21-01-2013, 21:54
The classification of antibacterial drugs is based on their molecular structure, since structurally identical groups have similar pharmacodynamic and pharmacokinetic parameters. The classification of antibacterial drugs is presented in table. 11.

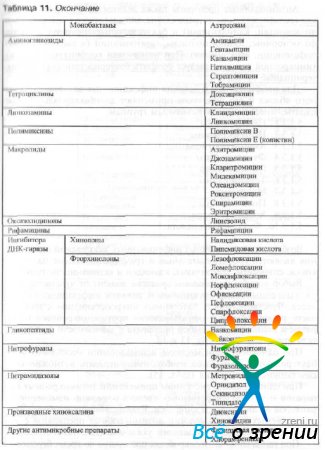
Table 11. Classification of antibacterial drugs
For the prevention and treatment of infectious diseases of the eyeball and its appendages, antibacterial drugs belonging to various groups are used.
- Penicillins
- Cephalosporins
- Aminoglycosides
- Fluoroquinolones
- Glycopeptides
- Tetracyclines
- Macrolides
- Polymyxins
- Chloramphenicol
- Fusidic acid.
The causative agents of various infectious diseases of the organ of vision are gram-negative and gram-positive rods and cocci, spirochetes, mycoplasma, chlamydia and actinomycetes (Table 12).
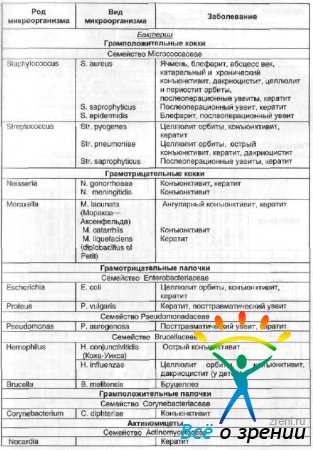
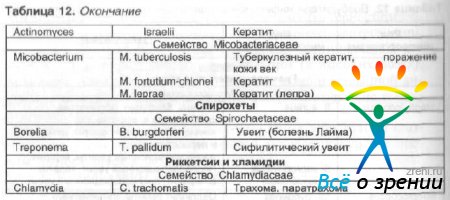
Table 12. Causative agents of infectious diseases of the organ of vision
The choice of antibacterial agent depends on the sensitivity of pathogenic microorganisms and the severity of the infectious process. The sensitivity of pathogenic microorganisms to the most commonly used antimicrobial drugs in ophthalmology and the rational choice of drug depending on the pathogen are presented in Table. 13 and 14.
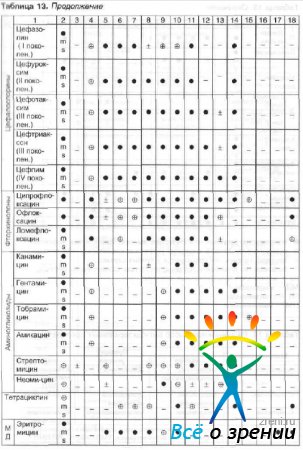

Table 13. Antimicrobial spectra
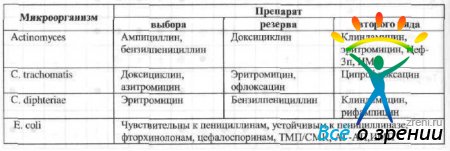

Table 14. Rational choice of antibacterial drugs
With the simultaneous local use of several antibacterial drugs, it is necessary to consider the possibility of their combined use (Table 15).

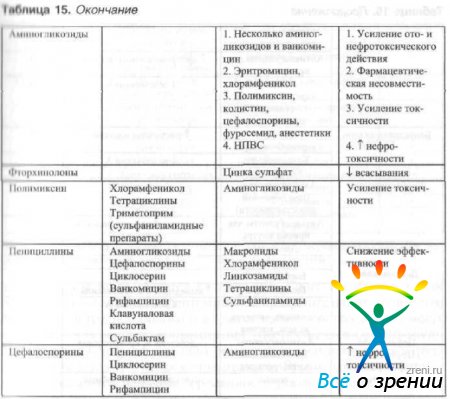
Table 15. The effectiveness of combined local use of antibacterial agents
With the simultaneous systemic use of antimicrobial drugs and other drugs, it is possible to change the parameters of their dynamics and kinetics. The interaction of the most commonly used antimicrobial drugs in ophthalmology with other drugs is indicated in Table. 16.
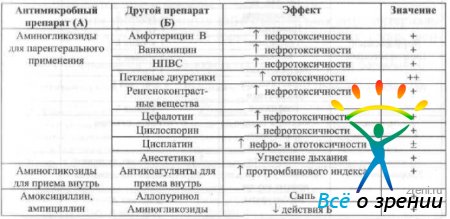
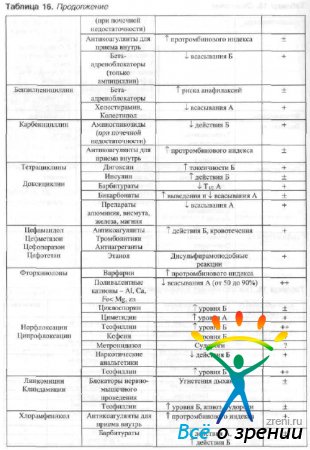
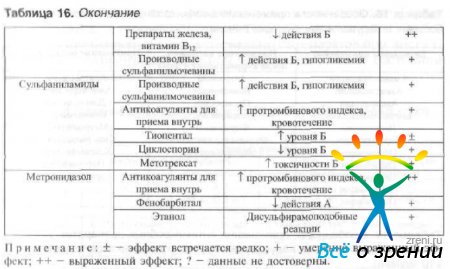
Table 16. Drug interactions
When prescribing antimicrobial drugs during pregnancy and lactation the transplacental transfer of the drug and its ability to be excreted in breast milk should be taken into account. Oxacillin is not excreted in breast milk. Antibiotics such as gentamicin, colistin, streptomycin pass into breast milk in small quantities and small concentrations of these drugs (up to 0.05 mg/l) can be detected in the blood plasma of newborns. Ampicillin, benzylpenicillin, and erythromycin accumulate in breast milk in significant concentrations. Recommendations for the use of drugs during pregnancy are indicated in table. 17.
Table 17. Use of antimicrobial drugs during pregnancy
When prescribing antimicrobial drugs to patients with liver and kidney diseases, it is important to know the features of their kinetics. Recommendations for dosing of antimicrobial drugs in this group of patients are presented in Table. 18 and 19.
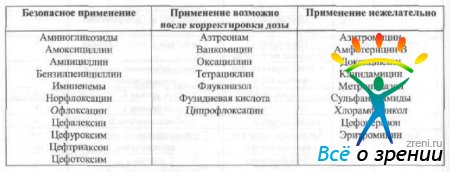
Table 18. Features of the use of antimicrobial drugs in patients with impaired liver function
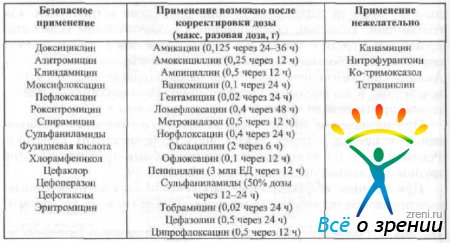
Table 19. Features of the use of antimicrobial drugs in patients with severe renal impairment (creatinine clearance<10 мл/мин)
In the treatment of infectious eye diseases, antibacterial drugs are used not only in the form of eye dosage forms (eye drops, ointments and films), but also injection (subconjunctival, parabulbar, intramuscular and intravenous injections) and intraocular administration of drugs are widely used.
When administered parenterally, it is necessary to take into account the ability of the drug to penetrate the blood-ophthalmic barrier. Chloramphenicol, sulfonamides, penicillins, aminoglycosides, lincomidin, cephalosporins, fluoroquinolones penetrate the blood-ophthalmic barrier well; tetracyclines, erythromycin, and polymyxins penetrate the barrier poorly. The average doses of the most commonly used antibacterial drugs for instillation, subconjunctival, intraocular and systemic use are shown in Table. 20.
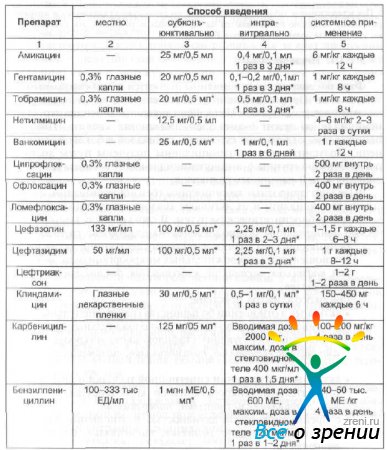
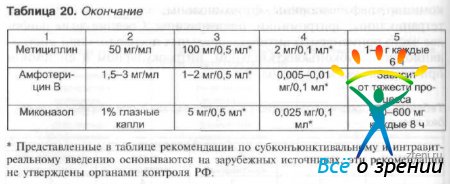
Table 20. Average doses of antibiotics for adults by different routes of administration
Penicillins
Pharmacodynamics: Penicillins are beta-lactam antibiotics. Natural penicillins are synthesized by certain types of molds (Penicillium notatum). The structure of penicillins is based on 6-aminoenicillanic acid. Penicillin homologs differ in the structure of the radicals in the amine side chain. Semi-synthetic penicillins are obtained by acetylation of the amino group of 6-aminopenicillanic acid and the addition of various radicals to it.
