The well-being of a nation is determined by the level of its health, one of the components of which is nutrition. It is a necessary condition for normal life and working capacity, resistance to diseases, an active life position both in adulthood and in childhood.
However, the negative trends of recent decades have affected the state of health of citizens of the entire state, which resulted in a significant reduction in life expectancy: according to this indicator, Russia lags behind developed countries by 20–25 years. Often people, especially males, die immediately after they go on a well-deserved rest.
Of course, an unbalanced diet plays a significant role in such sad statistics, when the diet is overloaded with fats and carbohydrates, but there is a constant lack of proteins, vitamins, microelements, including fluorine, iron, potassium, iodine, calcium. The reason for such distortions in nutrition can be hidden both in a significant decrease and loss of the purchasing power of Russian citizens, and in a lack of knowledge in matters of proper healthy nutrition. When filling the food basket, the citizens of our country are often guided solely by their own taste preferences, without thinking about the importance of providing the body with micronutrients that are not synthesized by the body itself, but come there exclusively from the outside. In this case, the main task is to ensure a regular and sufficient intake of micronutrients for the body in accordance with the physiological norm.
The importance of this moment was highlighted at the international conference of the World Health Organization, which was held in the early 90s in the capital of Italy. It was noted that the lack of micronutrients in the daily diet of the population is relevant even for developed countries, and in countries with a low standard of living, it has become a global threat. Measures not taken in time to effectively correct micronutrient deficiencies can lead to the formation of a number of common chronic diseases, a low level of health for entire generations, which will directly affect the quality of life of the population of our country.
Iron- the most important trace element, the deficiency of which can be expressed in various forms:
- prelatent,
- latent,
- Iron-deficiency anemia.
The prevalence of this disease among some categories of the population of the Russian Federation ranges from 20 to 80%, and so far the situation remains quite serious. This is evidenced by the decision of the Chief State Sanitary Doctor of the Russian Federation Onishchenko G.G. dated 05.05.2003 No. 91 "On measures to prevent diseases caused by iron deficiency in the structure of nutrition of the population." The document presents data according to which the incidence of anemia has doubled over the past decade and the reason for this is poor nutrition in vitamins and microelements. Infants of the first year of life, children under 3 years of age, as well as women with different stages of pregnancy and nursing mothers are at particular risk.
Iron deficiency in a child's body has particularly devastating consequences: almost all organs and systems of the child function in a slow mode, the immune system suffers, and there is an increasing lag in the mental and physical development of children.
This problem is being studied at the international level, comparative analyzes of the nutrition of the population of different countries are being carried out, including taking into account food habits and the objective prevailing conditions for food production. Studies have shown that severe forms of iron deficiency anemia (IDA) are directly related to the lack of iron in the daily diet of various populations, and they are also a consequence of the lack of prevention, which involves taking iron supplements.
 As it turned out, the deficiency of this microelement in any form causes a negative impact on health in general, including malfunctions of the central nervous system, cardiovascular and digestive systems, slows down the processes of hematopoiesis and tissue regeneration, causing immunity disorders, infectious diseases, slowing down intellectual and physical development of children, disability in adults.
As it turned out, the deficiency of this microelement in any form causes a negative impact on health in general, including malfunctions of the central nervous system, cardiovascular and digestive systems, slows down the processes of hematopoiesis and tissue regeneration, causing immunity disorders, infectious diseases, slowing down intellectual and physical development of children, disability in adults.
In this regard, the World Health Organization has developed the Iron Fortification Program, which is recommended for implementation in most countries of the world. Based on this document, their own nationwide programs for the prevention of iron deficiency were adopted. There is such a program in the Russian Federation, according to which the state policy regarding the healthy nutrition of the population involves the production of iron-enriched products, as well as the production of biologically active food supplements (BAA) with anti-anemic action.
Thus, the relevance of clinical nutrition research is dictated by the need to take urgent measures to prevent and eliminate iron deficiency in the population of our country, especially children and adolescents.
PREVENTION AND TREATMENT OF IRON DEFICIENCY IN HUMANS
According to the WHO, iron deficiency- a truly massive disease. Of the 7 billion people who make up the world's population, about 2 billion suffer from some degree of iron deficiency. Currently, in medical circles, this disease has become known as sideropenia. Sideropenia has become especially widespread in third world countries, where the low standard of living of the population does not allow diversifying the diet sufficiently. However, in developed countries, the picture is not so favorable, the reasons for this phenomenon are:
- insufficient iron content in the diet,
- violation of absorption processes in the intestine,
- depletion of microelement reserves due to blood loss,
- increased need for iron in children and adolescents during intensive growth,
- pregnancy,
- lactation period.
Of no small importance is the low content of iron in the soils of certain territories, such as the Vladimir, Yaroslavl, Kostroma, Ivanovo and Vologda regions of the Central Federal District, as well as in the Northern Urals, in the highlands of Central Asia.
Approximately 60 mg of a trace element per kilogram of weight of a healthy person, so the total amount of iron approaches 5 g. Most of it is found in blood hemoglobin, but it also accumulates in the spleen, liver, muscle tissue myoglobin, brain and bone marrow, groups. More than 7 dozen enzymes, including proteins lactoferrin, transferrin, are the main depots of iron in the body.
In the muscles of an adult male, myoglobin contains 100 mg of iron, in women - 30-50 mg less, in newborns after a full-term pregnancy - 400 mg, and in premature babies - only 100 mg.
If the microelement accumulates in the body in insufficient quantities, then they talk about WDN - the iron deficiency state of the body. Its variety is the clinical and hematological syndrome with the abbreviation IDA, when iron deficiency provokes a failure in the synthesis of hemoglobin in the body.
According to the WHO, three quarters of anemia of various origins were caused by anemic IDA syndrome, which in absolute terms amounted to more than 200 million people. Women of the fertile period of life, expectant mothers at various stages of pregnancy, as well as children of preschool age, fall into a special risk group. In the United States, 25% of children under the age of two are prone to iron deficiency anemia, and in Russia this figure is already 50%. Children of senior preschool and primary school age also become ill with anemia quite often, their share is 20%.
Due to intense blood loss, 90% of women in these groups have some degree of iron deficiency, 30% of the remaining Russian women also have a latent iron deficiency. These indicators are higher in such regions of our country as the North Caucasus, Eastern Siberia, and the Arctic.
Thus, they can develop iron deficiency anemia at any time.
As a rule, the initial symptoms of sideropenia do not alert potential patients. Systolic murmur, tachycardia, dizziness, general weakness, shortness of breath, pallor of the skin are attributed to fatigue or stress. In fact, all these symptoms are caused by a lack of oxygen in the tissues and organs, which causes IDA. Without proper treatment, the body continues to degrade and disturbances appear in the immune, respiratory systems, central nervous system, gastrointestinal tract, and cardiovascular system. Sideropenia becomes the forerunner of many serious diseases, the causes of which could be eliminated by increasing iron intake. Such unpleasant signs of sideropenia as brittle nails, hair loss, changes in taste and smell sensations are also familiar to most people.
Thus, almost no disease in children and adults can be cured completely without eliminating IDA, which can have two pathogenetic expressions:
1) insufficient activity of tissue respiration enzymes;
2) incomplete provision of oxygen to the body.
