory mediators, glutamic and aspartic acids, are released. Subsequent activation NMDA receptors, increasing
in the intracellular environment, the concentration of sodium and calcium ions and osmotic pressure cause swelling and death of neurons. Ketamine as an antagonist NMDA-receptors eliminates the overload of neurons with ions and the associated neurological deficit.
Contraindications to the use of ketamine are cerebrovascular accidents, arterial hypertension, eclampsia, heart failure, epilepsy and other convulsive diseases.
MIDAZOLAM- non-inhalation anesthetic benzodiazepine structure. When injected into a vein, it causes anesthesia within 15 minutes; when injected into muscles, the duration of action is 20 minutes. It acts on benzodiazepine receptors and allosterically enhances the cooperation of GABA with GABA receptors of the type A. Like tranquilizers, it has muscle relaxant and anticonvulsant effects.
Anesthesia with midazolam is carried out only with artificial ventilation of the lungs, since it significantly depresses the respiratory center. This drug is contraindicated in myasthenia gravis, circulatory failure, in the first 3 months. pregnancy.
Barbiturates HEXENAL and THIOPENTAL-SODIUM after injection into a vein, they cause anesthesia very quickly - “at the end of the needle”, the anesthetic effect lasts 20-25 minutes.
During anesthesia, reflexes are not completely suppressed, the tone of skeletal muscles increases (N-cholinomimetic effect). Intubation of the larynx without the use of muscle relaxants is unacceptable due to the risk of laryngospasm. Barbiturates do not have an independent analgesic effect.
Barbiturates depress the respiratory center, reducing its sensitivity to carbon dioxide and acidosis, but not to reflex hypoxic stimuli from the carotid glomeruli. Increase the secretion of bronchial mucus, independent of cholinergic receptors and not eliminated by atropine. Excite the center of the vagus nerve with the development of bradycardia and bronchospasm. They cause arterial hypotension, as they inhibit the vasomotor center and block the sympathetic ganglia.
Hexenal and thiopental-sodium are contraindicated in diseases of the liver, kidneys, sepsis, fever, hypoxia, heart failure, inflammatory processes in the nasopharynx. Geksenal is not administered to patients with paralytic ileus (strongly inhibits motility), thiopental sodium is not used for porphyria, shock, collapse, diabetes mellitus, bronchial asthma.
Non-inhalation anesthetics are used for induction, combined anesthesia and independently for short-term operations. In outpatient practice, propanidide, which does not have an aftereffect, is especially convenient. Midazolam is used for premedication, and is also administered orally as a hypnotic and tranquilizer.
SODIUM OXYBUTYRATE (GHB) when injected into a vein causes anesthesia after 30 - 40 minutes for a duration of 1.5 - 3 hours.
This drug turns into a GABA mediator, which regulates inhibition in many parts of the central nervous system (cerebral cortex, cerebellum, caudate nucleus, pallidum, spinal cord). GHB and GABA reduce the release of excitatory mediators and increase postsynaptic inhibition by affecting GABA A receptors. Under anesthesia with sodium oxybutyrate, reflexes are partially preserved, although strong muscle relaxation occurs. Relaxation of skeletal muscles is due to the specific inhibitory effect of GABA on the spinal cord.
Sodium oxybutyrate does not inhibit the respiratory, vasomotor centers, heart, moderately increases blood pressure, sensitizing α-adrenergic receptors of blood vessels to the action of catecholamines. It is a strong antihypoxant in the brain, heart, retina.
Sodium oxybutyrate is used for induction and basic anesthesia, labor pain relief, as an anti-shock agent, in the complex therapy of hypoxia, including cerebral hypoxia. It is contraindicated in myasthenia gravis, hypokalemia, it is prescribed with caution in toxicosis of pregnant women, accompanied by arterial hypertension, as well as in people whose work requires rapid mental and motor reactions.
COMBINED ANESTHESIA (multicomponent)
|
A combination of two or more anesthetics (eg, hexenal and ether; hexenal, nitrous oxide and ether). Currently, in most cases, combined general anesthesia is performed, which is safer for the patient and more convenient for the surgeon in terms of performing the operation. The combination of several anesthetics improves the course of anesthesia (disturbances in breathing, gas exchange, blood circulation, liver, kidney and other organs are less pronounced), makes anesthesia more manageable, eliminates or significantly reduces the toxic effect on the body of each of the drugs used. |
Neuroleptanalgesia (Greek neuron nerve + lepsis grasping, attack + Greek negative prefix ana- + algos pain) is a combined method of intravenous general anesthesia, in which the patient is conscious, but does not experience emotions (neurolepsy) and pain (analgesia). Due to this, protective reflexes of the sympathetic system are turned off and the need for oxygen in tissues decreases. The advantages of neuroleptanalgesia also include: a large breadth of therapeutic action, low toxicity and suppression of the gag reflex. Anesthesia is an insensible, unconscious state caused by narcotic drugs, which is accompanied by a loss of reflexes, a decrease in skeletal muscle tone, but at the same time, the functions of the respiratory, vasomotor centers and the work of the heart remain at a level sufficient to prolong life.
Lecture 12. neurotropic drugs
Drugs for anesthesia.
Alcohols.
Sleep aids.
Antipsychotics and tranquilizers
Sedatives.
Narcotic analgesics.
Non-narcotic analgesics
Anticonvulsants.
General characteristics and classification of CNS stimulants.
Caffeine group (psychostimulants).
CNS stimulating plants.
Camphor and its substitutes
Strychnine group.
Literature:
Subbotin V.M., Subbotina S.G., Aleksandrov I.D. Modern drugs in veterinary medicine. / Series “Veterinary and animal husbandry”, Rostov-on-Don: “Phoenix”, 2000. - 592 p.
Pharmacology / V.D. Sokolov, M.I. Rabinovich, G.I. Gorshkov and others. Under. ed. V.D. Sokolov. - M. : Kolos, 1997. - 543 p.
I.E. Brain. Pharmacology. - M. : Agropromizdat, 1985. - 445 p.
D.K. Chervyakov, P.D. Evdokimov, A.S. Vishker. Medicines in veterinary medicine. - M. : Kolos, 1977. - 496 p.
M.I. Rabinovich. Workshop on veterinary pharmacology and formulation. - M. : Agropromizdat, 1988. - 239 p.
5. M.D. Mashkovsky. Medicines. - Moscow: "New Wave", 2000 volume 1 - 530 p., volume 2 - 608 p.
6. D.A. Kharkevich. Pharmacology. - M. : Medicine, 2004. - 735 p.
7. V.N. Zhulenko, O.I. Volkova, B.V. Usha et al. General and clinical veterinary formulation. - M. : Kolos, 1998. - 551 p.
8. I.F. Klenova, N.A. Eremenko. Veterinary drugs in Russia. Directory. - Selkhozizdat, 2000. - 543 p.
9. Teaching aid for students' independent work on general and private pharmacology / Tolkach N.G., Arestov I.G. Golubitskaya A.V., Zholnerovich Z.M. and others - Vitebsk, 2000. -37 p.
10.Modern pharmacological agents and methods of their application: teaching aid for private pharmacology. /Tolkach N.G., Arestov I.G., Golubitskaya A.V. and others - Vitebsk 2001 - 64 p.
12. M.D. Mashkovsky. Medicines. M.: "New wave", 2005 - 1015 p.
13. Medicines in veterinary medicine. Directory. Yatusevich A.I., Tolkach N.G., Yatusevich I.A. and others. Minsk, 2006. -
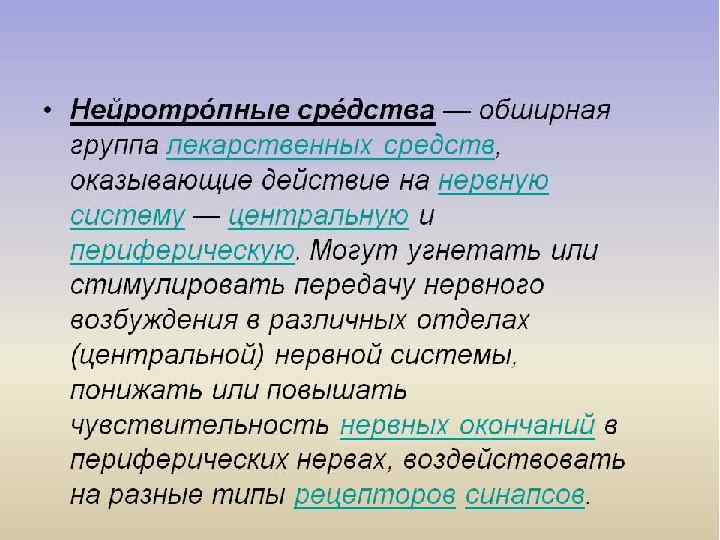
General characteristics and classification of neurotropic drugs.