There are natural penicillins (benzylpenicillin, phenoxymethylpenicillin) and their active analogs obtained synthetically or biosynthetically. In turn, semisynthetic penicillins are divided into the following groups:
- penicillinase-resistant with preferential activity against gram-positive microorganisms: methicillin, nafcillin, oxacillin, cloxacillin, dicloxacillin, flucloxacillin;
- wide spectrum of action:
- active against most gram-negative (except Pseudomonas aeruginosa) and gram-positive (except penicillinase-forming staphylococci) microorganisms: ampicillin, hetacillin, pivampicillin, talampicillin, amoxicillin;
- active against Pseudomonas aeruginosa and other gram-negative microorganisms: carbenicillin, ticarcillin, azlocillin, mezlocillin, piperacillin;
- with preferential activity against gram-negative bacteria: mecillin, pivmecillin, bakmecillin, acidocillin;
- combination antibiotics: ampiox;
- acid-fast antibiotics, but inactivated by penicillinase: pheneticillin, propicillin.
The spectrum of antibacterial action depends on the structure of penicillins and differs between natural and semi-synthetic drugs (for more details, see Table 13).
Penicillins disrupt the process of cell wall biosynthesis by stopping the synthesis of peptoglycan in the cell wall of microorganisms. They act both on microorganisms located inside the tag and outside the cell. The effect on intracellular microorganisms is less pronounced.
Resistance to penicillins develops due to the production of the enzyme - penicillinase(beta-lactamase), which destroys peptide bonds in the penicillin molecule and deprives it of its bactericidal effect.
Some semisynthetic penicillins are resistant to the action of penicillinase; in addition, to increase the effectiveness of penicillinase-sensitive penicillins, they are used in conjunction with penicillinase inhibitors (clavulanic acid, sulbactam).
Pharmacokinetics: Penicillins do not penetrate the blood-ophthalmic barrier well. However, against the background of the inflammatory process, their penetration into the internal structures of the eye increases, and the concentration of penicillins in the eye tissues can reach a therapeutically significant level. Penicillins are excreted primarily by the kidneys (80% through the renal tubules, 20% by glomerular filtration). Small amounts are excreted in bile.
When penicillin solutions are instilled into the conjunctival sac, they are found in therapeutic concentrations in the corneal stroma; penicillins practically do not penetrate into the moisture of the anterior chamber of the eye when applied topically.
With subconjunctival administration, therapeutic concentrations are determined in the cornea and the humor of the anterior chamber. In the vitreous body, the concentration of penicillins is below the therapeutic level.
With intravitreal administration, the half-life is about 3 hours. With parallel systemic use of penicillinase inhibitors, the half-life increases. The minimum concentration of penicillin that causes toxic damage to the retina is 5000 units.
Indications- penicillins are used to treat:
- gonococcal conjunctivitis (benzylpenicillin);
- canaliculitis, especially caused by actinomycetes (benzylpenicillin, phenoxymethylpeniillin);
- abscess and phlegmon of the orbit (phenoxymethylpeniiillin, methicillin, oxycillin, cloxacillin, nafcillin, dicloxacillin, a combination of ampicillin and clavulanate, ampicillin and sulbactam, ticarcillin and clavulanate);
- keratitis (benzylpenicillin, methicillin, oxycillin, ampicillin, ticarcillin, piperacillin);
- damage to the organ of vision due to Lyme disease (benzylpenicillin);
- damage to the organ of vision due to syphilis (benzylpenicillin).
Penicillins are also used to prevent infectious complications in injuries of the eyelids and orbit, especially when foreign bodies penetrate into the orbital tissue (a combination of ampicillin and clavulanate, ampicillin and sulbactam, ticarcillin and clavulanate).
Contraindications: hypersensitivity to penicillin antibiotics and cephalosporins.
Semi-synthetic antibiotics are contraindicated for:
- infectious mononucleosis;
- lymphocytic leukemia;
- liver dysfunction;
- bronchial asthma;
- severe allergic diathesis (amoxicillin, carbenicillin, ampicillin, oxacillin);
- nonspecific ulcerative colitis (carbenicillin).
Features of application (should be taken into account, first of all, for systemic use).
Amoxicillin in combination with metronidazole is not recommended for use in persons under 18 years of age.
The safety of carbenicillin in pediatrics has not been established.
Decreased renal function and metabolic activity in the elderly may require penicillin dosage adjustments.
In case of renal and/or liver failure, drug accumulation is possible. In case of moderate and severe insufficiency of renal and/or liver function, dose adjustment of drugs and lengthening of the periods between administrations are required.
Use during pregnancy is possible only when the expected benefit to the mother outweighs the potential risk to the fetus.
If necessary, use during lactation should stop breastfeeding.
Side effects:
- Allergic reactions - urticaria, erythema, Quincke's edema, rhinitis, conjunctivitis. In rare cases, fever, joint pain, eosinophilia may develop, and in isolated cases, anaphylactic shock.
- Effects associated with chemotherapeutic action - the development of superinfection. With systemic use, the development of candidiasis of the oral cavity, vagina, and intestinal dysbiosis is possible.
- From the digestive system - with systemic use, nausea, vomiting, and diarrhea occur.
- From the side of the central nervous system - nausea, vomiting. Increased reflex excitability, symptoms of meningism, convulsions, coma. Neurotoxic effects develop when benzylpenicillin is used in high doses, especially when administered endolumbarally.
- From the blood coagulation system - hemorrhagic syndrome. Observed when using carbenicillin in patients with impaired renal function.
- From the side of input-electrolyte metabolism - hyponatremia or hypokalemia. Observed when using carbenicillin in high doses.
- From the urinary system - hematuria, proteinuria, interstitial nephritis. Observed when using oxacillin.
- When amoxicillin is used in combination with clavulanate, cholestatic jaundice may develop.
- Local reactions - burning.
Directions for use and doses: penicillins in ophthalmology are used parenterally, orally, in the form of eye drops, and are also administered subconjunctivally and intravitreally. Doses for oral and parenteral administration correspond to the average doses used to treat other bacterial diseases.
In the form of eye drops, penicillins are used to treat diseases of the conjunctiva and cornea. The frequency of instillation depends on the severity of the inflammatory process.
In case of a moderately severe infection, 1-2 drops of the drug are injected into the conjunctival sac every 4 hours or a strip of ointment 1.5 cm long is placed behind the lower eyelid of the affected eye 2-3 times a day. If a severe infectious process develops, the drug is instilled every hour or the ointment is placed behind the lower eyelid every 3-4 hours. As the inflammation decreases, the frequency of drug instillations is reduced. Duration of use is no more than 14 days.
Penicillin solutions are used to wash the lacrimal ducts in the treatment of canaliculitis.
Solutions for topical use are prepared ex temporae.
- Benzylpenicillin [MNI]
A solution containing 100,000-333,000 units/ml is instilled into the conjunctival sac (in pediatrics, solutions containing 10,000-20,000 units/ml are used to treat gonoblennorrhea in newborns). To prepare a solution for instillation, dissolve 500,000 units in 5 ml of saline solution. To prepare a solution used for instillation in pediatrics, 250,000 units are dissolved in 5 ml of saline, then 1 ml of the resulting solution is taken and saline is added to 5 ml.
0.5-1 million units/0.5 ml is administered subconjunctivally.
No more than 2000 units of benzylpenicillin are administered intravitreally. To prepare a solution for intravitreal administration, 250,000 units are dissolved in 5 ml of physiological solution, then 1 ml of the resulting solution is taken and physiological solution is added to 12 ml. No more than 0.5 ml of the resulting solution is injected intravitreally. At the same time, probenecid 0.5 g is prescribed orally 4 times a day.
- Methicillin [INN]
A solution containing 50 mg/ml is instilled into the conjunctival sac.
75-100 mg/0.5 ml is administered subconjunctivally.
No more than 2 mg of methicillin is administered intravitreally. At the same time, probenecid 0.5 g is prescribed orally 4 times a day.
- Oxacillin [INN]
A solution containing 66 mg/ml is instilled into the conjunctival sac. To prepare a solution for instillation, 250 mg of the substance is dissolved in 4 ml of physiological solution.