Diagnosis of WDN is based on the establishment of laboratory signs of anemia proper and iron deficiency in the body (Table 1).
Table 1.
Indicators of the exchange of iron, erythrocytes and hemoglobin in healthy people, patients with IDA and in patients with IHD.

The World Health Organization, the American Committee on Nutrition and Nutritional Supplements attach critical importance to iron trace elements in the treatment of anemia. It is impossible to correct the balance of iron content in the body by changing the diet or using herbal medicine. They can act as maintenance therapy after the treatment itself, but they cannot fully replace it. The Russian scientist A. Alperin created the most comprehensive classification of IDA, where this pathology is divided by severity, stages and form. According to his classification, severe anemia implies a hemoglobin level in the body of less than 70 g / l, the average corresponds to 70-90 g / l, and mild anemia is estimated at Hb from 90 to 110 g / l.
IRON DEFICIENCY IN CHILDREN AND ADOLESCENTS.
 As the medical statistics of the Office for the Protection of Motherhood and Childhood of the Ministry of Health of the Russian Federation show, in our country, various degrees of WDN are diagnosed in 30% of children of preschool and primary school age, as well as in almost all women with different stages of pregnancy. The consequence of this are frequent acute respiratory viral infections, infections of the digestive system, and deaths. For example, when suffering from salmonellosis, children with high hemoglobin levels tolerate this disease more easily than small patients with IDA.
As the medical statistics of the Office for the Protection of Motherhood and Childhood of the Ministry of Health of the Russian Federation show, in our country, various degrees of WDN are diagnosed in 30% of children of preschool and primary school age, as well as in almost all women with different stages of pregnancy. The consequence of this are frequent acute respiratory viral infections, infections of the digestive system, and deaths. For example, when suffering from salmonellosis, children with high hemoglobin levels tolerate this disease more easily than small patients with IDA.
The lack of a microelement also damages the brain activity of the child's developing organism. Apathy, inhibited reactions, a dull mood, capriciousness - all these deviations in behavior indicate iron deficiency anemia in a growing organism. If a child is not interested in learning, he complains of a deterioration in memory and concentration, then this also applies to the symptoms of IDA.
A control group of schoolchildren who were diagnosed with mild anemia showed reduced mental development: their IQ was 25 points lower, and problem solving took 4.08 seconds compared to 1.81 seconds for children without anemia.
Table 2.
Symptoms of clinical polymorphism depending on age.

Prevention of iron deficiency anemia in children during the first months of life includes a balanced diet for women during pregnancy and lactation with the inclusion of a sufficient amount of meat products, fruits and vegetables rich in vitamin C, as well as specialized products containing minerals and vitamins. When the hemoglobin content is below 100 g / l, it is advisable to prescribe oral ferropreparations or iron-fortified multivitamins to a woman.
The natural prevention of IDA in children during the first months of life is exclusively breastfeeding up to 4-6 months of life. It is known that the concentration of iron in human milk is only 0.2-0.4 mg / l, but this is enough to meet the needs of a growing child's body in iron due to its high bioavailability (50%).
With artificial feeding for children of the first half of life, mixtures with an iron content of 0.4 to 0.8 mg / 100 ml are used, which is quite sufficient, since the “maternal” iron reserves are not yet depleted. The content of iron in the "subsequent" adapted milk mixtures (for children of the second half of life) increases to 0.9-1.3 mg / 100 ml.
By 4-6 months of age, antenatal iron stores are depleted in the child's body and its metabolism becomes absolutely dependent on the amount of micronutrients supplied with food in the form of complementary foods. When choosing products to compensate for iron deficiency, it is necessary to take into account not only the total amount of iron in the products, but also the qualitative form of its compounds.
It is advisable to include industrial products enriched with iron in the diet (fruit juices, fruit and vegetable purees, instant cereals), which increases the amount of iron that enters the child's body with food.
Despite the high content of iron in some products of plant origin, they are not able to provide the high ferro-needs of a growing child's body. The substances present in plant products (tannins, phytins, phosphates) form insoluble compounds with Fe (III) and are excreted with feces. There is also evidence of an adverse effect on the absorption of iron by dietary fiber, which is rich in cereals, fresh vegetables, and fruits. In the intestine, dietary fiber is practically not digested, iron is fixed on their surface and excreted from the body. On the contrary, ascorbic and other organic acids, as well as animal protein containing heme iron, increase the bioavailability of iron.
It is important that meat and fish products increase the absorption of iron from fruits and vegetables when they are used simultaneously. Given the above, as well as the high content of readily available iron in meat, it is recommended to introduce meat complementary foods no later than 6 months.
Whole cow's milk is not used in the nutrition of children under 1 year old. The concentration of iron in cow's milk is only 0.3 mg/l, and its bioavailability is about 10%. Numerous studies have shown that the use of non-adapted products (cow's milk and kefir) in the diet of young children leads to the occurrence of microdiapedetic gastrointestinal bleeding, which is a risk factor for the development of WDN.
Materials for this chapter are also provided by: PhD Rybakova E.P. (Moscow), Ph.D. Bushueva T.V. (Moscow), Ph.D. Stepanova T.N. (Moscow), Ph.D. Kazyukova T.V. (Moscow)
Pharmaceutical Care:
iron deficiency anemia treatment
I. A. Zupanets, N. V. Bezdetko, National Pharmaceutical University
Blood is the vital medium of the body. It performs numerous and varied functions: respiration, nutrition, excretion, thermoregulation, maintaining water and electrolyte balance. The protective and regulatory functions of blood are well known due to the presence of phagocytes, antibodies, biologically active substances, and hormones in it.
The most common blood disorder is iron deficiency anemia. According to WHO, more than half of the population of various countries suffer from iron deficiency anemia. It covers all age groups of the population, but is most common in children, adolescents and pregnant women. In many countries, the issue of preventing and treating anemia is becoming a social issue. The presence of an iron deficiency state reduces the quality of life of patients, disrupts their ability to work, and causes functional disorders in many organs and systems. For the prevention and elimination of iron deficiency conditions, a whole group of iron-containing preparations is successfully used, the range of which is continuously replenished and updated. The recommendations of the pharmacist on the choice of the optimal drug, the conditions for its rational use will help to significantly improve the well-being and quality of life of patients with iron deficiency, as well as contribute to the timely prevention of the development of iron deficiency in "risk groups".
The role of iron and its metabolism in the human body
The body of an adult contains 2-5 g of iron, in a newborn - 300-400 mg. However, despite its low content, iron is a unique trace element in its significance, which is present in various molecular systems: from complexes in solution to macromolecular proteins in cell membranes and organelles. In particular, iron is an important constituent of hemoglobin, myoglobin and iron-containing enzymes.
First of all, the role of iron is determined by its active participation in tissue respiration, which is an indispensable condition for the existence of any living cell. Iron is a component of chromoprotein proteins that provide electron transfer in biological oxidation chains. These chromoprotein proteins include cytochrome oxidase, an enzyme of the respiratory chain that directly interacts with oxygen, as well as cytochrome components localized in the membranes of mitochondria and the endoplasmic reticulum. As part of heme, iron is one of the components of hemoglobin, a universal molecule that provides the binding, transport and transfer of oxygen to cells of various organs and tissues, as well as myoglobin, a heme-containing protein in muscle tissue. In addition, iron is involved in a number of other biologically important processes occurring at the cellular and molecular level, in particular, in the processes of cell division, the biosynthesis of DNA, collagen, and the functional activity of various parts of the immune system.