Drugs for anesthesia.
Alcohols.
Sleep aids.
General characteristics and classification of neurotropic drugs.
A significant section of private pharmacology is devoted to drugs that affect the nervous regulation of body functions. With the help of such substances, it is possible to influence the transmission of excitation at different levels of the central nervous system, as well as in the afferent and efferent pathways of peripheral innervation.
The classification of neurotropic drugs is based on the localization of their action. This refers to their effect on the central or peripheral nervous system.
The central nervous system regulates all activities of the body. For the central nervous system, 2 main physiological processes are inherent: excitation and inhibition. Depending on the ratio of these processes, several types of nervous activity are distinguished. In this regard, all drugs that regulate the functions of the central nervous system are divided into:
I. Means that depress the central nervous system.
1. Means for anesthesia (general anesthetics);
2. Sleeping pills;
3. Alcohols;
4. Painkillers (analgesics):
* non-narcotic analgesics;
* narcotic analgesics,
5. Anticonvulsants;
6. Sedatives;
7. Antipsychotics and tranquilizers.
II. Stimulants (stimulating the central nervous system):
1. Caffeine group;
2. Camphor group;
3. Strychnine group;
4. Plants stimulating the central nervous system.
III. Drugs affecting the peripheral part of the nervous system.
1. Means that affect efferent innervation:
* funds that affect cholinergic synapses;
* funds that affect adrenergic synapses.
2. Means affecting the afferent innervation:
* funds that reduce the sensitivity of afferent nerves;
* Means that increase the sensitivity of afferent nerves.
Send your good work in the knowledge base is simple. Use the form below
Students, graduate students, young scientists who use the knowledge base in their studies and work will be very grateful to you.
Posted on http://www.allbest.ru/
Neurotropic drugs
It should be recalled that in private pharmacology, the issues of pharmacodynamics and pharmacokinetics are presented in relation to specific groups of drugs and the most important drugs for practical medicine.
We will begin the study of private pharmacology with drugs that affect the nervous regulation of body functions. With the help of such means, it is possible to influence the transmission of excitation at different levels of the central nervous system, as well as in the afferent (sensory) and efferent (executive) pathways of peripheral innervation. This large group of funds is called NEUROTROPIC MEDIA, that is, funds whose action is directed to the nervous system.
Based on the structural and functional features of different parts of the reflex arc, neurotropic agents are divided into 2 huge groups:
1) neurotropic agents that affect (regulate) the functions of the peripheral part of the nervous system;
2) neurotropic agents that regulate the functions of the central nervous system. In turn, the first group of agents that affect the function of the reef link of the nervous system is divided into 2 subgroups:
a) drugs that affect afferent innervation, that is, centripetal nerve fibers, through which excitation is transmitted from tissues to the central nervous system (lat. - afferens - bringing);
b) drugs that affect efferent innervation (from lat. -efferens - carrying out), that is, affecting centrifugal nerve fibers, through which excitation is transmitted from the central nervous system to tissues.
Let's start the presentation of the material with the means that affect the afferent innervation. drug neurotropic afferent innervation
Classification of drugs affecting afferent innervation
Excitation from the periphery to the center, to the central nervous system, is transmitted by sensory nerves. Therefore, the means acting on the afferent innervation are also divided into 2 groups:
1) means that depress the sensitivity of afferent nerves; these include:
a) local anesthetics;
b) binders;
c) enveloping (and emollient);
d) adsorbents;
2) means that excite afferent nerves, that is, of the current type, or rather, means that selectively excite the endings of the sensory nerves of the skin or mucous membranes. These are the following subgroups:
a) irritants;
b) respiratory stimulants of reflex action; c) expectorant reflex action; d) bitterness; e) laxatives; e) choleretic reflex action. Let's start the analysis of medicines that reduce the sensitivity of afferent nerves or prevent their excitation with ANESTHETIC MEDICINES or LOCAL ANESTHETICS. Local anesthetics (anaesthetica localica) are drugs that reduce pain sensitivity at the site of their application. Since anesthetics (from the Greek - anaesthesva - insensibility) cause local loss of sensation, they are called local anesthetics.
The sequence of action of this class of drugs is as follows: first of all, they eliminate the feeling of pain, when the anesthesia deepens, the temperature is turned off, then tactile sensitivity, and lastly, reception to touch and pressure (deep sensitivity). The most important property of local anesthetics is that they act reversibly and with the preservation of consciousness.
By acting on the endings of sensory nerves, local anesthetics prevent the generation and conduction of excitation. The mechanism of action of local anesthetics, according to molecular mechanics, is currently associated with the fact that, by binding to membrane structures, they stabilize the membranes of nerve cells, thereby blocking the permeability of their membranes for Na and K ions. This prevents the emergence and development of the potential actions, and, consequently, the conduction of impulses. The data obtained by molecular mechanics methods show that the biological activity of local anesthetics largely depends on their polarizability, ionization potential, molecular conformation, and electric charge of the molecule. From the modern standpoint, the mechanism of action is associated with the formation of a complex of the local anesthetic drug with the membrane Na-channel receptor, as a result of which the flow of Na ions is blocked.
According to the CHEMICAL STRUCTURE, local anesthetics (synthetics) are divided into 2 groups:
a) esters (esters) of aromatic acids (novocaine, dicaine, anesthesin-PABA esters, cocaine - benzoic acid ester);
b) substituted amino acid amides (lidocaine, trimecaine, pyromecaine, mepivacaine, bupivacaine).
If esters are metabolized by esterases, then the metabolism of amides mainly occurs in the liver. comes out
The benefits of amides:
Longer period of action;
Non-allergens;
Do not weaken the action of sulfonamides.
The active principle of local anesthetics are bases (due to the presence of nitrogen in the amine group), which form soluble salts with acids. Bases are poorly soluble. In tissues with an alkaline environment (pH = 7.4), the free base is released and has a pharmacological effect. All drugs are produced in the form of salts, mainly in the form of hydrochlorides. In an acidic environment, the base is not cleaved off and the action of local anesthetics is not manifested.
There are a number of requirements for anesthetics. First of all, they must have:
1) high selectivity of action, without causing an irritating effect either on the nerve elements or on the surrounding tissues;
2) have a short latent period;
3) high activity with different types of local anesthesia;
4) a certain duration of action, convenient for a variety of manipulations.
5) It is desirable that they: narrow the vessels or at least not expand them. Vasoconstriction enhances anesthesia, reduces bleeding from tissues, and reduces toxic effects. Among the most important requirements for local anesthetics, they also include:
6) Low toxicity and minimal side effects. Preparations should also well:
7) Dissolve in water and not break down during sterilization.
Local anesthetics are used to obtain different types of anesthesia, the main types of which are the following:
1) Terminal, terminal or surface anesthesia - an anesthetic is applied to the surface of the mucous membrane. In addition, the anesthetic can be applied to the wound, ulcerative surface. A typical example of this type of anesthesia is a small foreign body in the eye (mote) - when it is removed, a dicaine solution is instilled into the conjunctival cavity. Terminal anesthesia can be performed mainly on the mucous membranes, since the skin is practically impervious to local anesthetics. For terminal anesthesia, solutions of cocaine (2% - 5 ml), dicaine (0.5% - 5 ml), lidocaine (1-2% solution), pyromecaine (0.5-1-2%), and also anesthesin (powder, tablets, ointment, suppositories).
2) The second type of anesthesia is infiltration. This type of anesthesia involves the sequential "impregnation" of the skin and deeper tissues through which the surgical incision will pass. A typical example is layer-by-layer infiltration anesthesia of tissues during appendectomy. For infiltration anesthesia, solutions of novocaine (0.25-0.5%), trimecaine (0.125-0.25-0.5%), lidocaine (0.25-0.5%) are used.
3) The third type of anesthesia - conduction or regional (regional) - the anesthetic is injected along the nerve; there is a block in the conduction of excitation along the nerve fibers, which is accompanied by a loss of sensitivity in the area innervated by them. A typical example of conduction anesthesia is the operation of extraction (removal) of a tooth. Solutions of novocaine (1-2%), trimecaine (1-2%), lidocaine (0.5-2%) are used for this type of anesthesia.
4) Varieties of conduction anesthesia are spinal anesthesia, when the anesthetic is administered subarachnoidly, as well as epidural anesthesia, in which the anesthetic is injected into the space above the dura mater. With these types of anesthesia, the drug acts on the anterior and posterior roots of the spinal cord, blocking the innervation of the lower half of the body. For these types of anesthesia, even more concentrated solutions of local anesthetics are used: novocaine (5%), lidocaine (1-2%), trimecaine (5%).