75-100 mg/0.5 ml is administered subconjunctivally. To prepare a solution, 250 mg of the substance is dissolved in 2 (1.5) ml of physiological solution or 500 mg of the substance is dissolved in 3.0 (2.5) ml of physiological solution.
No more than 500 mcg of oxacillin is administered intravitreally. To prepare a solution for intravitreal administration, 250 mg of the substance is dissolved in 5 ml of physiological solution, then 1 ml of the resulting solution is taken and physiological solution is added to 10 ml. Next, take 1 ml of the resulting solution and add physiological solution to 5 ml. No more than 0.5 ml of the resulting solution is injected intravitreally.
- Ampicillin [INN]
A solution containing 50 mg/ml is instilled into the conjunctival sac. To prepare a solution for instillation, 250 mg of the substance is dissolved in 5 ml of physiological solution.
100 mg/0.5 ml is administered subconjunctivally. To prepare a solution, 250 mg of the substance is dissolved in 1.5 ml of physiological solution or 500 mg of the substance is dissolved in 2.5 ml of physiological solution.
No more than 5000 mkg of ampicillin is administered intravitreally. To prepare a solution for intravitreal administration, 250 mg is dissolved in 5 ml of physiological solution, then 1 ml of the resulting solution is taken and physiological solution is added to 5 ml. No more than 0.5 ml of the resulting solution is injected intravitreally.
- Ticarcillin [INN]
A solution containing 6-20 mg/ml is instilled into the conjunctival sac.
Subconjunctivally inject 100 mg/0.5 ml.
- Pineracillin (INN)
A solution containing 6-20 mg/ml is instilled into the conjunctival sac. To prepare a solution for instillation, 2 g of the substance is dissolved in 10 ml of physiological solution. Next, take 1 ml of the assigned solution and add physiological solution to 10 ml.
100 mg/0.5 ml is administered subconjunctivally. To prepare the solution, 2 g of the substance is dissolved in 5 ml of physiological solution.
- Carbenicillin [INN]
No more than 1000-2000 mcg of carbenicillin is administered intravitreally. To prepare a solution for intravitreal administration, 1 g of the substance is dissolved in 10 ml of physiological solution, then take 1 ml of the resulting solution and add physiological solution to 10 ml. Next, take 1 ml of the resulting solution and add physiological solution to 5 ml. No more than 0.5 ml of the resulting solution is injected intravitreally.
Interaction with other drugs.
When used together with bacteriostatic drugs (macrolides, chloramphenicol, lincosamides, tetracyclines, sulfonamides), the bactericidal effect is reduced.
Penicillins (ampicillin, oxacillin) reduce the effectiveness of oral contraceptives. Probenecid, diuretics, allopurinol, phenylbutazone, NSAIDs can increase plasma concentrations of penicillins. Antacids, glucosamine, laxatives and aminoglycosides slow down the absorption of oral penicillins. Oral penicillins enhance the effect of indirect anticoagulants. Carbenicillin enhances the antiplatelet properties of NSAIDs.
Pharmaceutical incompatibility occurs when combining aminoglycosides and carbenicillin.
The combination of penicillins with bactericidal antibiotics and penicillinase inhibitors leads in most cases to a change in activity. The optimal combination is a combination of penicillins and aminoglycosides, cephalosporins, cycloserine, vancomycin, rifampicin, clavulanic acid, sulbactam.
Drugs
- Benzylpenicillin sodium salt (Russia) - powder for the preparation of solution for injection 250,000, 500,000 and 1,000,000 units;
- Oxacillin (Russia) - powder for the preparation of solution for injection, 250 and 500 mg;
- Pipracil (Lederle, USA) - powder for the preparation of a solution for injection of 2 and 4 g of piperacillin;
- Carbenicillin sodium salt (Russia) - powder for the preparation of solution for injection 1 g.
Antibacterial drugs are derivatives of the vital activity of microorganisms or their semi-synthetic and synthetic analogs that can destroy microbial flora or inhibit the growth and reproduction of microorganisms. Antibacterial therapy is a type of chemotherapy and requires the correct approach to treatment based on the kinetics of absorption, distribution, metabolism and excretion drugs, on the mechanisms of therapeutic and toxic effects of drugs.
If we take into account the way in which these drugs fight the disease, the classification of antibiotics according to the mechanism of action divides them into: drugs that disrupt the normal functioning of cell membranes; substances that stop the synthesis of protein and amino acids; inhibitors that destroy or suppress the synthesis of cell walls of all microorganisms. According to the type of effect on the cell, antibiotics can be bactericidal and bacteriostatic. The former very quickly kill harmful cells, the latter help slow down their growth and prevent reproduction. The classification of antibiotics by chemical structure takes into account groups according to the spectrum of action: beta-lactam (natural, semi-synthetic, broad-spectrum substances), which have different effects on microbes; aminoglycosides that affect bacteria; tetracyclines that inhibit microorganisms; macrolides that fight gram-positive cocci, intracellular irritants, which include chlamydia, mycoplasma, etc.; ansamycins, especially active in the treatment of gram-positive bacteria, fungi, tuberculosis, leprosy; polypeptides that stop the growth of gram-negative bacteria; glycopeptides that destroy the walls of bacteria, stopping the synthesis of some of them; anthracyclines used for tumor diseases.
According to the mechanism of action, antibacterial agents are divided into 4 main groups:
1. Inhibitors of microbial cell wall synthesis:
§ penicillins;
§ cephalosporins;
§ glycopeptides;
§ fosfomycin;
§ carbapenems;
§ bacitracin.
Drugs that destroy the molecular organization and function of cytoplasmic membranes:
§ polymycosins;
§ some antifungal agents.
3. Antibiotics that inhibit protein synthesis:
§ aminoglycosides;
§ macrolides;
§ tetracyclines;
§ group of chloramphenicol (chloramphenicol);
§ lincosamides (lincosamines).
4. Medicines that disrupt the synthesis of nucleic acids:
§ ansamacrolides (rifamycins);
§ fluoroquinolones;
§ sulfonamide drugs, trimethoprim, nitromidazoles.
Depending on the interaction of the antibiotic with the microorganism, bactericidal and bacteriostatic antibiotics are distinguished.
Antimicrobial drugs are mostly antibiotics, the appearance of which opened a new era in practical medicine and led to a number of specific consequences both in the existence of microorganisms and in the course of a variety of diseases. The main problem in the use of these drugs is the formation of adaptive mechanisms in bacteria. Mainly this is enzymatic activity against antibiotics and immunity to these agents. Insensitivity can be isolated and cross, when one type of microbe is resistant to several groups of antibacterial agents. The problem of allergies to antibiotics and intolerance to them has also become relevant. The extreme degree of this phenomenon is polyallergy, when it is generally impossible to treat the patient with drugs of this class.
An alternative direction was the use bacteriophages. This extracellular life form is akin to viruses. Each type of bacteriophage devours its own type of bacteria, causing microbial addiction to a lesser extent. Phages exist both in isolation and in mixed solutions supplied with a preservative.
The practice of self-treatment with antibiotics, which has slowed down somewhat in recent years due to the transfer of these drugs to the prescription class, should be considered completely vicious. Any antibiotic should be prescribed according to indications, taking into account not only the sensitivity of infectious agents, but also taking into account the characteristics of the patient. The doctor also takes into account the frequency of use of certain drugs in a given country or locality, which leads to differences in the immunity of the same microbes in different regions.
Antimicrobial drugs
I. Betalactam antibiotics.
Medicines with a bacteriostatic effect and a wide spectrum of activity. Block the exchange of proteins in microbial cell membranes. They block the transport of substances and weaken the protection of bacteria.
1. Natural (sodium and potassium salts of benzylpenicillin and phenoxymethylpenicillin). Used parenterally.
2. Semi-synthetic (flemoxin, ampicillin, amoxicillin, oxacillin, ticarcillin, carbenicillin). Tablet and injection forms.
3. Combined penicillins. Ampiox.
4. Inhibitor-protected (amoxicillin clavulonate: flemoclav, panclave, amoxiclav, augmentin; ampicillin sulbactam: unasin, sultamicillin, ampixide).
To protect against bacterial enzymes they contain clavulanic acid.
Bactericidal betalactam agents. These antibiotics act similarly to penicillins, disrupting the structure of the cell wall of microbes. Currently they are inferior to the group of macrolides, maintaining their position in the treatment of the urinary and upper respiratory tract.
First generation: cefazolin, cephalexin.
Second generation: cefuroxime, cefaclor.
Third generation: cefoperazone, ceftibuten, ceftriaxone, cefixime, cefotaxime, cefazidime.
Fourth generation: cefepime.
Resistant to betalactamases. Biapenem, imipenem, faropenem, ertapenem, doripenem, meropenem.