About 60-65% of the total iron in the body is found in hemoglobin, 2.5-4% in the bone marrow, 4-10% in myoglobin, 0.1-0.5% in iron-containing enzymes and 24-26 % in the form of iron depot in the form of ferritin and hemosiderin.
Iron absorption is a complex process. Iron absorption occurs mainly in the initial part of the small intestine. It is important to note that the greater the iron deficiency in the body, the larger the zone of its absorption in the intestine, with anemia, all parts of the small intestine are involved in the absorption process. From the intestinal mucosa to the blood, iron is transported using active transport mechanisms of cells. This process is carried out only with the normal structure of mucosal cells, which is supported by folic acid. Transport through the cells of the intestinal mucosa is carried out both by simple diffusion and with the participation of a special carrier protein. This protein is most intensively synthesized in anemia, which ensures better absorption of iron. The protein transfers iron only once, the next iron molecules carry new carrier protein molecules. It takes 4-6 hours for their synthesis, therefore, more frequent intake of iron preparations does not increase its absorption, but increases the amount of unabsorbed iron in the intestine and the risk of side effects.
There are two types of iron: heme and non-heme. Heme iron is part of hemoglobin. It is contained only in a small part of the diet (meat products), is well absorbed (by 20-30%), its absorption is practically not affected by other food components. Non-heme iron is in free ionic form - ferrous (Fe II) or ferric (Fe III). Most dietary iron is non-heme iron (found mainly in vegetables). The degree of its assimilation is lower than that of heme, and depends on a number of factors. From food, only divalent non-heme iron is absorbed. To “turn” ferric iron into ferrous, a reducing agent is needed, the role of which in most cases is played by ascorbic acid (vitamin C).
Iron is absorbed in both heme and non-heme form. A balanced daily diet contains about 5-10 mg of iron (heme and non-heme), but no more than 1-2 mg is absorbed.
In the process of absorption in the cells of the intestinal mucosa, ferrous iron Fe2 + turns into oxide Fe3 + and binds to a special carrier protein - transferrin, which transports iron to hematopoietic tissues and iron deposition sites. Transferrin is synthesized by the liver. It is responsible for transporting iron absorbed in the liver, as well as iron coming from destroyed red blood cells for reuse by the body. Under physiological conditions, only about 30% of the iron-binding capacity of plasma transferrin is used.
Iron is deposited in the body in the form of ferritin proteins (most) and hemosiderin. Ferritin is iron oxide/hydroxide enclosed in a protein shell, apoferritin. It is found in virtually all cells, providing a readily available reserve for the synthesis of iron compounds and presenting iron in a soluble, non-ionic, non-toxic form. The cells richest in ferritin are the precursors of erythrocytes in the bone marrow, macrophages and reticuloendothelial cells of the liver. Hemosiderin is found in macrophages of the bone marrow and spleen, liver cells. It is considered as a smaller form of ferritin, in which the molecules have lost part of the protein shell and clustered together. The rate of iron mobilization from hemosiderin is slower than from ferritin. With an excess of iron in the body, its proportion increases, which is deposited in the liver in the form of hemosiderin.
The body's ability to excrete iron is limited. Most of the iron from degrading erythrocytes (more than 20 mg daily) again enters hemoglobin. The total loss of iron during desquamation of skin and intestinal cells reaches about 1 mg per day, about 0.4 mg is excreted in feces, 0.25 mg in bile, less than 0.1 mg in urine. These losses are common for men and women. In addition, each woman loses 15-25 mg of iron during one menstruation. During pregnancy and lactation, she needs an additional 2.5 mg of iron per day. Taking into account that the daily intake of iron with food is only 1-3 mg, during these physiological periods, women have a negative iron balance. As a result, by the age of 42-45 years, a woman approaches with a pronounced iron deficiency.
Iron-deficiency anemia
Iron deficiency occurs as a result of a mismatch between the body's need for iron and its intake (or loss). There are two stages in the development of iron deficiency:
- latent iron deficiency - the level of ferritin iron and transferrin saturation are reduced, the hemoglobin level is reduced, there are no clinical signs of iron deficiency;
- iron deficiency anemia (clinically pronounced iron deficiency) is a disease in which the iron content in the blood serum, bone marrow and depot decreases; as a result, the formation of hemoglobin is disrupted, hypochromic anemia and trophic disorders in tissues occur.
The most common causes of iron deficiency anemia in adults
- Blood loss - repeated and prolonged bleeding uterine, gastrointestinal (peptic ulcer, hemorrhoids, ulcerative colitis), pulmonary (cancer, bronchiectasis).
- Increased iron consumption - pregnancy, lactation, intensive growth, puberty, chronic infectious diseases, inflammatory processes and neoplasms.
- Violation of the absorption of iron - resection of the stomach, enteritis; taking medications that reduce iron absorption.
- Decreased amount of iron from food.
The most common causes of iron deficiency anemia in children
In children, the need for iron per 1 kg of body weight is much greater than in adults, since the child's body needs iron not only for hematopoiesis processes, but also for intensive tissue growth. So, a child in the first half of life should receive at least 6 mg of iron per day (60% of the daily requirement of an adult), in the second half of the year - 10 mg (as an adult), in adolescence (11-18 years old) - 12 mg per day.
Due to the greater need, children suffer from a lack of iron much more than adults. According to available data, about 60% of preschool children and a third of schoolchildren suffer from iron deficiency anemia in Ukraine. The main causes of iron deficiency in children of all age groups are:
- insufficient intake of iron in the body of the fetus (premature pregnancy, anemia in the mother, late toxicosis of pregnancy);
- artificial feeding (in children under 1 year old);
- acute and/or chronic infectious diseases;
- unbalanced nutrition - the predominance of flour and dairy dishes in the diet, in which the iron content is relatively low;
- insufficient consumption of meat products;
- intensive growth.
Symptoms of hidden iron deficiency
Latent iron deficiency occurs most often in childhood, as well as in adolescents and young women. Women lose 12-79 mg of iron per 1 menstrual bleeding (average 15 mg), losses during each pregnancy, childbirth and lactation - 700-800 mg (up to 1 g). Early signs of developing iron deficiency are:
- weakness, increased fatigue;
- anxiety, lack of concentration;
- decrease in working capacity;
- psychological lability;
- headaches in the morning;
- decreased appetite;
- increased susceptibility to infections.
Symptoms of iron deficiency anemia
If measures are not taken to prevent the development of iron deficiency in “risk groups”, iron deficiency is not compensated in the early stages, iron deficiency anemia (IDA) develops.
In the clinical picture of IDA, several specific symptoms and syndromes can be identified.
The characteristic specific (sideropenic) symptoms of iron deficiency include:
- taste perversion (use of chalk, clay, eggshells, toothpaste, raw cereals, raw meat, ice);
- perversion of smell (attract smells of dampness, lime, kerosene, exhaust gases, acetone, shoe polish, etc.).
Hypoxic syndrome occurs as a result of oxygen starvation of tissues with sufficient severity of anemia. It is manifested by the following symptoms:
- pallor of the skin and mucous membranes;
- cyanosis of the lips;
- dyspnea;
- tachycardia;
- stitching pains in the heart;
- weakness, constant feeling of fatigue;
- decrease in emotional tone;
- retardation of children in mental development.