The first local anesthetic used in medical practice was cocaine, an alkaloid from the coconut shrub Erythroxylon coca (which grows in South America). Cocaine hydrochloride salt is used (Cocaini hydrochloridum 1-3% in the conjunctival cavity, 2-5% - anesthesia of the mucous membranes), which is the hydrochloride of the ester of benzoic acid and methylecgonine. The chemical structure of cocaine is close to atropine. Known hundreds of years ago. The natives of Chile, Peru, Bolivia chewed the leaves of the Erythroxylon coca tree to ease hunger and fatigue and induce a surge of strength, and the Peruvians still use it. In 1860, Niemann isolated cocaine from the leaves of this tree, and in 1884, Karl Koller used it to anesthetize the eyes. In 1902, Wilstetter established the structure of cocaine and carried out its synthesis. It turned out that cocaine has at least two negative properties, namely, significant toxicity and the ability to cause addiction in patients. At the same time, unlike heroin or morphine, cocaine develops a mental rather than a physical addiction. The high toxicity of cocaine severely limits its use. At the same time, cocaine is a very effective local anesthetic.
In view of the toxicity of the drug, its use even for superficial anesthesia should be cautious, especially in children. This is due to the fact that cocaine can be absorbed from the mucous membranes and have a toxic effect. Due to its high toxicity, cocaine is used primarily in eye, nose and throat surgery; in dentistry is part of the arsenic paste. It is a surface anesthetic for local anesthesia of the conjunctiva and cornea (1-3%), mucous membranes of the oral cavity, nose, larynx (2-5%), for anesthesia of the dental pulp. When instilling 1-3% solutions of cocaine into the cavity of the conjunctiva, there is a pronounced anesthesia of the latter, lasting about 1 hour. In this case, cocaine constricts the vessels of the sclera, dilates the pupil. Intraocular pressure decreases, however, in some individuals, intraocular pressure rises sharply (especially in the elderly). With prolonged use, cocaine causes desquamation and ulceration of the corneal epithelium. The danger of phenomena of general intoxication requires its combination with adrenaline. Cocaine is part of the drops for the treatment of patients with rhinitis, sinusitis, conjunctivitis. In the criminal world, cocaine is known as "marafet". Now in the West, an even stronger and cheaper semi-synthetic drug "Krek" has appeared.
Chronic use of cocaine by inhalation through the nose causes ulceration of the nasal mucosa. Earlier, before the advent of more modern drugs, cocaine addicts were recognized by ulceration of the nasal mucosa (vasospasm). With a resorptive effect, cocaine stimulates the central nervous system (euphoria, anxiety, psychomotor agitation, a feeling of fatigue, there may be hallucinations). Allergic reactions are often observed.
The next drug used for superficial anesthesia is Dicain (Dicainum) - an even stronger drug (about 10 times stronger than cocaine), but also 2-5 times more toxic than cocaine. Dikain is a derivative of para-aminobenzoic acid. Due to toxicity, it is used only for terminal anesthesia in ophthalmic practice (0.25-2% solutions). Pupils do not dilate, intraocular pressure does not decrease, does not affect accommodation. In dentistry, dikain is part of Platonov's liquid, which is used to anesthetize the hard tissues of the tooth. In ENT practice, 0.5-1% anesthetic solutions are used. In a surgical clinic, dikain is used to lubricate various bougies, catheters, and during endoscopic manipulations.
Dikain dilates blood vessels, so it is advisable to combine it with adrenomimetics (with adrenaline, for example). It is well absorbed through the mucous membranes, so even a slight excess of therapeutic doses can have a severe toxic effect (up to death). In children, with a special friability of their mucosa, severe toxic effects are possible (up to 10 years - cannot be used at all).
Unlike cocaine and dicaine, the para-aminobenzoic acid derivative ANESTHESIN (Anaesthesinum) is poorly soluble in water. This is due to the fact that anestezin does not give salts, since it exists only as a base. Due to the insolubility of anestezin, it exists in dry form, in the form of a powder. Therefore, it is used externally in the form of powders, pastes, 5% ointments for terminal anesthesia. In dentistry, they are used in the form of 5-10% ointments, 5-20% oil solutions (glossitis, stomatitis), powders are rubbed for anesthesia of hard tooth tissues (anesthesia of solids). These dosage forms are applied to the affected skin surface with abrasions, frostbite, urticaria, skin itching. Anestezin can also be used enterally in the form of tablets (0.3 each), powders, mixtures with mucus to provide terminal anesthesia of the gastric mucosa (peptic ulcer, gastritis), administered rectally (candles containing 0.05-0.1 anestezin) for diseases rectum (hemorrhoids, fissures).
A unique dosage form has been created - an aerosol called AMPROVISOL, which includes anesthesin, menthol, vitamin D - ergocalciferol, glycerin. The drug promotes the healing of ulcers, stimulating the processes of reparation
Very often anestezin is a part of suppositories used for rectal fissures, hemorrhoids.
For surface anesthesia, the drug PYROMECAINE (bumecaine) is also used. It is used in ophthalmology (0.5% -1%), otorhinolaryngology (1-2%), dentistry (1-2%). Pyromecaine has an antiarrhythmic effect, which makes it possible to use it as an antiarrhythmic agent in the clinic of internal diseases. Used as an anesthetic in endoscopic procedures (bronchoscopy, bronchography, intubation). Available in ampoules of 10, 30 and 50 ml of a 1-2% solution, in the form of a 5% ointment and gel. It is used only for terminal anesthesia, as it has an irritating effect on tissues due to the high pH value (4, 4-5, 4).
NOVOCAINE (Novocainum) is an ester of diethylaminoethanol and para-aminobenzoic acid. Produced in ampoules of 1, 2, 5, 10, 20 ml 0.25% concentration, in a bottle, bottles of 200 ml (0.25%), in the form of an ointment, suppositories. Novocaine is one of the oldest local anesthetics. Has moderate activity and duration of action. The duration of infiltration anesthesia is on average 30 minutes. Novocaine is used mainly for infiltration and conduction anesthesia. For infiltration anesthesia, novocaine is used in low concentrations (0.25-0.5%) and in large volumes (hundreds of ml). For conduction anesthesia, the volume of the anesthetic solution is significantly less, but its concentration increases (12% in a volume of 5, 10, 20 ml). Novocaine is used for spinal anesthesia, even less often for terminal anesthesia (large doses are needed).
The big advantage of novocaine is its low toxicity. Novocaine has a scope in therapy: it has a slight ganglioblocking effect, reducing the release of acetylcholine from preganglionic fibers. In this regard, as well as as a result of the depressant effect on the central nervous system, the excitability of the motor zones of the cortex decreases, and the effect of agents that depress the central nervous system is potentiated. It has a hypotensive effect, as well as a weak antiarrhythmic. Reduces spasm of smooth muscles. As an antiarrhythmic agent, a novocaine derivative, NOVOCAINOMIDE, is more often used in therapy. Of the side effects, one should point out its antagonistic effect with chemotherapeutic drugs, namely with sulfonamides. This is due to the competitive action of the metabolite of novocaine - paraaminobenzoic acid - with sulfonamides (PABA is a competitor to sulfonamides).
Particular attention should be paid to the possibility of intolerance to the drug: allergic reactions can often occur, up to anaphylactic shock. An allergic history is required. Frequent allergic reactions of novocaine are again associated with its chemical structure, since, if ether derivatives often cause allergic reactions (amide compounds are much less common). More than 4% of people are highly sensitive to novocaine, this is the most allergenic drug. In addition, novocaine cannot be used for anesthesia of inflamed tissues, since in an acidic environment it does not have an anesthetic effect (does not dissociate).
LIDOCAINE (Lidocainum). Release form: amp. - 10, 20 ml - 1%, 2, 10 ml - 2%; in aerosols - 10%; dragee 0.25 each. Abroad - KSIKAIN (lidestin, ultracain). It is a general purpose local anesthetic used for almost all types of anesthesia. It is indicated for superficial, infiltration, conduction, epidural, subarachnoid and other types of anesthesia.
In terms of anesthetic activity, it surpasses novocaine by 2.5 times and acts 2 times longer (about 60 minutes). In combination with adrenomimetics, it exhibits an anesthetic effect for 2-4 hours (0.5% solution; 1 drop of adrenaline per 10 ml). There is a drug Xylonor, which is a combination of xicaine and norepinephrine. This commercial preparation cannot be used for terminal anesthesia.
Its toxicity is approximately the same as that of novocaine or slightly exceeds it. Does not irritate tissues. When instilled into the cavity of the conjunctiva, it does not affect the size of the pupil and vascular tone.