II. Tetracyclines. Bacteriostatics, the mechanism of action of which is based on the inhibition of protein synthesis. Tetracycline hydrochloride (tablets, ointment), doxycycline (capsules), oletethrin (tablets)
III. Macrolides. By binding to fats in the membranes, they disrupt the integrity of the latter. Clarithromycin, josamycin, azithromycin (azithromycin, azitral, hemomycin, sumamed).
IV. Aminoglycosides. As a result of disruption of protein synthesis in ribosomes, they have a bactericidal effect.
First generation: streptomycin, kanamycin, neomycin.
Second generation: sisomycin, tobramycin, gentamicin, netilmicin.
Third generation: amikacin.
V. Fluoroquinolones. The bactericidal effect is carried out on the basis of a block of bacterial enzymes. They also disrupt the synthesis of microbial DNA. Tsiprofloxacin (Zindolin, Quintor, Ircebro), Offloxacin (kirall, glaucos, zanocin), Lomefloxacin (Lomacin, Lomeflox, Xenakson), Norfloxacin (Loxson, Negaflox, Quinocasicin), Levofloxacin, Lefloxacin, Moxifloxacin, Gatifsacin , sparfloxacin (Sparflo).
Drugs to which microorganisms of different groups are less resistant. Ideally, they should be treated as reserve antibiotics along with anti-tuberculosis drugs. However, the commercial interests of pharmaceutical companies have brought them into the wider arena.
VI. Lincosamides. Bacteriostatic agents. Lincomycin, clindamycin. They act by binding to a component of the ribosomal membrane.
VII. Chloramphenicol (chloramphenicol). Due to its high toxicity to blood and bone marrow, it is mainly used topically (levomekol ointment).
VIII. Polymyxinv. bactericidal selectively against gram-negative flora. Polymyxin M, polymyxin B.
IX. Antituberculosis antibiotics. They are used against Pmycobacterium tuberculosis, although they are effective against a wide range of bacteria. Reserve drugs, that is, they try not to treat anything other than tuberculosis. Rifampin, isoniazid.
X. Sulfonamides. Sulfamidic acid amine derivatives. Today they are practically not used due to side effects.
XI. Nitrofurans. They have a bacteriostatic and, in high concentrations, a bactericidal effect. Affects gram-negative and gram-positive flora. The main areas of application are intestinal infections (furazolidone, enterofuril, nifuroxazide) and urinary tract infections (furomac, furomax, furadonin).
in the form of solutions they are used for local (rinsing, washing, lotions) and systemic oral administration. Drugs of choice for allergic reactions to antibiotics and dysbacteriosis. Klebsiella, staphylococcal, intestinal, pyobacteriophage, salmonella.
in solutions and sprays are widely used for disinfection of the oral cavity, skin, and wound treatment.
Self-medication with antimicrobial drugs is harmful by the development of multiple allergies, the cultivation of microbial populations in one’s own body that are insensitive to many antibacterial agents, and the risk of dysbiosis. Bacteria that survive after inadequate therapy can turn any acute inflammation into a long-term chronic infection and cause immune diseases.
Antibacterial are drugs created on the basis of natural antibacterial substances or semi-synthetically. They suppress the growth and reproduction of pathogenic bacteria and have no effect on viruses. Medicines in this group are used to treat infectious diseases. Based on their chemical structure, they are divided into many subgroups. According to the mechanism of action, they are divided into bactericidal (have a detrimental effect on microorganisms) and bacteriostatic (inhibit their growth).
Penicillin group drugs
Benzylpenicillin sodium salt
Active ingredient: benzylpenicillin sodium salt.
Pharmacological action: inhibits the growth and reproduction of gram-positive (streptococci, pneumococci, corynebacteria) and gram-negative bacteria (gonococci, meningococci, treponema). Does not affect staphylococcal species that produce penicillinase.
Indications: pneumonia, septic endocarditis, pleurisy, peritonitis, cystitis, syphilis, genitourinary infections.
Contraindications: hypersensitivity to the drug, heart rhythm disturbances, increased potassium levels in the blood.
Side effects: nausea, arrhythmias, allergic reactions.
Directions for use: administered intramuscularly, intravenously at a dose of 250,000–500,000 units 6 times a day.
For infective endocarditis – 30,000,000–40,000,000 units per day. For children – 50,000–100,000 units/kg body weight/day.
Release form: in the form of a powder for the preparation of an injection solution in bottles of 250,000, 500,000, 1,000,000 units.
Oxacillin
Active ingredient: oxacillin.
Pharmacological action: bactericidal – against gram-positive bacteria, gram-negative cocci, some types of actinomycetes. It is resistant to penicillinase.
Indications: sepsis, pneumonia, endocarditis, pericarditis, pleural empyema, osteomyelitis, cystitis, cholecystitis, syphilis, extensive burns.
Contraindications: hypersensitivity to drugs of the penicillin group, cephalosporins.
Side effects: nausea, vomiting, diarrhea, dysfunction of the liver, kidneys, yellowness of the skin and mucous membranes, suppression of bone marrow function, vaginal candidiasis, allergic reactions in the form of urticaria and skin itching.
Directions for use: orally, intravenously, intramuscularly 0.25-0.5 g 4-6 times a day for 7-10 days (the duration of treatment depends on the form and severity of the disease, the course of treatment can be extended to 2-3 weeks or even more) . The maximum dose is 3 g per day, but can be increased to 6–8 g in severe pathologies. For parenteral administration, the maximum dosage is 2–4 g per day.
Release form: powder for the preparation of injection solution, 0.25, 0.5 g in a bottle.
Special instructions: combined with benzylpenicillin, ampicillin. Bacteriostatic drugs significantly suppress the effects of oxacillin. Cannot be taken simultaneously with methotrexate.
Ampicillin
Active ingredient: ampicillin.
Pharmacological action: bactericidal - against gram-positive and gram-negative bacteria, not resistant to penicillinase.
Indications: community-acquired pneumonia, otitis media, tonsillitis, bronchitis, exacerbation of chronic obstructive pulmonary disease, cystitis, pyelonephritis, colitis, enterocolitis, salpingoophoritis, etc.
Contraindications: allergy to the drug, liver failure.
Side effects: skin rashes and other allergic reactions; with long-term treatment, due to a disturbance in the composition of the microflora, another infection may occur caused by microbes that are not sensitive to the drug or fungi.
Directions for use: tablets orally 30–60 minutes before meals. The dose of the drug may vary. Patients over 10 years of age are recommended to take 250–500 mg 4 times a day. A maximum of 2–3 g of the drug per day is allowed. For young children, the medicine is prescribed at a dose of 100 mg/kg body weight per day. The general course of treatment is 10–14 days.
Release form: tablets of 0.25 g - 20 pieces per package; capsules of 0.25, 0.5 g - 20 pieces per package.
Special instructions: use cautiously for allergies, bronchial asthma, as well as during pregnancy and breastfeeding.
Amoxin
Active ingredient: amoxicillin trihydrate.
Pharmacological action: has a detrimental effect on a wide range of microorganisms, affects the cell wall of bacteria, promoting its destruction. Acts on staphylococci (except those that produce the enzyme penicillinase), streptococci, gonococci, meningococci, E. coli, Shigella and salmonella.
Indications: bacterial diseases of the upper and lower respiratory tract (tracheitis, bronchitis, pneumonia), frontal sinusitis, sinusitis, inflammatory processes in the pharynx and tonsils, inflammation of the middle ear). The drug is also active against diseases of the kidneys and urinary tract (pyelonephritis, cystitis), and is effective against gonorrhea, infections of the female genital organs (colpitis, adnexitis). Can be used for inflammation of the gallbladder and bile ducts, in the complex treatment of peritonitis, for purulent infections of the skin and soft tissues (erysipelas, pustular diseases). Used for intestinal infections: salmonellosis, shigellosis (dysentery), for the prevention of endocarditis after surgery on the heart and large vessels or medical procedures. In addition, amoxin can be taken for inflammation of the meninges (meningitis) and bacterial infection of the blood.
Contraindications: allergic reactions (including intolerance to antibiotics of the cephalosporin group, carbapenems).
Side effects: allergies of varying severity, joint pain, fever, nausea, vomiting, inflammation of the oral mucosa, stool disorders, pain in the liver. With long courses of treatment, a disturbance in the composition of the intestinal microflora is possible. Rarely, when taking amoxin, sleep disturbances, changes in behavior, headache, and convulsions are observed. Sometimes there is a decrease in the number of red blood cells and white blood cells.