The syndrome of epithelial tissue damage develops as a result of a decrease in the synthesis of iron-containing enzymes and a violation of tissue metabolism processes. Characteristic manifestations:
- dry skin;
- fragility, hair loss;
- fragility and striation of nails;
- cracks in the skin of the legs and arms;
- stomatitis;
- decreased muscle tone, muscle weakness;
- imperative urge to urinate, urinary incontinence when laughing and sneezing, bedwetting;
- damage to the stomach and intestines - unstable stool, impaired gastric secretion, in 50% of patients - atrophic gastritis.
Hematological syndrome- characteristic changes in the clinical analysis of blood.
Diagnostic criteria for iron deficiency anemia are:
- decrease in the number of erythrocytes to 1.5-2.0 x 1012 / l,
- a decrease in hemoglobin in children of the first 5 years of life below 110 g / l, in children older than 5 years and adults - below 120 g / l;
- decrease in color index is less than 0.85.
The frequency of the most common symptoms of IDA in different age groups
| IDA symptoms | Frequency (%) | ||
| adults | Children | Teenagers | |
| muscle weakness | 97 | 82 | - |
| Headache | 68 | - | 21 |
| Decreased memory | 93 | - | 8 |
| dizziness | 90 | - | 30 |
| Brief syncope | 17 | - | 3 |
| Arterial hypotension | 87 | 22 | - |
| Tachycardia | 89 | - | - |
| Shortness of breath on exertion | 89 | 48 | 51 |
| Pain in the region of the heart | 81 | - | - |
| Symptoms of gastritis | 78 | - | 4 |
| perversion of taste | 31 | 79 | - |
| Perversion of smell | 14 | 27 | - |
Measures to prevent iron deficiency conditions
A necessary component of the prevention of iron deficiency in all age groups is a good diet with a sufficient content of meat products.
Prevention of iron deficiency conditions in children should begin even before birth, for which it is recommended that women take iron supplements throughout the entire period of pregnancy, especially in the last trimester.
Prevention of iron deficiency conditions, especially in children, reduces their risk of infectious diseases, contributes to a more complete mental and physical development of the child.
Principles of rational therapy of iron deficiency anemia
It is impossible to eliminate iron deficiency, and even more so iron deficiency anemia, without iron supplements - only a diet consisting of iron-rich foods. Iron from drugs can be absorbed 15-20 times more than from food.
In the treatment of iron deficiency conditions, preference is given to oral iron preparations. Treatment with iron preparations should be started with low doses, increasing them after a few days to avoid overdose and toxic reactions.
To correct iron deficiency conditions, the body should receive about 0.5 mg of iron per kg of body weight daily. Since only 10% of iron is normally absorbed from the gastrointestinal tract, and up to 25% of iron in anemia, about 2 mg / kg of body weight should be prescribed, which is 100-200 mg Fe (II) per day in adults. Higher doses are pointless (because iron absorption is limited by physiological mechanisms) and only increase the side effects.
You should not stop treatment with iron preparations after the normalization of hemoglobin and red blood cells: in order to create a "depot" in the body, you should continue taking the drugs for another 1-2 months.
Possible side effects when taking iron supplements
When taking oral iron preparations, a number of side effects can occur:
- gastrointestinal disorders: nausea, vomiting, intestinal colic, diarrhea / constipation;
- darkening of teeth;
- false reaction to occult blood in the feces;
- flushing of the face, a feeling of heat (rarely);
- allergic reactions (rarely);
- decrease in blood pressure;
- tachycardia.
The most common dyspeptic disorders (in 50% of patients) associated with the irritating effect of iron ions on the mucosa of the gastrointestinal tract. It should be noted that the severity of side effects from the gastrointestinal tract is associated with the amount of unabsorbed drug: the better the drug is absorbed, the better it is tolerated and gives fewer side effects.
iron poisoning
Acute poisoning with oral iron preparations in adults is extremely rare. However, since many iron preparations are attractively shaped, severe poisoning in children is possible if large amounts of the drug are accidentally taken. Ingestion of more than 2 g is fatal, with intake of less than 1 g (ferrous sulfate) within one to several hours, hemorrhagic gastroenteritis develops, necrosis with nausea, bloody vomiting, bloody diarrhea and circulatory shock. Death can occur within 8-12 hours after ingestion. After poisoning, sharp scars in the stomach area (pyloric stenosis) and significant liver damage often remain.
| Product | Content iron (mg/100 g) |
Product | Content iron (mg/100 g) |
| Pork liver | 12 | Buckwheat | 8 |
| beef liver | 9 | oatmeal | 4 |
| Meat | 4 | Semolina | 2 |
| A fish | 0,5-1 | Bread | 3-4 |
| chicken eggs | 2-3 | cocoa powder | 12 |
| Peas | 9 | Vegetables | 0,5-1,5 |
| Beans | 12 | Fruit | 0,3-0,5 |
| Soya | 12 |
Treatment includes induction of vomiting, ingestion of milk and eggs to form an iron-protein complex, gastric lavage with 1% NaHCO3 solution to form sparingly soluble iron carbonate. Further give deferoxamine 5-10 g in 100 ml of saline through a gastric tube, as well as 0.5-1 g intramuscularly or, if the patient is in shock, 15 mg/kg/h as a long-term infusion for 3 days.
Deferoxamine is a weak base with high selectivity for iron and forming chelate compounds with it, which are not absorbed in the intestines and are easily removed from the blood through the kidneys.
Criteria for the effectiveness of iron therapy
The effectiveness of iron preparations is judged by laboratory criteria - the results of a blood test in dynamics. By the 5-7th day of treatment, the number of reticulocytes (young red blood cells) should increase by 1.5-2 times compared with the initial data. Starting from the 7th-10th day of therapy, the hemoglobin content increases, after 2-4 weeks there is a positive trend in the color index.
Clinical signs of improvement appear much earlier (after 2-3 days) compared to the normalization of hemoglobin levels. This is due to the intake of iron in enzymes, the deficiency of which causes muscle weakness.
Comparative characteristics of iron preparations for oral use
Numerous iron preparations presented on the pharmaceutical market of Ukraine can be divided into groups depending on their composition and clinical and pharmaceutical properties.