Its valuable quality is the fact that neither lidocaine (xicaine) nor its metabolites enter into a competitive relationship with sulfonamides. In addition, lidocaine rarely causes allergic reactions, unlike novocaine. The drug is stable, it can be stored for a long time at room temperature, as well as autoclaved.
Of the other positive qualities of lidocaine, its high activity as an antiarrhythmic agent should be noted. As an antirhythmic, it is currently considered the leading drug for ventricular forms of arrhythmias (extrasystole, tachycardia). Unfortunately, in view of the small output of it by our industry, it represents a certain deficit.
Side effects: hypotension, drowsiness, dizziness, amnesia, convulsions, tremor, toxic tachyarrhythmia, visual impairment, respiratory failure. There may be allergic reactions (bronchospasm, urticaria, dermatitis).
OTHER DRUGS IN THE GROUP OF SUBSTITUTED AMIDES. ARTIKAIN is a local anesthetic for infiltration, conduction, spinal anesthesia. It is used in the form of 2% and 5% solutions. The drug is a combination with the vasoconstrictor glucose. The duration of action is about 4 hours.
Used as a local anesthetic in surgery as well as obstetric clinic
Bupivacaine (marcaine) is a drug for long-term anesthesia (8 hours). It is the longest acting local anesthetic. Apply in the form of 0, 25%; 0.5%; 0.75% solutions with adrenaline. One of the most active, strong local anesthetics (4 times more powerful than lidocaine). It is used for infiltration, conduction and epidural anesthesia in obstetric and surgical practice in the postoperative period, with chronic pain syndrome. It is a drug with a slow onset of action, the maximum effect is created only after 30 minutes.
Side effects - convulsions, decreased heart activity.
Mepivacaine (Mepivacainum). 1%, 2%, 3% solutions are used for infiltration and conduction anesthesia, including spinal anesthesia. It is very similar in chemical structure to the bupivocaine molecule (differences are associated with only one radical). It is a local anesthetic with an average duration of action (up to 2 hours). Has a fast onset effect. The rest is similar to the previous preparation.
SCANDICAIN - used in dentistry in the form of a 1% solution.
ULTRAKAIN - see reference book. An overdose of local anesthetics can lead to poisoning.
As a rule, intoxication with local anesthetics is realized by generalized convulsions. In this case, the introduction of diazepan (seduxen), which is the best anticonvulsant, is necessary. In case of depression of the centers of respiration and blood circulation, it is necessary to use CNS stimulants (analeptics such as bemegrid, etimizol), and possibly artificial respiration against the background of the introduction of adrenomimetics (adrenaline, ephedrine).
Astringents (ADSTRINGENTIA)
Astringents are classified as anti-inflammatory or antiphlogistic (from the Greek - phlogizo - I ignite) topical preparations. They are used in inflammatory processes of the mucous membranes and skin.
The mechanism of action of astringents is due to the fact that at the site of application of these drugs there is a compaction of colloids ("partial coagulation" of proteins) of extracellular fluid, mucus, exudate, cell surfaces (membranes), vessel walls. The permeability of the latter, the degree of inflammation decreases, and the film formed as a result of this compaction protects the endings of sensory nerves from irritation and the feeling of pain weakens. In addition, there is a limitation of reflexes from receptors that support the pathological process.
Astringents by origin are divided into 2 groups:
1) ORGANIC (of vegetable origin);
2) INORGANIC (metal salts).
Otherwise, astringents are sometimes classified:
a) vegetable origin;
b) preparations - metal salts.
ORGANIC include TANIN (Taninum), which is an alkaloid of bird cherry, tea. Alkaloids are substances that have the properties of bases, and contain nitrogen in their chemical structure. There is a lot of tannin in oak bark, sage, chamomile, St. Infusions and decoctions are prepared from these plants. In addition, tannin is prescribed in the form of solutions for external use and ointments. Solutions for rinsing the mouth, nose, pharynx, larynx - 1-2%, and 3-10% ointment is used to lubricate the affected surfaces (for burns, bedsores, cracks).
Of the NON-ORGANIC astringents, preparations that are metal salts are of interest: LEAD (lead acenate), BISMUTH (basic bismuth nitrate) or BISMUTH SUBNITRATE (Vismuthi subnitras), DE-NOL (colloidal bismuth subcitrate), ALUMINUM (alum), DERMATOL (basic bismuth salt), ZINC (zinc oxide and zinc sulfate), COPPER (copper sulfate), SILVER (silver nitrate - Argento nitras).
Astringents have the following pharmacological effects:
1) astringent; at the same time, at low concentrations, the salts of these metals have an astringent effect, and at higher concentrations, they have a cauterizing effect;
2) anti-inflammatory; this effect of astringents is also due to the fact that reflexes that support pathological processes are limited;
3) analgesic;
4) to some extent detoxifying.
INDICATIONS FOR USE.
Astringents are prescribed for inflammation of the oral mucosa, stomatitis of various genesis, gingivitis, in the form of lotions, rinses, douches, lubrications, powders. A feature of astringents is their antimicrobial activity, and in this regard, new bismuth preparations, in particular De-nol, are of main interest. Astringents can sometimes be administered orally - the same preparations of bismuth (De-nol), bismuth is used as a powder, and in combined tablets - vikalin, vikair - is used orally for gastritis, gastric ulcer, duodenal ulcer. In addition, bismuth preparations are also used as a powder (Dermatol). The protein preparation of tannin - TANALBIN - is also prescribed inside for inflammation of the gastrointestinal mucosa (enteritis, colitis), as well as infusions and decoctions of bird cherry fruits, chamomile flowers. Tannin solutions are used topically for burns and administered orally for poisoning with salts of heavy metals, alkaloid salts, glycosides (they contribute to their precipitation).
COATING AGENTS (MACILAGINOSA) are indifferent substances that can swell in water to form colloidal solutions of a mucus-like type. Enveloping agents, covering the mucous membranes, prevent irritation of the endings of sensory nerves, thereby protecting the gastrointestinal tract in case of mild disorders. They envelop the mucous membranes, from where they got their name.
Enveloping products by origin are divided into 2 groups:
1) enveloping inorganic type (aluminum oxide hydrate, magnesium trisilicate);
2) enveloping agents of organic origin (mucus from potato, corn, wheat starch, mucus from flax seeds, mucus from rice, marshmallow root tubers, jelly).
Pharmacological effects:
a) anti-inflammatory;
b) antidiarrheal (antidiarrheal);
c) analgesic;
d) partially adsorbent.
Indications for the use of enveloping agents:
In inflammatory processes of the gastrointestinal tract;
When taken together with substances that have an irritating effect (starch mucus);
In clinical toxicology, to reduce the absorption of poison.
Enveloping is not absorbed, so they do not have a resorptive effect. Emollients adjoin the group of enveloping agents. For this purpose, various oils are used (vaseline oil, cocoa butter, glycerin).
ADSORBING AGENTS (ADSORBENTIA) - emollient oils, petroleum jelly, glycerin. Adsorbents are fine powdery inert substances (or ..... cells) with a large adsorption surface, insoluble in water and not irritating to tissues. These funds, adsorbing chemical compounds on their surface, protect the endings of sensitive nerves from their irritating effect. In addition, by covering the skin or mucous membranes with a thin layer, adsorbent agents mechanically protect the endings of sensory nerves.
a) adsorbent;
b) detoxifying;
c) analgesic;
d) anti-inflammatory.
Classical adsorbing agents include TALC, which is a magnesium silicate of the following composition: 4SiO + 3MgO + HO, which, when applied to the skin, adsorbs gland secretions, dries the skin and protects it from mechanical irritation, reduces pathological reflexes.
The adsorbing agents include WHITE CLAY (Bolus alba), ALUMINUM HYDROXIDE (Al(OH)). But the best adsorbent is ACTIVATED CARBON (Carbo activatus), CARBOLEN (Carbonis activati). Effects, indications: adsorbing hemostatic agents for stopping bleeding and gluing tissues during surgical interventions.
Activated charcoal is used for all acute poisoning (alcoloids, salts of heavy metals), often in large doses - 1-2 tablespoons in powder form. For this purpose, we obtain a suspension of activated charcoal in a glass of water, which we introduce either per os to the patient, or through a probe. In tablets, activated charcoal (carbolene - 0.25 and 0.5) is prescribed for flatulence for adsorption of gases (absorb hydrogen sulfide), for dyspepsia, food intoxication.
Adsorbent hemostatic agents for stopping bleeding and gluing tissues during surgical interventions:
Beriplast XC (solution for topical application);
Tachocomb (adsorbent sponge). Thus, astringent, enveloping, absorbent agents have one important common property: they locally, at the point of their application, have an ANTI-INFLAMMATORY EFFECT. In this regard, in the literature they are often called LOCAL ANTIFLOGISTICS (anti-inflammatory agents).