Directions for use: orally with water, before or after meals. For infections of the respiratory organs, kidneys and urinary tract, skin and soft tissues, patients weighing more than 40 kg are prescribed 500 mg of the drug 3 times a day for mild cases of the disease and 0.75-1 g for severe cases. For children under 10 years of age, it is advisable to give the drug in the form of a suspension (dissolve in 0.5 glasses of water): up to 2 years - 20-60 mg per 1 kg of body weight per day, from 2 to 5 years - 125 mg, and from 5 up to 10 years – 250 mg 3 times a day. The general course of treatment, depending on the severity of the infection, ranges from 5 to 14 days.
For gonococcal infection, amoxin is prescribed in a dose of 3 g once; in women, due to the high frequency of latent infection, this dose is taken twice.
For intestinal infections, cholecystitis and cholangitis, diseases of the genital organs in women (cervicitis, colpitis, inflammation of the appendages), the drug is taken 1.5–2 g 3 times a day or 1–1.5 g four times a day. The duration of treatment is also determined by the severity of the disease. When carrying Salmonella, amoxin is taken for up to 1 month.
To prevent endocarditis, it is necessary to take 3 g of amoxicillin in adults (1.5 g in children) 1 hour before medical manipulation or surgery and 8 hours after major surgical interventions.
Release form: capsules of 250 or 500 mg - 20 pieces per package; tablets of 500 mg or 1 g - 10 and 24 pieces per package, granulate for preparing a suspension in a bottle (250 mg or 500 mg in 5 ml of suspension).
Special instructions: amoxicillin is prescribed with caution to patients with colitis suffered while taking antibiotics, with insufficient renal function (for glomerulonephritis, diabetes mellitus, reduce the dose of the drug and reduce the frequency of administration), as well as during pregnancy and breastfeeding.
With simultaneous treatment with amoxin and aminoglycoside antibiotics, the effect of both drugs is reduced. Parallel intake of vitamin C increases the absorption of the drug. When prescribing treatment for patients taking oral contraceptives, it should be remembered that the latter become less effective when using amoxin.
Ospen
Active ingredient: phenoxymethylpenicillin.
Pharmacological action: a broad-spectrum antibiotic from the penicillin group that destroys bacteria by preventing the formation of components of their cell wall. Effective against infections caused by staphylococci and streptococci, microorganisms of the genus Neisseria (gonococcus, meningococcus). Does not affect microbes capable of producing penicillinase.
Indications: treatment and prevention of minor infections. Effective for diseases of the upper and lower respiratory tract (pharyngitis, bronchitis, pneumonia), diseases of the ENT organs (inflammation of the middle ear, sinuses, tonsillitis), skin and soft tissues (pustular infections, erysipelas).
It is used as a prophylactic agent in case of danger of complications of streptococcal infections: repeated rheumatic fever, endocarditis, nephritis.
Contraindications: allergies, severe bacterial infections.
Side effects: As a rule, they rarely develop. Mild stool disorders, allergies, transient pain in joints and muscles, and changes in the blood are possible.
Directions for use: inside, regardless of food intake, take a sufficient amount of water.
For children with infections, the dose is prescribed at the rate of 30-60 mg per 1 kg of body weight per day (dose frequency 3-4 times), for adults 500 mg - 1.5 g per day, also 3-4 times a day. The course of treatment is 7-10 days.
To prevent recurrent rheumatic fever, smallpox is prescribed 500 mg 2 times a day, to prevent endocarditis - 1 g for children, 2 g for adults before surgery (tooth extraction, insertion of an intravenous catheter, etc.) and 250 mg every 6 days. hourly intervals over the next two days.
Release form: tablets of 250 mg and film-coated tablets of 500 mg, 1 or 1.5 g - 12 pieces per package; granulate for preparing a suspension in a bottle (250 mg in 5 ml of suspension), syrup in a 60 ml bottle (250 mg in 5 ml).
Special instructions: in isolated cases, while taking smallpox, a false increase in glucose levels in the urine is possible; the analysis must be repeated after completion of the course of treatment.
Augmentin
Active ingredient: amoxicillin and clavulanic acid.
Pharmacological action: amoxicillin has an effect on many pathogens, which does not apply to microbes that secrete the enzyme penicillinase, which can destroy the drug. Clavulanic acid contained in Augmentin prevents the destructive action of penicillinase, as a result of which this complex drug acts on a greater number of pathogens than amoxicillin. Augmentin is active against chlamydia, treponema, enterococci, listeria, streptococci, staphylococci, clostridia, E. coli, Helicobacter, Vibrio cholerae, etc.
Indications: infections of the upper and lower respiratory tract (pharyngitis, tonsillitis, bronchitis, pneumonia), sore throat, inflammation of the sinuses and middle ear, kidneys and urinary tract (pyelonephritis, including urolithiasis, cystitis), dental infectious diseases, soft tissue infections and bones (phlegmon, pyoderma, erysipelas, osteomyelitis, bursitis, bite wounds), blood poisoning, urological and gynecological infections. The drug can be used to prevent purulent complications during various operations and other medical interventions, as well as to get rid of Helicobacter in gastritis and peptic ulcers of the stomach and duodenum.
Contraindications: individual intolerance to the drug, liver dysfunction in the past associated with the use of penicillins.
Side effects: allergies, candidiasis, decrease in the number of leukocytes, red blood cells and platelets in the blood, headache, stool disorders, nausea, colitis, abdominal pain, increased activity of liver enzymes in the blood, jaundice, nephritis.
Directions for use: The tablet form of the drug is best taken at the beginning of a meal. 625 mg of the drug is indicated for mild infections 2 times a day. Moderate and severe diseases require taking 1 g of medication up to 3 times a day. The course of treatment is 5-14 days.
For a number of diseases (severe pneumonia, peritonitis, phlegmon, sepsis), augmentin is first prescribed in the form of intravenous injections, and then, when the patient’s condition has stabilized, they switch to tablets.
The suspension is taken orally: 25 mg of amoxicillin and 3.6 mg of clavulanic acid per 1 kg of body weight per day for mild infections; 45 mg of amoxicillin and 6.4 mg of clavulanic acid per 1 kg of body weight in more serious cases. It is also used in the treatment of infectious diseases in children.
To prepare an injection solution, 600 mg of powder is diluted in 10 ml of water for injection, a dose of 1.2 g in 20 ml of solvent is administered intravenously by stream or drip (in the latter case, it is administered in 100 ml of 0.9% sodium chloride solution). Frequency of application 2-3 times a day.
Release form: tablets of 625 mg (500 mg amoxicillin and 125 mg clavulanic acid) - 20 pieces per package and 1 g (875 mg amoxicillin and 125 mg clavulanic acid) - 14 pieces per package; powder for preparing a suspension in a bottle (228.5 mg in 5 ml of suspension); powder for the preparation of an injection solution of 600 mg (500 mg amoxicillin and 100 mg clavulanic acid) and 1.2 g (1 g amoxicillin mg and 200 mg clavulanic acid) in a bottle.
Special instructions: in case of renal failure, the dose and frequency of administration of the drug is reduced. For hepatitis, liver cirrhosis, liver failure of various origins, treatment is carried out under the control of liver functions (determining the level of liver enzymes in the blood). Augmentin in high dosages (1 g or more) should not be prescribed to children under 12 years of age. It is used with caution during pregnancy and breastfeeding.
Cephalosporins
Cephalothin
Active ingredient: cephalothin.
Pharmacological action: 1st generation cephalosporin. Bactericidal - against gram-positive and gram-negative microorganisms, as well as leptospira and spirochetes.
Indications: infections of the respiratory tract, skin, bones, joints, endocarditis, peritonitis.
Contraindications: hypersensitivity to the drug, renal failure, pregnancy, breastfeeding.
Side effects: allergic reactions, nausea, vomiting, renal dysfunction.
Directions for use: intramuscularly or intravenously, 0.5–2 g 4 times a day. The maximum dose is 12 g per day. Children – 20–40 mg/kg body weight per day.
Release form: powder for preparing an injection solution - in bottles of 0.5 and 1 g.
Orizolin
Active ingredient: Cefazolin.
Pharmacological action: The antibiotic prevents the formation of bacterial cell wall components, causing their destruction and death. Effective against a wide range of pathogens: streptococci, staphylococci, gonococcus, meningococcus, treponema, E. coli, etc.
Indications: sinusitis, infectious diseases of the respiratory tract (pharyngitis, bronchitis, pneumonia, etc.), kidneys and urinary tract (cystitis, pyelonephritis), gall bladder (cholecystitis, cholangitis), soft tissues and bones (phlegmons, abscesses, osteomyelitis, mastitis) , gynecological and urological infections (gonorrhea, inflammation of the uterine appendages, syphilis). The drug can be used for severe infections: bacterial blood poisoning, bacterial endocarditis, peritonitis, as well as for the prevention of purulent complications after surgical interventions.
Contraindications: allergies, age up to 1 month.