Comparative characteristics of iron-containing preparations for internal use
| Tradename | The composition of the dosage form | Release form | |
| BIVALENT IRON PRODUCTS | |||
| MEDICINES CONTAINING IRON SULFATE | |||
| Hemopher prolongatum | Ferrous sulfate | 325 mg | Dragee |
| MEDICINES CONTAINING IRON CHLORIDE | |||
| Hemopher | Ferric chloride | 157 mg/ml | |
| MEDICINES CONTAINING IRON FUMARATE | |||
| Heferol | Ferrous fumarate | 350 mg | Capsules |
| PRODUCTS CONTAINING IRON GLUCONATE | |||
| Ferronal | Iron gluconate | 0.3 g | Tablets |
| Iron oxide sucrose solution (iron wine) | Iron saccharate | 73.9 g/kg | Solution for internal use |
| Rafinated sugar | 107.8 g/kg | ||
| COMPLEX PREPARATIONS CONTAINING BIVALENT IRON | |||
| Aktiferrin | Iron(II) sulfate | 113.85 mg | Capsules |
| D, L - serine | 129 mg | ||
| Iron(II) sulfate | 47.2 mg/ml | Drops | |
| D, L - serine | 35.6 mg/ml | ||
| Iron(II) sulfate | 171 mg/5 ml | Syrup | |
| D, L - serine | 129 mg/5 ml | ||
| Gino-Tardiferon | Iron(II) sulfate | 256.3 mg | Dragee |
| folic acid | 0.35 mg | ||
| Ascorbic acid | 30 mg | ||
| Mucoproteosis | 80 mg | ||
| Sorbifer Durules | Iron(II) sulfate | 320 mg | Coated tablets |
| Ascorbic acid | 60 mg | ||
| Tardiferron | Iron(II) sulfate | 256.3 mg | Depot tablets |
| Ascorbic acid | 30 mg | ||
| Mucoproteosis | 80 mg | ||
| Fenotek | Iron(II) sulfate | 150 mg | Capsules |
| Ascorbic acid | 50 mg | ||
| Riboflavin | 2 mg | ||
| Thiamine mononitrate | 2 mg | ||
| Nicotinamide | 15 mg | ||
| Pyridoxine hydrochloride | 1 mg | ||
| Calcium pantothenate | 2.5 mg | ||
| Ferroplex | Iron(II) sulfate | 50 mg | Dragee |
| Ascorbic acid | 30 mg | ||
| Vitafer | Iron(II) fumarate | 175 mg | Capsules |
| Ascorbic acid | 75 mg | ||
| cyanocobalamin | 30 mcg | ||
| folic acid | 200 mcg | ||
| Thiamine chloride | 3.5 mg | ||
| Riboflavin | 3.5 mg | ||
| Nicotinamide | 15 mg | ||
| Pyridoxine hydrochloride | 2 mg | ||
| Calcium pantothenate | 5 mg | ||
| Ranferon | Iron(II) fumarate | 305 mg | Capsules |
| folic acid | 0.75 mg | ||
| cyanocobalamin | 5 mcg | ||
| Ascorbic acid | 75 mg | ||
| zinc sulfate | 5 mg | ||
| Totem | Iron(II) gluconate | 5 mg/ml | Solution for internal use |
| manganese gluconate | 0.133 mg/ml | ||
| Copper gluconate | 0.07 mg/ml | ||
| TERIC IRON PRODUCTS | |||
| Maltofer | 50 mg/5 ml | Drops | |
| Iron (III) in the form of hydroxide polymaltose complex | 10 mg/ml | Syrup | |
| Iron (III) in the form of hydroxide polymaltose complex | 100 mg | Tablets | |
| Ferramin-Vita | Iron (III) asparaginate (in terms of Fe (III) | 60 mg | Tablets |
| Riboflavin | 25 mg | ||
| Nicotinamide | 15 mg | ||
| folic acid | 0.2 mg | ||
| cyanocobalamin | 0.025 mg | ||
| Ferrostat | Iron (III) carboxy-methylcellulose | 0.028 g | Tablets |
| ferrum lek | Iron (III) in the form of hydroxide polymaltose complex | 50 mg/5 ml | Syrup |
| Iron (III) in the form of hydroxide polymaltose complex | 100 mg | Tablets | |
| MULTIVITAMIN PRODUCTS CONTAINING IRON | |||
| Vitrum | Iron | 18 mg | Coated tablets |
| Vitrum centuri | Iron | 9 mg | Coated tablets |
| Vitrum circus with iron | Iron | 15 mg | Tablets |
| Vitrum junior | Iron | 18 mg | Coated tablets |
| Vitrum prenatal | Iron | 60 mg | Effervescent tablets |
| Multibionta junior | Iron | 3 mg | Effervescent tablets |
| Multivitamins "Daily with iron" | Iron | 18 mg | Tablets |
| Multivitamins forte | Iron | 10 mg | Tablets |
| Multivitamins and Minerals | Ferrous sulfate | 5 mg | Tablets |
| Multivitamins with iron | Ferrous fumarate | 12.17 mg | Tablets |
Preparations containing divalent iron Fe (II): ferrous sulfate, ferrous fumarate, ferrous chloride, ferrous gluconate. Different drugs contain different amounts of iron, the ability of which to assimilate is not the same: 12-16% - in iron sulfate, 7-9% - in iron lactate, 5-6% - in iron chloride, 14-16% - in iron fumarate, 20 -22% - in iron gluconate.
A number of Fe(II) complex preparations contain mucoproteosis, prevent irritation of the gastrointestinal mucosa with iron ions, promote slow release of iron ions, increase its bioavailability and improve tolerability.
Ferrous iron preparations have a number of common disadvantages: they can cause darkening of teeth and gums in patients, dyspeptic symptoms (nausea, vomiting, epigastric pain, constipation or diarrhea), and allergic reactions such as urticaria. With an overdose of Fe(II) preparations, cases of severe poisoning are possible, especially in children, which is associated with the activation of free-radical oxidation processes and hyperproduction of active radicals. This leads to metabolic and functional disorders in the body, primarily in the cardiovascular system.
Preparations containing trivalent iron Fe (III). Trivalent iron is practically not absorbed in the gastrointestinal tract. However, complex organic compounds of Fe(III) with a number of amino acids, maltose are significantly less toxic than Fe(II), but no less effective. Immobilization of Fe(III) on amino acids ensures its resistance to hydrolysis in the gastrointestinal tract and high bioavailability due to the slow release of the drug and its more complete absorption, as well as the absence of dyspepsia.
It is rational to allocate polycomponent drugs, containing, along with iron ions, additional substances that promote erythropoiesis (group B vitamins - B6, B9, B12); stimulating iron absorption (ascorbic acid, succinic acid, amino acids); multivitamin preparations containing iron.
Pharmaceutical guardianship in the use of oral iron preparations
- Treatment with iron preparations is recommended under medical supervision.
- Treatment with iron preparations should be accompanied by periodic blood tests.
- Iron preparations are recommended for children after consulting a pediatrician.
- Iron deficiency anemia should be treated mainly with drugs for internal use (Fe II).
- The use of iron preparations should be combined with the optimization of the diet, with the mandatory introduction of meat dishes into the menu.
- You should not prescribe iron preparations to children against the background of inflammatory processes (ARVI, tonsillitis, pneumonia, etc.), since in this case iron accumulates in the focus of infection and is not used for its intended purpose.
- The inclusion of ascorbic acid in complex preparations of iron improves the absorption of iron (as an antioxidant, ascorbic acid prevents the conversion of Fe-II ions into Fe-III, which are not absorbed in the gastrointestinal tract) and reduces the prescribed dose. Iron absorption also increases in the presence of fructose, succinic acid.
- Taking combined preparations that, along with iron, contain copper, cobalt, folic acid, vitamin B12 or liver extract makes it extremely difficult to control the effectiveness of iron therapy (due to the hematopoietic activity of these substances).
- During pregnancy, the intake of multivitamin preparations containing iron (glutamevit, complevit, oligovit, etc.)
- Do not simultaneously prescribe drugs that form non-absorbable complexes with iron (tetracyclines, levomycetin, calcium preparations, antacids).