DRUGS AFFECTING EFFERENT INNERVATION (excitation is transmitted from the central nervous system to the tissues; efferens - efferent)
Currently, quite a lot of such funds are known, there are already several hundred.
Recall that efferent innervation includes:
1) autonomic nerves (innervate internal organs, blood vessels, glands)
2) motor nerves of skeletal muscles.
Efferent nerves carry information from the center to the periphery. Let us give brief information on the anatomical and physiological features of the efferent nerves.
The connection between the ends of an axon and a nerve cell, a muscle cell, or a gland cell is called SINAPSE (Sherrington). A person has - chemical synapses, that is, they transmit excitation (action potential) with the help of a chemical, a mediator. The synapse works like a valve (in one direction).
Vegetative innervation, depending on the mediator released in the neuro-effector synapses, is divided into CHOLINERGIC or PARASYMPATIC (mediator - acetylcholine) and ADRENERGIC or SYMPATIC (mediator - norepinephrine) innervation. Autonomic nerves consist of 2 neurons: preganglionic and ganglionic. In cholinergic innervation, the bodies of preganglionic neurons have a craniosacral localization. The cranial nuclei are found in the midbrain and medulla oblongata. The cranial part of the parasympathetic nervous system is represented by a number of cranial nerves: PAIR III (n. oculomotorius), VII pair (n. facialis), IX (n. glossopparyngens), and X - (n. vagus). In this topic, 2 pairs are of particular interest: III and X. In the sacral region (sacral), preganglionic neurons (S II and IY) originate from the lateral horns of the gray matter of the spinal cord.
In adrenergic innervation, the bodies of preganglionic neurons are mainly located in the lateral horns of the thoracolumbar region (sternolumbar) (C, Th-L) of the spinal cord.
The axons of preganglionic neurons terminate in the autonomic ganglia, where they form synaptic contacts with ganglion neurons. Sympathetic ganglia are located outside the organs (sympathetic trunks), and parasympathetic - most often intraorgan. Thus, the length of the preganglionic fibers is different.
The mediator in the sympathetic and parasympathetic ganglia is acetylcholine. Motor neurons that innervate skeletal muscles are cholinergic, that is, neuromuscular transmission is mediated by acetylcholine. They begin in the anterior horns of the spinal cord, as well as the nuclei of individual cranial nerves, and go without interruption to the end plates of the skeletal muscles.
Consequently, efferent nerves are divided into 2 groups: autonomic (autonomous, independent, control the plant functions of the body) and somatic or motor nerves. In turn, autonomic nerves are divided into sympathetic and parasympathetic. Impulses from the autonomic nerves are transmitted by various mediators or transmitters.
If the mediator in neuroeffector synapses is acetylcholine, then we are dealing with cholinergic nerves. These are, first of all, parasympathetic nerves, preganglionic sympathetic nerves and all somatic. Only postganglionic sympathetic nerves release noradrenaline at their endings (adrenergic nerves). In particular, peripheral vessels have practically only sympathetic innervation. The mediator acts on the perceiving apparatus, which are receptors. Synapses where transmission is carried out with the help of acetylcholine belong to cholinergic synapses (ganglia, parasympathetic nerve endings on effector organs, on the neuromuscular ending, that is, on the end plates of skeletal muscles).
CLASSIFICATION OF DRUGS AFFECTING EFFERENT NERVES
The systematics of drugs that affect efferent innervation is based on the direction of their action on synapses with acetylcholine or norepinephrine mediation of nervous excitation. There are 2 main groups of funds:
a) agents that affect cholinergic synapses (cholinergic agents);
b) agents that affect adrenergic synapses (adrenergic agents).
Hosted on Allbest.ru
...Similar Documents
Medicines that affect the regulation of the nervous functions of the body; types of nerves. Superficial, conduction, infiltration anesthesia; local anesthetics: astringents, adsorbents and enveloping agents; irritants and stimulants.
abstract, added 04/07/2012
Substances affecting the peripheral nervous system. The autonomic nervous system and its structure. Resting potential and action potential: stages of occurrence. The effect of drugs on the efferent innervation of cholinergic and adrenergic drugs.
presentation, added 04/02/2011
The structure of the human cerebral cortex, the functions of its individual sections. Classification of disorders of the functions of the central nervous system, features of their clinic. Points of application of neurotropic medicinal substances. Indications for the use of psychotropic drugs.
presentation, added 04/02/2016
Drugs that reduce the sensitivity of the endings of the afferent nerves. The use of drugs that stimulate (irritate) the endings of afferent nerves. The main focus of the action of substances that prevent the excitation of the endings of sensory nerves.
presentation, added 02/23/2016
Sensitive nerve endings. Suprathreshold stimulation of receptors. Drugs that reduce and stimulate the sensitivity of nerve endings. Mechanism of action of local anesthetics. Blockade of nerve impulses along axons.
presentation, added 04/13/2015
Medicinal substances that affect the sensory endings of the afferent nerves and the neurochemical transmission of excitation in the synapses of the autonomic and somatic nervous systems. Competent use of medicinal substances, the nature and mechanism of their action.
tutorial, added 12/20/2011
Analysis of the mechanism of action of antihypertensive (hypotensive) drugs. Classification and general characteristics of drugs. Antiadrenergic agents of central and peripheral action. Means that affect the water-electrolyte balance.
presentation, added 03/30/2015
General characteristics and properties of drugs that affect the digestive organs. Their groups: affecting appetite, secretion of the glands of the stomach, intestinal motility and microflora, liver and pancreas function, emetics and antiemetics.
presentation, added 10/04/2016
Classification of funds that affect the activity of the Central Nervous System of a person, their varieties and nature of action. Means that depress the central nervous system: alcohol and sleeping pills. The effect of ethanol on the liver. The mechanism of action of teturam, advantages and disadvantages.
presentation, added 10/07/2013
Brief historical outline of the development of pharmacology. Rules for prescribing solid dosage forms: tablets, capsules. distribution of drugs in the body. Drugs affecting the nervous system. Classification of adrenergic receptors and their localization.

 Neurotropic drugs I. Drugs that affect the peripheral nervous system: 1) Drugs that affect afferent innervation (conduction of excitation from organs and tissues to the central nervous system): A) drugs that depress afferent innervation: local anesthetics, astringents, adsorbents, enveloping agents. B) means stimulating afferent innervation (substances with a reflex action) 2) means affecting efferent innervation (conducting excitation from the central nervous system to organs and tissues). II. Means affecting the central nervous system.
Neurotropic drugs I. Drugs that affect the peripheral nervous system: 1) Drugs that affect afferent innervation (conduction of excitation from organs and tissues to the central nervous system): A) drugs that depress afferent innervation: local anesthetics, astringents, adsorbents, enveloping agents. B) means stimulating afferent innervation (substances with a reflex action) 2) means affecting efferent innervation (conducting excitation from the central nervous system to organs and tissues). II. Means affecting the central nervous system.



 There are 2 families of receptors for acetylcholine: 1) muscarinic and 2) nicotinic receptors, which differ from each other on the basis of their different affinity for substances that mimic the action of acetylcholine. 1. Muscarinic receptors. Excited by acetylcholine, and muscarine - an alkaloid of poisonous fly agaric. Found in the heart, smooth muscles and endocrine glands. 2. Nicotinic receptors. Cylindrical structure with Na+ channel inside. Binds acetylcholine and nicotine. Nicotine first stimulates, then blocks the receptor. Found in the CNS, adrenal glands, ganglia and neuromuscular junctions. Ganglion nicotinic receptors are distinct from neuromuscular junction receptors.
There are 2 families of receptors for acetylcholine: 1) muscarinic and 2) nicotinic receptors, which differ from each other on the basis of their different affinity for substances that mimic the action of acetylcholine. 1. Muscarinic receptors. Excited by acetylcholine, and muscarine - an alkaloid of poisonous fly agaric. Found in the heart, smooth muscles and endocrine glands. 2. Nicotinic receptors. Cylindrical structure with Na+ channel inside. Binds acetylcholine and nicotine. Nicotine first stimulates, then blocks the receptor. Found in the CNS, adrenal glands, ganglia and neuromuscular junctions. Ganglion nicotinic receptors are distinct from neuromuscular junction receptors.