Side effects: allergies of varying severity, fever, muscle and joint pain, headache, epileptiform reactions (convulsions), nausea, diarrhea, jaundice. Drug-induced hepatitis and suppression of hematopoiesis rarely develop. With prolonged courses of treatment, disorders may occur in the composition of the intestinal and vaginal microflora in women, and infection with microbes resistant to cefazolin (superinfection) is likely.
Directions for use: intramuscularly and intravenously, including drips. Depending on the severity of the infection, the drug is prescribed in a daily dose of 1 to 4 g, the frequency of administration is 3-4 times a day at regular intervals. The highest permissible dose is 6 g of orizolin per day. The course of treatment is 7-14 days.
If the drug is used as a prophylactic agent, it is administered in an amount of 1 g intravenously before surgery and 500 mg - 1 g after it every 8 hours for 24 hours.
Release form: powder for the preparation of injection solution, 125 mg, 500 mg and 1 g in a bottle.
Special instructions: the drug is prescribed with caution for severe kidney disease with insufficient kidney function. Patients who previously developed colitis while taking antibiotics require observation. When the drug is injected into a muscle, pain may occur for a long time; If administered intravenously too quickly, inflammation of the vein is possible - phlebitis.
Treatment with orizolin should not be carried out in parallel with taking certain diuretics (furosemide) and anticoagulants. When orizolin is administered in the same syringe with an aminoglycoside antibiotic, both drugs cease to be active.
Ceftriaxone
Active ingredient: ceftriaxone.
Pharmacological action: disrupts the formation of the bacterial shell, which contributes to its destruction and death of microbes. It acts against many pathogens, including activity against bacteria that are capable of producing β-lactamase. Can be used to combat E. coli, Klebsiella, gonococci, Proteus, Salmonella, etc.
Indications: infections of the upper and lower respiratory tract (pharyngitis, bronchitis, pneumonia, etc.), ENT organs (sinusitis, sinusitis), kidneys and bladder (pyelonephritis, cystitis), genital area, meninges, soft tissues, joints and bones (osteomyelitis, purulent processes). Prevention of postoperative complications, surgical diseases (peritonitis, cholecystitis), intestinal infections, extensive wounds, including burns and bites, treatment of sepsis.
Contraindications: allergies, including to other cephalosporins, penicillin antibiotics and carbapenems.
Side effects: allergies, nausea, stool disorders, abdominal pain, inflammation of the oral mucosa, jaundice, disturbances in the composition of the intestinal microflora, inhibition of blood cell formation, deterioration of blood clotting, changes in urine (appearance of casts, glucose), headache, candidiasis. There may be irritation and soreness in the injection area.
Directions for use: The powder is dissolved in water for injection, and the resulting solution is injected into a muscle or vein. For patients over 12 years of age, the dosage is on average 1–2 g per day, the drug is administered once a day. For severe infectious diseases, the amount of drug administered can reach 4 g per day.
For children from 2 weeks to 12 years of age, the dose of the drug is calculated by weight - from 20 to 80 mg per 1 kg of body weight per day, and if the amount of the drug is more than 50 mg per 1 kg of body weight, then it must be administered slowly, t That is, it is preferable to administer intravenous drips. Children under 2 weeks of age are administered no more than 20–50 mg of the drug per 1 kg of body weight per day. The course of treatment averages from 7 to 14 days.
In children under 5 years of age, with inflammation of the meninges, ceftriaxone is prescribed at a dose of 100 mg per 1 kg of body weight per day. The maximum permissible dose is 4 g per day. If the infection is caused by meningococcus, the course of treatment is 4 days, for pneumococcus - a week.
Gonococcal infection is treated with intramuscular administration of the drug - 250 mg of ceftriaxone once. If the medicine is used to prevent postoperative purulent complications, then it is administered 1–2 g once 30–90 minutes before surgery.
For intramuscular injection, the drug is dissolved in 3.6 ml of water for injection, for intravenous administration - in 10 ml of solvent. If the medicine is injected into a muscle, the solution can be mixed with lidocaine to reduce soreness. To prevent venous irritation, intravenous administration of the drug is carried out slowly, over 2–3 minutes. If ceftriaxone is planned to be administered by drip, the solution is prepared in 50 ml of 0.9% sodium chloride solution.
Release form: powder for preparing an injection solution - 1 g per bottle.
Special instructions: renal failure in the patient requires a reduction in the dose of ceftriaxone. If the medicine is used in parallel with drugs that reduce blood clotting (acetylsalicylic acid, clopidogrel, warfarin), it is necessary to anticipate an increased risk of bleeding. Treatment with ceftriaxone is not recommended with the simultaneous use of certain diuretics (furosemide), since the removal of the antibiotic from the body is impaired. During the treatment period, alcohol consumption is prohibited. Use with caution during pregnancy and breastfeeding.
Carbapenems
Meronem
Active ingredient: meropenem.
Pharmacological action: bactericidal - against gram-positive and gram-negative microorganisms - both aerobic and anaerobic.
Indications: pneumonia, including nosocomial infections, infectious diseases of the urinary system, skin, female genital organs, peritonitis. Used for septicemia and meningitis.
Contraindications:
Side effects: digestive disorders, changes in the cellular composition of the blood, skin allergic reactions, headache, increased levels of liver enzymes in the blood, pain at the injection site.
Directions for use: intravenously. For adults - 500 mg every 8 hours, for severe infections - 1 g every 8 hours. For meningitis - 2 g every 8 hours. For children, the drug is prescribed at 10-20 mg/kg body weight every 8 hours. For meningitis, the daily dose is increased up to 40 mg/kg body weight.
Release form: powder for the preparation of solution for injection in a bottle of 500 mg - 1 g.
Special instructions: There are no data on the safety of the drug during pregnancy.
Aminoglycosides
Amikacin
Active ingredient: amikacin.
Pharmacological action: bacteriostatic semi-synthetic antibacterial drug with a broad spectrum of action.
Indications: infections of the respiratory system, skin, genitourinary system, gastrointestinal tract, burns, endocarditis, osteomyelitis, peritonitis, meningitis.
Contraindications: hypersensitivity to the drug, decompensated renal failure accompanied by uremia, liver dysfunction, auditory neuritis, pregnancy.
Side effects: damage to the organ of hearing and kidneys.
Directions for use: intravenously, intramuscularly. The dosage is set individually, taking into account the form of the disease, the severity of the clinical picture, as well as the sensitivity of the microflora to the drug.
Dose for adults and adolescents – 5 mg/kg body weight 3 times a day or 7.5 mg/kg body weight 2 times a day. The usual dose for children is 10 mg per 1 kg of body weight for 2-3 administrations. For kidney diseases, the dose is selected strictly taking into account laboratory parameters. The course of treatment is 7-10 days.
Release form: solution for injection in 2 ml ampoules containing 100, 500 mg of the drug, in a package - 5 ampoules.
Special instructions: cannot be used simultaneously with heparin, erythromycin, amphotericin B, vitamins B and C, polymyxin B, vancomycin, diuretics, non-steroidal anti-inflammatory drugs, sulfonamides, polymyxins, opioid analgesics.
Tobramycin
Active ingredient: tobramycin sulfate.
Pharmacological action: has a detrimental effect on a wide range of pathogens and is effective against many intestinal and pyogenic bacteria, staphylococci.
Indications: lower respiratory tract infections (bronchitis, including exacerbation of chronic obstructive pulmonary disease, pneumonia), infected wounds of any origin, osteomyelitis, phlegmon, pyoderma, arthritis. The drug is active in diseases of the kidneys (pyelonephritis), reproductive system organs (prostatitis, inflammation of the ovaries, etc.), surgical infections (peritonitis). Tobramycin is used in the treatment of bacterial blood poisoning, inflammation of the meninges, and bacterial endocarditis.
Contraindications: individual intolerance to the drug, pregnancy and breastfeeding.
Side effects: allergies, headache, unmotivated increase in body temperature, suppression of hematopoiesis, hearing loss, weakness, changes in urine (appearance of protein and a small number of red blood cells), decrease in blood levels of calcium, potassium, magnesium and sodium with corresponding symptoms. Most often, undesirable effects develop when taking high doses of the drug and long courses of treatment.
Directions for use: intramuscularly or intravenously (drip). A solution for intramuscular administration is prepared in 5 ml of water for injection; for intravenous administration, the drug is diluted in 100–200 ml of 0.9% sodium chloride solution or 5% glucose solution.
The dose of the drug is calculated based on the patient’s weight and divided into 3 doses. The amount of drug administered differs depending on the severity of the disease. Mild and moderately severe infections require the use of 2–3 mg of tobramycin per 1 kg of body weight per day; for severe diseases, 4–5 mg of the drug per 1 kg of body weight per day is required. For infants, the dose of the drug should not exceed 3 mg per 1 kg of body weight per day.
The course of treatment averages 7-14 days, depending on the severity of the disease. In especially severe cases (sepsis, endocarditis), treatment can be continued for up to 1.5 months.