- Iron ions form insoluble salts that are not absorbed and then excreted with feces, with food components such as phytin (rice, soy flour), tannin (tea, coffee), phosphates (fish, seafood).
- Since iron forms complexes with phosphates, at excessively high doses in children, the absorption of phosphates can be reduced so much that this leads to rickets.
- It is rational to take iron preparations 30-40 minutes before meals, which contributes to better absorption. At the same time, with this mode, the occurrence of symptoms of an irritating effect on the gastric mucosa is more likely.
- Oral iron preparations should be taken at least 4 hours apart.
- Tablets and dragees containing iron should not be chewed!
- After taking iron preparations, you should rinse your mouth, and liquid preparations (syrups, solutions for internal use) are best used through a tube.
- Taking iron supplements by mouth leads to darkening of the stool and can give false positive results in tests for occult blood.
- The simultaneous administration of iron preparations orally and parenterally (intramuscularly and / or intravenously) should be completely excluded!
- Parenteral administration of iron preparations should be done only in a hospital!
- Iron preparations should be stored out of the reach of children.
Literature
- Bokarev I. N., Kabaeva E. V. Treatment and prevention of IDA in outpatient practice // Ter. archive.- 1998.- No. 4.- S. 70-74.
- Zmushko E. I., Belozerov E. S. Drug complications.- St. Petersburg: Peter, 2001.- 448 p.
- Kazakova L. M. Iron deficiency and prevention in the practice of a pediatrician. Guidelines.- M., 1999.- 23 p.
- Compendium 2001/2002 - drugs / Ed. V. N. Kovalenko, A. P. Viktorova.- K.: Morion, 2002.- 1476 p.
- Krasnova A. Iron inside us // Pharmacist.- 1998.- No. 19-20.- P. 59-61.
- Krivenok V. A necessary component of the treatment of iron deficiency anemia // Pharmacist. - 2002. - No. 18. - P. 44.
- Mikhailov I. B. Clinical pharmacology.- St. Petersburg: Folio, 1998.- 446 p.
- Fundamentals of Internal Diseases / Ed. I. A. Zupantsa.- Kh.: Prapor, 1999.- 82 p.
- Modern over-the-counter drugs / Ed. A. L. Tregubova.- M.: Gamma-S. A.", 1999.- 362 p.
- Shiffman F. J. Pathophysiology of blood. - M.-SPb.: "BINOM" - "Nevsky dialect", 2000.- 448 p.
A.G. RUMIANCEV 1,4 , d.m.s., prof., I.N. ZAKHAROVA 2 , MD, prof., V.M. CHERNOV 1.4, MD, prof., I.S. TARASOVA 1.4, MD, A.L. PATCHERS 2 , MD, prof. ON THE. KOROVINA 2 , MD, prof., T.E. BOROVIK 3.5 , MD, prof., N.G. ZVONKOVA 3.5, PhD, E.B. MACHNEVA 2 , S.I. LAZAREVA 6 , T.M. VASILYEV 6
1
FSBI "Federal Scientific and Clinical Center for Pediatric Hematology, Oncology and Immunology named after N.N. Dmitry Rogachev" of the Ministry of Health of Russia
2
SBEE DPO "Russian Medical Academy of Postgraduate Education" of the Ministry of Health of Russia
3
FGBNU "Scientific Center for Children's Health"
4
State Budgetary Educational Institution of Higher Professional Education "Russian National Research Medical University. N.I. Pirogov" of the Ministry of Health of Russia
5
GBOU VPO "First Moscow State Medical University named after A.I. THEM. Sechenov" of the Ministry of Health of Russia
6
GBUZ "Children's City Polyclinic No. 133" DZ of Moscow
Iron deficiency states (WHD) are widespread in all countries of the world, therefore doctors of almost all specialties need to know about this disease. Knowledge of iron deficiency anemia (IDA) and latent iron deficiency (LID) is especially important for a practicing pediatrician. The article presents data from domestic and foreign studies on the prevalence of IDA and LAD. The most significant factors influencing the prevalence of WDN among various population groups are discussed: gender, age, environmental, physiological, socio-economic factors.
Iron deficiency anemia (IDA) is a polyetiological disease, the occurrence of which is associated with iron deficiency (ID) in the body due to a violation of its intake, absorption or increased losses, characterized by microcytosis and hypochromic anemia. In turn, latent iron deficiency (LID) is an acquired condition in which there is a latent iron deficiency, a decrease in iron stores in the body and its insufficient content in tissues (sideropenia, hyposiderosis), but there is no anemia yet.
Iron deficiency states are a widespread pathology among the population of the entire globe. According to the World Health Organization (WHO), iron deficiency (ID) ranks first among the 38 most common human diseases. The highest risk of developing ID is in children (especially the first two years of life) and women of reproductive age. According to S. Osendarp et al. in the world, about 50% of preschool children and pregnant women have anemia. With an anemia frequency of 20%, ID exists in 50% of the population in the population, and with an anemia frequency of 40% or more, the entire population has various types of ID. According to studies by D. Subramanian et al., 9% of children in the first two years of life have IDA.
According to WHO experts, iron deficiency still remains one of the most significant malnutrition-related diseases in the world. Iron deficiency negatively affects the cognitive development of both young children and adolescents, damages immune mechanisms, which leads to an increase in the incidence of infectious diseases. If ID is present during pregnancy, various adverse outcomes are possible, both for the mother (increased risk of bleeding, sepsis, maternal death) and for the fetus (increased risk of perinatal mortality and low birth weight). Even in industrialized countries, most pregnant women have insufficient iron stores in their bodies. The presence of ID affects the physical performance and labor productivity of both men and women. WHO experts concluded that the economic consequences of iron deficiency make it obvious that this pathology should be prevented with the use of iron-fortified dietary supplements.
WHO experts have done a lot of work, as a result of which it was shown that anemia is more common in developing countries, two groups of the population are most susceptible to anemia - young children and pregnant women ( tab. one).
Due to the high prevalence of anemia, it is found in the practice of a doctor in almost any specialty. It is known that IDA accounts for 90% of all anemias in childhood and 80% of all anemias in adults. It was previously believed that all anemias in pregnant women are iron-deficient, however, later it was shown that IDA accounts for 60–70% of all anemias in this category of the population, and the rest of the anemias have a different origin.
As already noted, iron deficiency anemia is more common in developing countries than in developed ones. In India, for example, up to 88% of pregnant and 74% of non-pregnant women suffer from anemia, in Africa - about 50% of pregnant and 40% of non-pregnant women. In Latin America and the Caribbean, the prevalence of anemia in pregnant and non-pregnant women is about 40% and 30%, respectively.
Data on the prevalence of anemia in different age groups is not known in all countries, however, the prevalence among preschool children is usually the same or even higher than among pregnant women. According to WHO experts, the prevalence of IDA in the population can be moderate - from 5 to 19.9%, medium - from 20 to 39.9% and significant - 40% or more ( tab. 2). With anemia prevalence of more than 40%, the problem ceases to be only medical and requires action at the state level.
The prevalence of ID varies significantly depending on factors such as age, sex, physiological characteristics, existing diseases, environmental and socio-economic conditions.