 Drugs that affect the transmission of excitation in cholinergic synapses Drugs that stimulate: Drugs that block: M-cholinomimetics M-anticholinergics N-cholinomimetics N-anticholinergics: M-, N-cholinomimetics-ganglioblockers Anticholinesterase-muscle relaxants
Drugs that affect the transmission of excitation in cholinergic synapses Drugs that stimulate: Drugs that block: M-cholinomimetics M-anticholinergics N-cholinomimetics N-anticholinergics: M-, N-cholinomimetics-ganglioblockers Anticholinesterase-muscle relaxants
 Substances acting on cholinergic synapses: I. Means stimulating cholinergic synapses 1) Cholinomimetics a) M-cholinomimetics (selectively excite Mcholinergic receptors) Aceclidin, pilocarpine. b) N-cholinomimetics (selectively excite Ncholinergic receptors) Lobelin, cytiton, nicatin (tabex). c) M-, N-cholinomimetics (simultaneously excite M- and N-cholinergic receptors) Acetylcholine, Carbacholin d) Anticholinesterase substances (cholinomimetics of indirect action) Prozerin, physostigmine
Substances acting on cholinergic synapses: I. Means stimulating cholinergic synapses 1) Cholinomimetics a) M-cholinomimetics (selectively excite Mcholinergic receptors) Aceclidin, pilocarpine. b) N-cholinomimetics (selectively excite Ncholinergic receptors) Lobelin, cytiton, nicatin (tabex). c) M-, N-cholinomimetics (simultaneously excite M- and N-cholinergic receptors) Acetylcholine, Carbacholin d) Anticholinesterase substances (cholinomimetics of indirect action) Prozerin, physostigmine
 2) drugs that block cholinergic synapses: A) M-anticholinergics: Atropine, platifillin, belladonna preparations, scopolamine (vegetable origin); Ipratropium bromide, tiotropium bromide, tropicamide (synthetics) B) N-anticholinergics: - ganglioblockers: Benzohexonium, pentamine, hygronium - drugs that block neuromuscular synapses (muscle relaxants): Arduan, Ditilin, Listenon
2) drugs that block cholinergic synapses: A) M-anticholinergics: Atropine, platifillin, belladonna preparations, scopolamine (vegetable origin); Ipratropium bromide, tiotropium bromide, tropicamide (synthetics) B) N-anticholinergics: - ganglioblockers: Benzohexonium, pentamine, hygronium - drugs that block neuromuscular synapses (muscle relaxants): Arduan, Ditilin, Listenon

 M-cholinomimetics of drugs of this group have a direct stimulating effect on M-cholinergic receptors located at the endings of postganglionic parasympathetic nerve fibers. As a result, they reproduce the effects of acetylcholine associated with the excitation of parasympathetic innervation: pupil constriction (miosis), spasm of accommodation (the eye is set to near vision), bronchial constriction, profuse salivation, increased secretion of the bronchial, digestive and sweat glands, increased motility of the gastrointestinal tract , increased tone of the bladder, bradycardia.
M-cholinomimetics of drugs of this group have a direct stimulating effect on M-cholinergic receptors located at the endings of postganglionic parasympathetic nerve fibers. As a result, they reproduce the effects of acetylcholine associated with the excitation of parasympathetic innervation: pupil constriction (miosis), spasm of accommodation (the eye is set to near vision), bronchial constriction, profuse salivation, increased secretion of the bronchial, digestive and sweat glands, increased motility of the gastrointestinal tract , increased tone of the bladder, bradycardia.

 The mechanism of action of M-cholinomimetics Excite muscarinic receptors on the cells of the glands, cardiac and smooth muscles (in the parasympathetic system) and cells of the sweat glands (in the sympathetic system) M 1 - CNS-control of mental and motor functions, autonomic gangia M 2 - heart-bradycardia, weakening of atrial contractions, M 3 -smooth muscles - increased tone; circular and ciliary muscle of the eye contraction, narrowing
The mechanism of action of M-cholinomimetics Excite muscarinic receptors on the cells of the glands, cardiac and smooth muscles (in the parasympathetic system) and cells of the sweat glands (in the sympathetic system) M 1 - CNS-control of mental and motor functions, autonomic gangia M 2 - heart-bradycardia, weakening of atrial contractions, M 3 -smooth muscles - increased tone; circular and ciliary muscle of the eye contraction, narrowing

 Pilocarpine is a plant alkaloid. Synthetically obtained, it is available in the form of pilocarpine hydrochloride. Its effect - lowering intraocular pressure, is used to treat glaucoma (increased intraocular pressure up to 50 -70 mm Hg. Art.). The use of pilocarpine causes constriction of the pupil due to contraction of the circular muscle of the iris, facilitates the outflow of fluid from the anterior chamber of the eye to the back due to the contraction of the ciliary muscle. At the same time, a spasm of accommodation develops (the curvature of the lens increases). Pilocarpine is used only topically, because it is quite toxic. Used for glaucoma, optic nerve atrophy, to improve eye trophism, etc. It has a slight irritating effect. It is part of the combined eye drops Fotil, Pilotim.
Pilocarpine is a plant alkaloid. Synthetically obtained, it is available in the form of pilocarpine hydrochloride. Its effect - lowering intraocular pressure, is used to treat glaucoma (increased intraocular pressure up to 50 -70 mm Hg. Art.). The use of pilocarpine causes constriction of the pupil due to contraction of the circular muscle of the iris, facilitates the outflow of fluid from the anterior chamber of the eye to the back due to the contraction of the ciliary muscle. At the same time, a spasm of accommodation develops (the curvature of the lens increases). Pilocarpine is used only topically, because it is quite toxic. Used for glaucoma, optic nerve atrophy, to improve eye trophism, etc. It has a slight irritating effect. It is part of the combined eye drops Fotil, Pilotim.
 Release form 1%, 2% eye drops of 5 and 10 ml, tube drops of 1.5 ml, 1 and 5% eye ointment, eye films, soda 0.0027 g of pilocarpine. Decrease in IOP after 10-30 minutes, the patient's condition is relieved for 4-8 hours
Release form 1%, 2% eye drops of 5 and 10 ml, tube drops of 1.5 ml, 1 and 5% eye ointment, eye films, soda 0.0027 g of pilocarpine. Decrease in IOP after 10-30 minutes, the patient's condition is relieved for 4-8 hours

 Aceclidine causes an increase in the functions of organs innervated by cholinergic nerves (increases tone and enhances peristalsis of the gastrointestinal tract, bladder, uterus. Used in ophthalmic practice (for glaucoma), parenterally for atony of the intestine and bladder (difficulty emptying).
Aceclidine causes an increase in the functions of organs innervated by cholinergic nerves (increases tone and enhances peristalsis of the gastrointestinal tract, bladder, uterus. Used in ophthalmic practice (for glaucoma), parenterally for atony of the intestine and bladder (difficulty emptying).
 N-cholinomimetics Nicotine is an alkaloid from tobacco leaves. Effects of small nicotine doses stimulating effect: increasing pulmonary ventilation, increased blood pressure, activation of Motoric K-ka, strengthening the secretion of bronchial glands, psychostimulating effect, it is possible to nauseate and vomiting the effects of large doses of nicotine inhibitory effect: respiratory depression, reduced blood pressure, inhibition of your kisnchnik, decreases SECRETORY ACTIVITY OF THE GLANDS, DOSPITALITY DEVELOPES, ALTHOUGH CONSUMS CAN DEVELOP IN THE BEGINNING.
N-cholinomimetics Nicotine is an alkaloid from tobacco leaves. Effects of small nicotine doses stimulating effect: increasing pulmonary ventilation, increased blood pressure, activation of Motoric K-ka, strengthening the secretion of bronchial glands, psychostimulating effect, it is possible to nauseate and vomiting the effects of large doses of nicotine inhibitory effect: respiratory depression, reduced blood pressure, inhibition of your kisnchnik, decreases SECRETORY ACTIVITY OF THE GLANDS, DOSPITALITY DEVELOPES, ALTHOUGH CONSUMS CAN DEVELOP IN THE BEGINNING.
 N-cholinomimetics (cytiton, lobelin) excite N-cholinergic receptors of carotid sinus glomeruli, which leads to reflex stimulation of the respiratory and vasomotor centers. There is an increase and deepening of breathing. Simultaneous excitation of synaptic nodes and adrenal glands leads to an increase in the release of adrenaline and an increase in blood pressure. Cytiton and Lobelina hydrochloride are reflex action stimulants of respiration and can be used for reflex respiratory arrest (carbon monoxide poisoning, drowning, suffocation, electrical injuries, etc.), and neonatal asphyxia. More widely, these substances are used to treat tobacco smoking. As part of tablets, Tabex (cytisine) is used to facilitate smoking cessation. For this purpose, small doses of nicotine are also used (Nicorette chewing gum, Nicotinell patch). These medicines reduce physical dependence on nicotine. Tobacco alkaloid - nicotine is also an N-cholinomimetic, but is not used as a drug. Penetrates the body when smoking tobacco and has a variety of effects. Nicotine affects both peripheral and central Ncholinergic receptors, and has a two-phase effect: the first stage - excitation - is replaced by a depressing effect. The constant effect of nicotine is its vasoconstrictive effect, due to the fact that nicotine stimulates the H-cholinergic receptors of the sympathetic ganglia, chromaffin cells of the adrenal glands and the carotid sinus zone, stimulates the release of adrenaline and reflexively excites the vasomotor center. In this regard, nicotine increases blood pressure and contributes to the development of hypertension. Severe vascular disease of the lower extremities - obliterating endarteritis - occurs almost exclusively in smokers. Nicotine narrows the blood vessels of the heart and contributes to the development of angina pectoris, myocardial infarction, tachycardia. Serious changes are observed from the side of the central nervous system. Exhibits nicotine and carcinogenic effects.