Release form: solution for intramuscular and intravenous administration - 1 and 2 ml (1 ml contains 10 or 40 mg) in ampoules, 10 pieces per package.
Special instructions: the drug is prescribed with caution to patients with renal failure and premature infants (in the latter, due to immature kidneys, the removal of the antibiotic from the body may slow down).
Treatment with tobramycin is carried out under the supervision of a physician with monitoring of the patient’s hearing (especially important in children), since antibiotics of its group can have an adverse effect on the auditory nerve. Most often, hearing disorders are observed during simultaneous treatment with diuretics: furosemide, ethacrynic acid.
Gentamicin
Active ingredient: gentamicin sulfate.
Pharmacological action: has the ability to influence protein metabolism processes in a bacterial cell, slows down the formation of structural components of microorganisms, which causes their death. The spectrum of activity is similar to that of tobramycin.
Indications: mainly for the treatment of severe infectious diseases. The drug is toxic, but in conditions where other antibiotics are not effective enough, its use is justified.
Prescribed for bacterial infection of the blood, including intrauterine infection of the fetus, extensive burn wounds, large phlegmons, osteomyelitis, extensive pneumonia, inflammation of the meninges.
Gentamicin can also be used for complicated diseases of the kidneys and urinary tract, for infections in patients with reduced immunity (suffering from HIV infection, diabetes mellitus, receiving treatment with hormones and antitumor drugs).
Contraindications: allergies, pregnancy.
Side effects: deterioration of hearing and kidney function, pain in the liver and an increase in the level of liver enzymes in the blood, changes in urine (the appearance of protein, single red blood cells), a decrease in the volume of urine excreted, inhibition of hematopoiesis, increased body temperature, allergies, sleep disorders, nausea.
Directions for use: as a solution for intramuscular and intravenous injections; sometimes the drug is instilled into the eyes.
The average dose of the drug for adult patients and children over 2 years of age is 3 mg per 1 kg of body weight per day (the indicated amount is divided by two and administered in the morning and evening), in particularly serious cases up to 5 mg per 1 kg of body weight is required. daily, dosage frequency 3–4 times. When treating complicated infectious diseases of the kidneys and bladder, 120–160 mg of the drug is used once a day. The course of treatment is on average 7-14 days.
For children under 2 years of age, the daily dose is determined at the rate of 6 mg per 1 kg of body weight, the drug is administered 2-3 times a day.
For infectious eye diseases, the drug is administered 1-2 drops every 1-4 hours.
Release form: solution of 40 and 80 mg in ampoules - 10 pieces per package; eye drops in a 5 ml dropper bottle (1 ml contains 3 mg).
Special instructions: use the drug with caution in patients with renal failure and hearing impairment; appropriate monitoring is required during treatment. Careful monitoring during the period of use of gentamicin is also necessary for people over 60 years of age and patients suffering from water-electrolyte imbalances and myasthenia.
Tetracycline group drugs
Doxycycline
Active ingredient: doxycycline hydrochloride.
Pharmacological action: semi-synthetic antibacterial drug with a broad spectrum of action. Bacteriostatically affects aerobic gram-positive and gram-negative microorganisms.
Indications: inflammatory infectious diseases of the respiratory system, digestive system, skin and soft tissues, ear. Used for infectious diseases, sexually transmitted diseases, osteomyelitis, trachoma.
Contraindications: hypersensitivity to tetracycline drugs, myasthenia gravis (for intravenous administration), children under 8 years of age, periods of pregnancy and lactation.
Side effects: dysfunctions of the digestive organs, various allergic manifestations, dysbacteriosis, hemolytic anemia.
Directions for use: orally or intravenously 1–2 times a day. Adults – 200 mg on the first day, then 100–200 mg per day. Children over 8 years old weighing more than 50 kg - 2-4 mg/kg body weight per day.
Release form: 100 mg capsules – 8 pieces per package; lyophilisate (100 mg) for the preparation of injection solution in 5 ml bottles.
Special instructions: solution for intravenous administration can be stored for up to 72 hours in the refrigerator.
Macrolides
Clarithromycin
Active ingredient: clarithromycin.
Pharmacological action: inhibits the proliferation of gram-positive and gram-negative bacteria - both aerobic and anaerobic.
Indications: infectious diseases caused by microbes sensitive to clarithromycin, inflammation of the sinuses, pharyngitis, sore throat, erysipelas and other skin infections, bronchitis, pneumonia.
Contraindications: childhood, intolerance to the drug components, pregnancy.
Side effects: nausea, vomiting, abdominal pain, taste disturbance, diarrhea, headache, allergies - most often in the form of skin rashes; sleep disturbances and tinnitus are possible; very rarely - disorders of consciousness, decreased ability to concentrate, hallucinations; infrequently – heart rhythm disturbances, increased heart rate.
Directions for use: tablets orally, regardless of meals, 250 mg 2 times a day at approximately equal intervals. Children under 12 years of age – 7.5 mg/kg body weight per day, but not more than 500 mg. Treatment lasts 7-10 days.
Release form: coated tablets of 250, 500 mg - 10 pieces per package; capsules of 250, 500 mg - 10 pieces per package.
Special instructions: The use of the drug is limited to people over 60 years of age, with severe liver and kidney diseases, and fungal infections.
Spiramycin
Active ingredient: spiramycin.
Pharmacological action: bacteriostatic – for streptococci, corynebacteria, mycoplasma, chlamydia, treponema, toxoplasma, clostridia.
Indications: diseases caused by microbes sensitive to spiramycin - diseases of the ear, throat, nose and respiratory tract (otitis media, sinusitis, bronchitis, tracheitis); atypical pneumonia, periodontitis, infections of the skin, genitourinary system - except those of gonorrheal origin. Spiramycin is a means of preventing meningitis caused by meningococcus, as well as recurrent rheumatic fever.
Contraindications: individual intolerance to the drug, some types of enzyme deficiency (possible destruction of red blood cells), liver diseases (bile stones, severe hepatitis, cirrhosis), pregnancy (some restrictions), breastfeeding.
Side effects: nausea, vomiting, diarrhea, occasionally - severe colitis, changes in sensitivity (a feeling of “crawling goosebumps”, numbness), liver dysfunction, possible destruction of red blood cells and a decrease in the level of platelets in the blood, with a certain predisposition can provoke blockades of the conduction system of the heart, allergic reactions in in the form of skin rashes.
Directions for use: tablets inside. Adults – 2,000,000-3,000,000 IU per day for 2 doses. The maximum daily dose is 4,000,000-5,000,000 IU per day. Children – 50-100 IU/kg body weight per day for 2 doses. The solution is administered intravenously to adults and adolescents in a dose of 500,000 IU to 1,000,000 IU 3 times a day.
Release form: coated tablets 1,500,000, 3,000,000 IU, powder in bottles (1,500,000 IU).
Sumamed
Active ingredient: azithromycin.
Pharmacological action: bactericidal drug of the macrolide group with a broad spectrum of action.
Indications: diseases whose pathogens are sensitive to the drug (skin infections, scarlet fever, atypical pneumonia, gonorrhea, chlamydia, otitis, acute respiratory viral infections complicated by bacterial infection), as well as gastric ulcer (to combat Helicobacter pylori).
Contraindications: drug intolerance, liver and kidney diseases with decreased function, pregnancy, breastfeeding.
Side effects: nausea, vomiting, diarrhea, increased gas formation in the intestines, jaundice with obstruction of the biliary tract, discomfort in the chest and abdomen, lethargy, possible changes in the number of blood leukocytes, increased sensitivity to sunlight, colitis.
Directions for use: orally 1 time per day isolated from food (one hour before or 2 hours after). On the first day, 2 capsules are prescribed, and then one at a time. Children – 5-10 mg/kg body weight per day once. The course of treatment is 5–7 days. A possible dosage regimen is 2 capsules per day for 3 days.
Release form: capsules and tablets of 250 mg - 6 pieces per package, 500 mg - 3 pieces per package.
Erythromycin
Active ingredient: erythromycin.
Pharmacological action: affects biochemical processes and prevents the proliferation of microorganisms, disrupts the metabolism in the bacterial cell. Active against staphylococci, streptococci, clostrilia, diphtheria bacillus, gonococci, meningococci, whooping cough pathogen, spirochetes. Ineffective against intestinal infections.
Indications: in tablet form, the drug can be used to treat childhood infections (whooping cough), respiratory diseases (pharyngitis, pneumonia), diphtheria, inflammation of the tonsils, middle ear, sinuses, exacerbations of chronic cholecystitis. Used in the fight against sexually transmitted diseases (syphilis, gonococcal infection), during purulent processes (phlegmon, abscesses, burns, bite wounds, etc.).