Full-term babies are usually born with sufficient iron stores in the liver and hematopoietic tissue. Subsequently, breast milk provides a certain amount of iron to the baby's body. Despite the fact that breast milk has a relatively low iron content (0.2-0.4 mg / l), it is much better absorbed from breast milk (50% bioavailability) than from cow's milk. ID often develops after 6 months. in the event that untimely and incorrect introduction of complementary foods does not provide sufficient iron intake. Iron requirements, depending on body weight, are proportional to the growth rate of the child. This is why iron deficiency is most common during the preschool years and during puberty. Another rise in the prevalence of ID may occur in old age, when nutrition often deteriorates in quality and quantity.
The prevalence of ID depends on gender. Gender differences are most noticeable after the onset of puberty. After the onset of menarche in adolescent girls, often iron losses due to uterine bleeding are not adequately compensated for by an adequate diet. The WDN that occurred in the pubertal period persists in the future in 10-12% of women of reproductive age.
The physiological characteristics of the body also affect the incidence of anemia. The most noticeable differences are typical for pregnant women. Significant amounts of iron from a woman's body enter the placenta and fetus during pregnancy. This leads to an increase in iron requirements of about 700 - 850 mg for the entire pregnancy. Lactation leads to the loss of iron through breast milk (1 mg/day), therefore, for some women, ID that occurs during pregnancy may be aggravated during lactation. However, in terms of iron balance, lactational amenorrhea in healthy women compensates for the loss of iron through breast milk.
Scientists from various countries have conducted studies on the prevalence of WDN among various population groups. The studies varied in scope. In Japan, for 30 years, mandatory screening of school-age children has been carried out for the purpose of early detection of IDA. Published in 2012 by Igarashi T. et al. data showed the prevalence of anemia among schoolchildren in Japan: 0.26% in elementary school among boys, 0.27% in elementary school among girls, 1.21% in high school among boys. The prevalence of anemia in the second and third years of secondary school in girls was lower than in the first year of secondary school. V tab. 3 presents data on the prevalence of IDA in some developed and developing countries.
| Table 3. IDA prevalence in developed and developing countries | |||
| The country | Publication year, author |
Frequency, % |
Children's age |
| China | Zhu Y, Liao Q, 2004 |
20,8 | 6 months -1 year |
|
7,8 |
1–3 years | ||
| WHO | Corapci F. et al., 2010 | 20–25 | First 2 years of life |
| USA |
Baker R., Greer F., 2010 | 2,1 | From 1 year to 3 years |
|
2,0 |
|||
|
1,6 |
|||
| 0,9 | |||
| USA | Amy Zhu et al., 2010 |
7 |
1–2 years |
| 5 | 3–5 years | ||
| 4 | 6–11 years old | ||
| African Americans USA |
Angulo-Barroso R.M. et al., 2011 |
39,8 |
9 months |
| Ghana |
55 |
9 months | |
| Brazil |
Cotta R. et al., 2011 |
55 |
Children under 5 years old |
| China |
Angulo-Barroso R.M. et al., 2011 |
31,8 |
9 months |
| Japan |
Igarashi T. et al., 2012 |
1,05–7,1 |
7–15 years old |
V tab. 4 presents data on the prevalence of latent iron deficiency (LID) in some developed and developing countries.
|
Table 4. Prevalence of latent iron deficiency in developed and developing countries |
|||
| The country |
Publication year, author |
Frequency, % | Children's age |
| China | Zhu Y, Liao Q., 2004 |
65,5 |
6 months -1 year |
|
43,7 |
1–3 years | ||
| Norway | Hay G. et al., 2004 |
4,0 | 6 months |
|
12 |
1 year | ||
| USA | Baker R., Greer F., 2010 |
9,2 |
1–3 years |
|
7,3 |
Non-Hispanic White Americans | ||
|
6,6 |
Non-Hispanic Black Americans | ||
|
13,9 |
Mexican Americans | ||
Zhu Y.P. et al. in 2004, a large epidemiological study was conducted on the prevalence of WDN among children in China. 9,118 children aged 7 months to 7 years were examined. According to the results of the study, the prevalence of LAD and IDA was 32.5% and 7.8%, respectively. Moreover, the prevalence of LAD and IDA were the highest in newborns - 44.7% and 20.8%, respectively. In preschool children aged 4 to 7 years, the prevalence was lower: 26.5% had LVAD, and 3.5% had IDA. A comparison was made of the prevalence of WDN among children living in the city and in rural areas. Urban children had a higher prevalence of LAD than rural children, however, rural children had a higher prevalence of anemia.
A. Zhu et al. in their 2010 publication, they provide data on the prevalence of IDA in the United States, taken from the Center for Disease Control and Prevention for 1999–2000. In the United States, which is a developed country, the prevalence of IDA was also higher in young children (1-2 years old) - 7% and lower in older children (6-11 years old) - 4%.
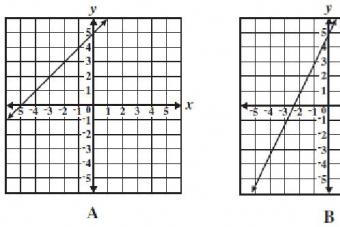
 Studies on the prevalence of WDN are also carried out in various regions of our country. So back in 1988, Yu.E. Malakhovskiy et al. published the results of a study of the frequency of IDA and LDZH in children. It is shown that by the end of the 80s. 20th century LJ frequency ( rice. one) and mild form of IDA ( rice. 2) among children of the first 6 months. life reached 40%. With age, there was a significant decrease in the incidence of ID (by the end of the 2nd year of life, IDA was recorded in more than 10% of children, and LVD - in more than 20%).
Studies on the prevalence of WDN are also carried out in various regions of our country. So back in 1988, Yu.E. Malakhovskiy et al. published the results of a study of the frequency of IDA and LDZH in children. It is shown that by the end of the 80s. 20th century LJ frequency ( rice. one) and mild form of IDA ( rice. 2) among children of the first 6 months. life reached 40%. With age, there was a significant decrease in the incidence of ID (by the end of the 2nd year of life, IDA was recorded in more than 10% of children, and LVD - in more than 20%).
Currently, according to various authors, it has been shown that the prevalence of WHD in children depends on the region, for example, LJD in some regions of the Russian Federation (North, North Caucasus, Eastern Siberia) reaches 50–60%. According to Yunusova I.M. (2002), the prevalence of IDA among the child population of various districts of Makhachkala was 43%.
Also, the frequency of WDN in our country was studied depending on the age group and gender. According to Tarasova I.S. (2013), the prevalence of anemia and the structure of WDN in adolescents have pronounced gender differences: anemia was detected in 2.7% of boys and 9% of girls, LAD - in 2.1 and 17.2%, respectively, IDA - in 2.7 and 7.3% respectively.
Socioeconomic conditions also influence the prevalence of WDN. So, according to Malova N.E. (2003), WDN are detected in 80.2% of young children in orphanages. In the structure of sideropenic conditions, the leading place is occupied by IDA - 59.3%, LAD was found in 40.7% of the examined children.
Thus, the accumulated world and domestic data on the prevalence of iron deficiency conditions show that it is high and depends on many factors: gender, age, environmental factors, socio-economic living conditions, the presence of pathological factors. This should be remembered by a practical doctor of any specialty in order to suspect and diagnose WDN in a timely manner for the purpose of adequate and early therapy. In addition, there is an obvious need for a systematic update of data on the prevalence of WDN based on epidemiological studies among various population groups, since the structure of factors affecting it changes over time.