N-cholinomimetics (cytiton, lobelin) excite N-cholinergic receptors of carotid sinus glomeruli, which leads to reflex stimulation of the respiratory and vasomotor centers. There is an increase and deepening of breathing. Simultaneous excitation of synaptic nodes and adrenal glands leads to an increase in the release of adrenaline and an increase in blood pressure. Cytiton and Lobelina hydrochloride are reflex action stimulants of respiration and can be used for reflex respiratory arrest (carbon monoxide poisoning, drowning, suffocation, electrical injuries, etc.), and neonatal asphyxia. More widely, these substances are used to treat tobacco smoking. As part of tablets, Tabex (cytisine) is used to facilitate smoking cessation. For this purpose, small doses of nicotine are also used (Nicorette chewing gum, Nicotinell patch). These medicines reduce physical dependence on nicotine. Tobacco alkaloid - nicotine is also an N-cholinomimetic, but is not used as a drug. Penetrates the body when smoking tobacco and has a variety of effects. Nicotine affects both peripheral and central Ncholinergic receptors, and has a two-phase effect: the first stage - excitation - is replaced by a depressing effect. The constant effect of nicotine is its vasoconstrictive effect, due to the fact that nicotine stimulates the H-cholinergic receptors of the sympathetic ganglia, chromaffin cells of the adrenal glands and the carotid sinus zone, stimulates the release of adrenaline and reflexively excites the vasomotor center. In this regard, nicotine increases blood pressure and contributes to the development of hypertension. Severe vascular disease of the lower extremities - obliterating endarteritis - occurs almost exclusively in smokers. Nicotine narrows the blood vessels of the heart and contributes to the development of angina pectoris, myocardial infarction, tachycardia. Serious changes are observed from the side of the central nervous system. Exhibits nicotine and carcinogenic effects.
 N-CHOLINOMIMETICS Cytisine (thermopsis alkaloid) tablets "Tabex" and Lobelin (lobelia alkaloid) - tablets "Lobesil" (to facilitate smoking cessation) are similar in action to nicotine, but differ in less activity and toxicity.
N-CHOLINOMIMETICS Cytisine (thermopsis alkaloid) tablets "Tabex" and Lobelin (lobelia alkaloid) - tablets "Lobesil" (to facilitate smoking cessation) are similar in action to nicotine, but differ in less activity and toxicity.


 Indications for the appointment of M-Ncholinomimetics Acetylcholine (a mediator that transmits excitation in all cholinergic synapses). - as a drug, they are almost never used, because its short-term effect is several minutes. Widely used in experimental work. Carbachol (Carbacholin) acts longer. - with atony of the intestines and bladder, sometimes with glaucoma.
Indications for the appointment of M-Ncholinomimetics Acetylcholine (a mediator that transmits excitation in all cholinergic synapses). - as a drug, they are almost never used, because its short-term effect is several minutes. Widely used in experimental work. Carbachol (Carbacholin) acts longer. - with atony of the intestines and bladder, sometimes with glaucoma.




 In terms of its effect on M-cholinergic receptors, it is close to atropine, but inferior to it in activity. It has a calming effect on the central nervous system. It is used for spasms of smooth muscles of internal organs, gastric ulcer, bronchial asthma, and also as a drug that dilates the pupil.
In terms of its effect on M-cholinergic receptors, it is close to atropine, but inferior to it in activity. It has a calming effect on the central nervous system. It is used for spasms of smooth muscles of internal organs, gastric ulcer, bronchial asthma, and also as a drug that dilates the pupil.

 Ganglioblockers - drugs that block N-cholinergic receptors of the ganglia of the sympathetic and parasympathetic systems, the adrenal medulla, carotid glomeruli. Used for hypertensive crisis, combined therapy of the lungs and brain, heart.
Ganglioblockers - drugs that block N-cholinergic receptors of the ganglia of the sympathetic and parasympathetic systems, the adrenal medulla, carotid glomeruli. Used for hypertensive crisis, combined therapy of the lungs and brain, heart.
 Classification according to the duration of action Hexamethonium benzosulfonate (benz oxonium) and azamethonium bromide (pentamine) -4 -7 long-term action. Trepirium iodide (hygronium) - 1015 min
Classification according to the duration of action Hexamethonium benzosulfonate (benz oxonium) and azamethonium bromide (pentamine) -4 -7 long-term action. Trepirium iodide (hygronium) - 1015 min

 storage conditions Pilocarpini hydrochoridum (A) Tabex Neostigminum (Proserinum) (A) Galantaminihydrobromidum (Nivalinum) (A) Distigminibromidum (Ubretidum) (A) Release forms Methods of application Ch. drops 2% solution - 2 ml m 1%, 2%, 10% solution - 5 ml, 10 Into the cavity of the conjunctiva 11-2 drops 2-3 times a day ml Lay behind the eyelid 1 time per day Ch. films Tab. 0, 0015 Take according to the scheme 1 tab. 2-3 times a day Tab. 0.015 Under the skin 1 ml Amp. 0.05% - 1 ml Into the cavity of the conjunctiva, 1-2 drops 2-3 times in Ch. drops 0.5% - 5 ml per day Tab. 0.02; 0.005 1 tab. 2-3 times a day after meals Amp. 0.25%; 0.5%; 1% solution - 1 ml. Under the skin, 1 ml Tab. 0.005 1 tab. 1 time per day Amp. 0.05%; 0.1% solution - 1 ml. Under the skin, 1 ml Chap. drops 1% solution - 5 ml In the cavity of the conjunctiva, 1-2 drops of T-ra Belladonnae (B) "Becarbonum" Amp. 0.1% solution - 1 ml Flac. 10 ml Official tab. Under the skin 0, 25-1 ml 5-10 drops per reception 1 tab. 2-3 times a day "Anusolum" Official. suppositories 1 suppository in the rectum at night Atropini sulfas (A) Amp. 0.05% solution - 1 ml Official. tab. In the cavity of the conjunctiva, 1-2 drops 2-3 times a day Under the skin 0.5-1 ml 1-2 tablets. before flight Metacinium iodidum (Methacinum) (A) Tab. 0.002 Amp. 0, 1% solution - 1 ml According to 1-2 tab. 2-3 times a day Under the skin (into a muscle, into a vein) 1 ml of Pirenzepinum (Gastrilum, Gastrozepinum) Tab. 0.025; 0.05 Amp. 0.5% solution - 2 ml 2 tablets. 2 times a day before meals Into the muscle (into a vein), 2 ml of Ipratropium bromidum (Atroventum) Tab. 0.01 Aerosol 300 doses 1 tab. 2-3 times a day before meals Inhale 2-3 times a day Hexamethonium (Benzohexonium) (B) Tab. 0, 1; 0.025 Amp. . 2, 5% solution - 1 ml 1-2 tablets. 3-4 times a day Under the skin (into the muscle) 1 ml 1-2 times a day Trepirium iodidum (Hygronium) (B) Amp. 0, 1 dry in-va Into a vein drip with 0.9% solution of sodium chloride Tubocurarini chloridum (A) Diplacinum (A) Suxamethonium Amp. 1% solution - 1.5 ml Amp. 2% solution - 5 ml In a vein, 0.5 ml per 1 kg of body weight In a vein, 0.25 ml per 1 kg of body weight Scopolamini hydrobromidun (A) "Aeronum" (B) Flac. 0.25% solution - 5 ml