Literature
Feeding and nutrition of infants and young children. Guidelines for the WHO European Region, with emphasis on the former Soviet countries. WHO Regional Publications, European Series, #87. WHO 2000, updated reprint 2003.
Osendarp S.J., Murray-Kolb L.E., Black M.M. Case study on iron mental development – in memory of John Beard (1947-2009). Nutr Rev. 2010; 68(1): 48–52.
Subramanian D.N., Kitson S., Bhaniani A. Microcytosis and possible early iron deficiency in pediatric inpatients: a retrospective audit. BMC Pediatr. 2009; 9:36.
UNICEF, United Nations University, WHO. Iron deficiency anemia: assessment, prevention and control. A guide for program managers. Geneva: World Health Organization; 2001 (WHO/NHD/01.3). – 114 p.Available at:http://www.who.int/nutrition/publications/micronutrients / anemia_iron_deficiency / WHO_NHD_01.3/en
Anemia in children: diagnosis, differential diagnosis, treatment. Ed. A.G. Rumyantsev and Yu.N. Tokarev. 2nd ed. add. and reworked. Moscow: MAKS Press; 2004. - 216 p.
Hurtle M. Differential diagnosis in pediatrics. Per. with him. Volume 2. M.: Medicine; 1990. - 510 p.
Guide to hematology. Ed. A.I. Vorobiev, 3rd edition, volume 3. M.: Nyudiamed; 2005. - 409 p.
Huh R, Breiman K. Anemia during pregnancy and the postpartum period. Per. from English. Tver: Triad; 2007. - 73 p.
Demikhov V.G. Anemia in pregnancy: differential diagnosis and pathogenetic substantiation of therapy. Abstract diss. … doc. honey. Sciences. Ryazan; 2003. - 45 p.
Tuermen T. Maternal mortality and morbidity due to anemia and postpartum haemorrhage. In: Prevention and management of anemia in pregnancy and postpartum haemorrhage. Huch A., Huch R., Breymann C., eds. Zurich: Schellenberg Verlag; 1998: 10–15
Igarashi T., Itoh Y., Maeda M., Igarashi T., Fukunaga Y. Mean haemoglobin levels in venous blood samples and prevalence of anaemia in japanese elementary and junior high school students. J. Nippon. Med. Sch. 2012; 79:232–235.
Baker R.D., Greer F.R. and The Committee on Nutrition. Clinical report - diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics. 2010; 126(5): 1040–1052.
Zhu Y, Liao Q. Prevalence of iron deficiency in children aged 7 months to 7 years in China. Zhonghua Erke Za Zhi. 2004; 42(12):886-91.
Corapci F., Calatroni A., Kaciroti N., Jimenez E., Lozoff B. Longitudinal evaluation of externalizing and internalizing behavior problems following iron deficiency in infancy. J. Pediatr. Psychol. 2010; 35(3): 296–305.
Zhu A., Kaneshiro M., Kaunitz J.D. Evaluation and treatment of iron deficiency anemia: a gastroenterological perspective. Dig. Dis. sci. 2010; 55:548–559.
Angulo-Barroso R.M., Schapiro L., Liang W., Rodrigues O., Shafir T., Kaciroti N., Jacobson S.W., Lozoff B. Motor development in 9-month-old infants in relation to cultural differences and iron status. dev. Psychobiol. 2011; 53:196–210.
Cotta RM, Oliveira F., Magalhães A., Ribeiro AQ, Sant "Ana LF, Priore SE, Franceschini Sdo.C. Social and biological determinants of iron deficiency anemia. Cad. Saúde Pública, Rio de Janeiro. 2011; 27 (2 ): 309–320.
Hay G., Sandstad B., Whitelaw A., BorchIohnsen B. Iron status in a group of Norwegian children aged 6–24 months. acta. paediatr. 2004; 93(5): 592–598.
Malakhovskiy Yu.E., Manerov F.K., Sarycheva E.G. A mild form of iron deficiency anemia and latent iron deficiency are borderline conditions in children during the first two years of life. Pediatrics. 1988; 3:27–34.
Gorodetsky V.V., Godulyan O.V. Iron deficiency states and iron deficiency anemia: treatment and diagnosis. M.: Medpraktika-M. 2008, pp. 1–27.
Zakharova N.O., Nikitin O.L. Iron deficiency anemia in elderly and senile patients: pos. for doctors. Samara. 2008. 60 p.
Yunusova I.M. Prevalence and structure of clinical forms of iron deficiency anemia in children in microdistricts of Makhachkala. Abstract diss. … cand. honey. Sciences. Moscow. 2002. 25 p.
Tarasova I.S. Development and scientific substantiation of screening for iron deficiency conditions in adolescents. Abstract dis. ... Dr. med. Sciences: Moscow. 2013. 67 p.
Malova N.E. Clinical and pathogenetic bases of differentiated therapy and prevention of iron deficiency anemia in young children. Abstract diss., Ph.D. honey. Sciences. Moscow. 2003. 25 p.
Sourcemk: Medical Council, No. 6, 2015
The primary prevention of iron deficiency is proper, nutritious nutrition.
Secondary prevention is the active detection of latent iron deficiency and IDA in the process of clinical examination, medical examinations.
1. Antenatal prophylaxis: according to WHO recommendations, an iron preparation at a dose of 60 mg / kg per day is used in the II and III trimesters of pregnancy and for 3 months of lactation (supplementation regimen).
In the menu of a pregnant woman, it should be recommended to include foods rich in protein - up to 120 g per day (meat, liver, cheese, fish), fruits, vegetables, vitamins and trace elements. Iron absorption is reduced by excessive consumption of large amounts of milk and plant foods.
2. Postnatal prophylaxis:
Non-specific preventive measures for IDA include: natural feeding with the timely introduction of complementary foods: assorted vegetable puree (potatoes, beets, carrots, cabbage, zucchini, etc.), pureed beef or calf liver mixed with vegetable puree from 5 months, meat minced meat from 7 months, etc. In the diet, white cereals (semolina, rice, oatmeal) should be limited, giving preference to buckwheat, barley, pearl barley, and millet. Porridge should be boiled in water or, better, in vegetable broth.
Specific preventive measures (taking iron supplements) for children at risk (premature, born from multiple pregnancies, etc.) should be started from 2 months of age, continuing it until the end of the first year of life; full-term children at risk from 4 months for 3-6 months.
The prophylactic dose of iron preparations for children under 3 years of age is 1-1.5 mg / kg per day, for children over 3 years old - 1/3 - ½ of the daily therapeutic dose of elemental iron (according to Shabalov N.P.).
Decreed terms for monitoring hematological parameters to confirm the effect of therapy: monthly hemoglobin during the period of dispensary observation (1 year), after 1, 3, 4 and 6 months from the start of therapy, control of the level of serum iron, TIBC and ferritin.
Vaccination is carried out after the normalization of hemoglobin levels (with reduced hemoglobin, vaccinations are immunologically ineffective).
Forecast. The prognosis of the disease is favorable, the cure should occur in 100% of cases. The so-called "relapses" of the disease are possible with: the use of low doses of iron preparations; ineffectiveness of oral ferropreparations; reducing the duration of treatment of patients; treatment of patients with chronic posthemorrhagic anemia with an unidentified and unidentified source of blood loss.