storage conditions Pilocarpini hydrochoridum (A) Tabex Neostigminum (Proserinum) (A) Galantaminihydrobromidum (Nivalinum) (A) Distigminibromidum (Ubretidum) (A) Release forms Methods of application Ch. drops 2% solution - 2 ml m 1%, 2%, 10% solution - 5 ml, 10 Into the cavity of the conjunctiva 11-2 drops 2-3 times a day ml Lay behind the eyelid 1 time per day Ch. films Tab. 0, 0015 Take according to the scheme 1 tab. 2-3 times a day Tab. 0.015 Under the skin 1 ml Amp. 0.05% - 1 ml Into the cavity of the conjunctiva, 1-2 drops 2-3 times in Ch. drops 0.5% - 5 ml per day Tab. 0.02; 0.005 1 tab. 2-3 times a day after meals Amp. 0.25%; 0.5%; 1% solution - 1 ml. Under the skin, 1 ml Tab. 0.005 1 tab. 1 time per day Amp. 0.05%; 0.1% solution - 1 ml. Under the skin, 1 ml Chap. drops 1% solution - 5 ml In the cavity of the conjunctiva, 1-2 drops of T-ra Belladonnae (B) "Becarbonum" Amp. 0.1% solution - 1 ml Flac. 10 ml Official tab. Under the skin 0, 25-1 ml 5-10 drops per reception 1 tab. 2-3 times a day "Anusolum" Official. suppositories 1 suppository in the rectum at night Atropini sulfas (A) Amp. 0.05% solution - 1 ml Official. tab. In the cavity of the conjunctiva, 1-2 drops 2-3 times a day Under the skin 0.5-1 ml 1-2 tablets. before flight Metacinium iodidum (Methacinum) (A) Tab. 0.002 Amp. 0, 1% solution - 1 ml According to 1-2 tab. 2-3 times a day Under the skin (into a muscle, into a vein) 1 ml of Pirenzepinum (Gastrilum, Gastrozepinum) Tab. 0.025; 0.05 Amp. 0.5% solution - 2 ml 2 tablets. 2 times a day before meals Into the muscle (into a vein), 2 ml of Ipratropium bromidum (Atroventum) Tab. 0.01 Aerosol 300 doses 1 tab. 2-3 times a day before meals Inhale 2-3 times a day Hexamethonium (Benzohexonium) (B) Tab. 0, 1; 0.025 Amp. . 2, 5% solution - 1 ml 1-2 tablets. 3-4 times a day Under the skin (into the muscle) 1 ml 1-2 times a day Trepirium iodidum (Hygronium) (B) Amp. 0, 1 dry in-va Into a vein drip with 0.9% solution of sodium chloride Tubocurarini chloridum (A) Diplacinum (A) Suxamethonium Amp. 1% solution - 1.5 ml Amp. 2% solution - 5 ml In a vein, 0.5 ml per 1 kg of body weight In a vein, 0.25 ml per 1 kg of body weight Scopolamini hydrobromidun (A) "Aeronum" (B) Flac. 0.25% solution - 5 ml

 Localization of cholinergic receptors and adrenoreceptors Cholinergic receptors M 1 M 2 M 3 Ng Nm CNS, autonomic ganglia Heart Circular and ciliary muscles of the eye, smooth muscles of internal organs, glands. Ganglia, adrenal medulla, carotid glomeruli Skeletal muscles Adrenoreceptors α 1 α 2 β 1 β 2 β 3 Radial muscle of the eye, vessels of smooth muscles of organs, skin, kidneys, veins, arterioles, liver, CNS myometrium, peripheral vessels, Platelets Heart, juxtaglomerular apparatus of the kidneys, ciliary body of the eyes, platelets Smooth muscles of the bronchi, liver, myometrium, coronary vessels. fat cells
Localization of cholinergic receptors and adrenoreceptors Cholinergic receptors M 1 M 2 M 3 Ng Nm CNS, autonomic ganglia Heart Circular and ciliary muscles of the eye, smooth muscles of internal organs, glands. Ganglia, adrenal medulla, carotid glomeruli Skeletal muscles Adrenoreceptors α 1 α 2 β 1 β 2 β 3 Radial muscle of the eye, vessels of smooth muscles of organs, skin, kidneys, veins, arterioles, liver, CNS myometrium, peripheral vessels, Platelets Heart, juxtaglomerular apparatus of the kidneys, ciliary body of the eyes, platelets Smooth muscles of the bronchi, liver, myometrium, coronary vessels. fat cells


 EFFECTS OF -ADRENOBLOCKERS Decrease in peripheral resistance, venous return, cardiac output, decrease in blood pressure, hypotension. reflex tachycardia. Miosis is a blockade of α-receptors in the radial muscle of the eye. Swelling of the nasal mucosa - blockade of α-receptors of the mucosal vessels. Increased intestinal peristalsis diarrhea. Decrease in renal blood flow; decrease in filtration rate; retention of sodium and water ions in the body. Decreased potency in men.
EFFECTS OF -ADRENOBLOCKERS Decrease in peripheral resistance, venous return, cardiac output, decrease in blood pressure, hypotension. reflex tachycardia. Miosis is a blockade of α-receptors in the radial muscle of the eye. Swelling of the nasal mucosa - blockade of α-receptors of the mucosal vessels. Increased intestinal peristalsis diarrhea. Decrease in renal blood flow; decrease in filtration rate; retention of sodium and water ions in the body. Decreased potency in men.
 -ADRENOBLOCKERS indications for use Non-selective 1-, 2-blockers: Relief of hypertensive crises (phentolamine, tropafen). Long-term treatment of pheochromocytoma (phenoxybenzamine). Violation of the peripheral circulation. Vestibular disorders (pyrroxane). Relief of acute migraine attacks - (ergot alkaloids). Cerebral vascular diseases (vasobral, nicergldine). Selective 1-, 2-blockers: Arterial hypertension. Prostate adenoma (tamsulosin). Violation of the peripheral circulation.
-ADRENOBLOCKERS indications for use Non-selective 1-, 2-blockers: Relief of hypertensive crises (phentolamine, tropafen). Long-term treatment of pheochromocytoma (phenoxybenzamine). Violation of the peripheral circulation. Vestibular disorders (pyrroxane). Relief of acute migraine attacks - (ergot alkaloids). Cerebral vascular diseases (vasobral, nicergldine). Selective 1-, 2-blockers: Arterial hypertension. Prostate adenoma (tamsulosin). Violation of the peripheral circulation.
 Classification of -blockers Non-selective (1+ 2): A. without internal sympathomimetic activity - propranolol (anaprilin), sotalol, timolol; B. with internal sympathomimetic activity - pindolol, oxprenolol, alprenolol; Cardioselective (1): . A. without internal sympathomimetic activity - atenolol, metoprolol, bisoprolol, nebivolol, betaxolol, talinolol; B. with internal sympathomimetic activity - acebutolol, practolol; Selective (2): – butoxamine (butoxamine)
Classification of -blockers Non-selective (1+ 2): A. without internal sympathomimetic activity - propranolol (anaprilin), sotalol, timolol; B. with internal sympathomimetic activity - pindolol, oxprenolol, alprenolol; Cardioselective (1): . A. without internal sympathomimetic activity - atenolol, metoprolol, bisoprolol, nebivolol, betaxolol, talinolol; B. with internal sympathomimetic activity - acebutolol, practolol; Selective (2): – butoxamine (butoxamine)
 Pharmacological effects of -adrenoblockers Blockade of 1 receptors of the heart - weakening of the strength of heart contractions - decrease in automatism of the atrioventricular node - inhibition of atrioventricular conduction - decrease in automatism of the atrioventricular node and Purkinje fibers Decrease in cardiac output (minute volume), heart work and myocardial oxygen demand - decrease in renin secretion
Pharmacological effects of -adrenoblockers Blockade of 1 receptors of the heart - weakening of the strength of heart contractions - decrease in automatism of the atrioventricular node - inhibition of atrioventricular conduction - decrease in automatism of the atrioventricular node and Purkinje fibers Decrease in cardiac output (minute volume), heart work and myocardial oxygen demand - decrease in renin secretion
 Pharmacological effects of -adrenergic blockers Blockade of 2 receptors narrowing of blood vessels Increased bronchial tone Increased contractile activity of the myometrium Decreased hyperglycemic action of adrenaline 2 Pupil size and accommodation do not change. Used in the treatment of glaucoma. CNS - sedation, drowsiness, lethargy, depressive states. Sexual function - decreased libido, decreased potency.
Pharmacological effects of -adrenergic blockers Blockade of 2 receptors narrowing of blood vessels Increased bronchial tone Increased contractile activity of the myometrium Decreased hyperglycemic action of adrenaline 2 Pupil size and accommodation do not change. Used in the treatment of glaucoma. CNS - sedation, drowsiness, lethargy, depressive states. Sexual function - decreased libido, decreased potency.
 Indications Arterial hypertension! Ischemic heart disease (treatment and prevention)! Tachyarrhythmias! Glaucoma (timolol, proxodolol) Increased labor activity, stopping uterine bleeding Prevention of some forms of tremor
Indications Arterial hypertension! Ischemic heart disease (treatment and prevention)! Tachyarrhythmias! Glaucoma (timolol, proxodolol) Increased labor activity, stopping uterine bleeding Prevention of some forms of tremor