In the form of an ointment, erythromycin is used to treat pyoderma and other external infectious processes. A specially developed eye ointment is suitable for the treatment of inflammatory diseases of the hair follicles of the eyelashes, conjunctiva and cornea of the eye, as well as trachoma (caused by chlamydia).
Contraindications: allergies, liver dysfunction due to taking antibiotics in the past, severe kidney disease with insufficient kidney function.
Side effects: allergies, nausea, abdominal discomfort, pain in the liver, very rarely drug-induced hepatitis. In addition, when used externally, redness of the skin, formation of scales, and discomfort at the site of application of the ointment are possible. When using eye ointment, there may be lacrimation, redness of the conjunctiva, transient photophobia and blurred vision immediately after its application.
Directions for use: The tablets are taken orally with water, an hour before or 2 hours after a meal. Depending on the severity of the infection, take 250–500 mg of the drug 4–6 times a day (at regular intervals). The maximum permissible single dose is 500 mg; it is not recommended to take more than 4 g per day.
For children under 3 months of age, the dose of the drug is from 20 to 40 mg per 1 kg of body weight per day in several doses (every 4-6 hours). Patients aged 4 months to 18 years are given 30–50 mg of the drug per 1 kg of body weight per day. Treatment lasts from 7 to 14 days.
Erythromycin in ointment form is applied to the skin 2-3 times a day. Burn wounds are treated every other day. For external use, the antibiotic is prescribed for long courses until signs of infection completely disappear. Eye ointment is placed behind the eyelid 2-3 times a day, treatment lasts from 2 to 8 weeks, for trachoma - 4 months.
Release form: coated tablets of 100, 250 and 500 mg - 16 pieces per package; ointment in tubes of 10, 15 and 30 g (1 g contains 10,000 units of erythromycin); eye ointment in tubes of 7, 10 and 15 g (1 g contains 10,000 units of erythromycin).
Special instructions: erythromycin can be used as an alternative to penicillin antibiotics if the patient has developed an allergy to the latter. It is prescribed with great caution during pregnancy and breastfeeding. With parallel treatment with diuretics, the elimination of erythromycin from the body slows down, which can increase its toxic effect on the liver and kidneys. The simultaneous use of this antibiotic with anticoagulants causes a slowdown in blood clotting. The drug can reduce the effectiveness of oral contraceptives, so during the treatment period you should resort to additional methods of contraception.
Drugs of the chloramphenicol group
Chloramphenicol
Active ingredient: chloramphenicol.
Pharmacological action: bacteriostatic antibiotic. It affects gram-positive and gram-negative microorganisms; resistance to it develops slowly.
Indications: salmonellosis, typhoid fever, dysentery; brucellosis, paratyphoid fever, meningitis, tularemia, chlamydia, gonorrhea, pneumonia, whooping cough and other infectious diseases.
Contraindications: hypersensitivity to the drug, eczema, psoriasis, fungal skin infections, periods of pregnancy and lactation, newborns, inhibition of hematopoiesis.
Side effects: skin rash, irritation of the mucous membrane of the mouth and pharynx, diarrhea, changes in the cellular composition of the blood, disturbances of consciousness, auditory and visual hallucinations, decreased visual and hearing acuity.
Directions for use: orally 30 minutes before meals. Daily doses: adults – 250–500 mg (maximum daily dose – 4 g), children under 3 years old – 10–15 mg/kg body weight, children 3–8 years old – 150–200 mg, children over 8 years old – 200–300 mg. Frequency of administration – 3–4 times a day. The course of treatment is 2 weeks.
Release form: in the form of tablets of 250 and 500 mg - 10 pieces per package.
Special instructions: the drug is incompatible with barbiturates, sulfonamides, and cytostatics.
Lincosamides
Clindamycin
Active ingredient: clindamycin.
Pharmacological action: bacteriostatic antibiotic of the lincosamide group. Affects anaerobic and aerobic gram-positive microorganisms, anaerobic gram-negative microorganisms. Microflora resistance to the drug develops slowly.
Indications: erysipelas, scarlet fever, sepsis, otitis, bacterial endocarditis, tonsillitis, aspiration pneumonia, inflammation of the sinuses, ulcers of various locations, infectious lesions of bones and joints, inflammation of the uterine appendages, colpitis, wound infection, etc.
Contraindications: individual intolerance to the drug, myasthenia gravis.
Side effects: abdominal pain, nausea, decreased number of leukocytes in the blood, colitis, skin rashes; If the drug is injected too quickly into a vein, a sharp drop in blood pressure may occur.
Directions for use: orally, intramuscularly and intravenously. In tablets – 150–450 mg 3–4 times a day. For children, the dosage is calculated based on the norm of 8-25 mg per 1 kg of body weight per day. For injection into muscle and vein, adults – 1.2–2.7 g per day, children up to 1 month – 15–20 mg/kg body weight per day, children over 1 month – 20–40 mg/kg body weight per day. The frequency of administration is 3–4 times a day.
Release form: solution for injection in ampoules of 4 ml (150 mg in 1 ml) - 5 ampoules per package; capsules of 150 mg, 300 mg - 8 pieces per package; vaginal cream in a 100 g tube.
Special instructions: The use of the drug is limited in pregnant and lactating women, as well as in patients with renal and liver failure, and young children.
Quinolones
Palin
Active ingredient: pipemidic acid.
Pharmacological action: affects metabolic processes, helping to destroy bacteria. Effective in the fight against Escherichia coli, gonococci, meningococci, Pseudomonas aeruginosa, and staphylococci.
Indications: kidney and urinary tract infections (inflammation of the renal pelvis, bladder, urethra, including gonorrhea), prostatitis.
Contraindications: the drug should not be used for diseases accompanied by seizures, renal and liver failure, individual intolerance, during pregnancy and breastfeeding, in patients under 14 years of age.
Side effects: nausea, vomiting, stool disorders, abdominal pain, disorders of the intestinal microflora, allergies, changes in behavior, seizures, insomnia, changes in skin sensitivity, suppression of hematopoiesis. Since palin acts on a limited range of microbes, the development of superinfection is possible - infection with bacteria resistant to quinolones.
Directions for use: orally, before meals, with water. The average dosage of the drug is 200 mg 2 times a day. If the disease is caused by one of the varieties of staphylococcus, the frequency of taking the drug should be increased to 3 times a day. The course of treatment is from 7 to 10 days, however, for severe pyelonephritis, taking palin can last up to 1.5 months, and for prostatitis - up to 2 months. For uncomplicated cystitis in women, the drug is used in the form of suppositories, 1 piece before bedtime.
Release form: capsules 200 mg - 20 pieces per package, coated tablets 400 mg - 20 pieces per package, vaginal suppositories 200 mg - 10 pieces per package.
Special instructions: if the patient has previously suffered a stroke, therapy should be carried out under the supervision of a physician. When taking palin, you need to drink more fluid. During the treatment period, a false increase in glucose levels in the urine is possible.
Fluoroquinolones
Norfloxacin
Active ingredient: norfloxacin.
Pharmacological action: a synthetic drug from the fluoroquinolone group that has a broad-spectrum bactericidal effect.
Indications: acute as well as chronic infectious diseases of the urinary tract, prevention of relapses of infectious diseases of the urinary tract, gonorrhea, bacterial gastroenteritis, prevention of diarrhea during travel.
Contraindications: childhood and adolescence, high sensitivity to the active substance of the drug, periods of pregnancy and lactation.
Side effects: allergic reactions, disorders of the stomach and intestines, dizziness, headache; in old age - drowsiness, fatigue, weakness, irritability, anxiety, confusion, hallucinations, fear, tinnitus, depression.
Directions for use: orally 1 hour before or 2 hours after meals, washed down with water, 1 tablet 2 times a day. The course of treatment is 1–2 weeks.
For acute uncomplicated cystitis - 1 tablet 2 times a day for 3-5 days. For gonorrhea - 1 time (0.8–1.2 g) or 2 times (0.4 g) per day for 3–7 days.
For chronic bacterial prostatitis - 1 tablet 2 times a day for 4-6 weeks.
To prevent diarrhea during travel, take 0.4 g 1 day before departure, and then during the entire trip - 1 tablet per day.
Release form: in the form of tablets of 0.4 g - 10 pieces per package.
Special instructions: Use cautiously in patients with kidney disease, central nervous system, and tendon inflammation. While taking the drug, you should avoid activities that require high concentration.
Ofloxacin
Active ingredient: ofloxacin.
Pharmacological action: a broad-spectrum drug with bactericidal properties.
Indications: urinary tract infections (urethritis, cystitis, prostatitis); gynecological infectious diseases (adnexitis, colpitis); respiratory tract infections (pneumonia, acute and chronic bronchitis); ENT infections (sinusitis, otitis media, pharyngitis, tonsillitis); infections of the skin and soft tissues (erysipelas, infected wounds); eye infections (keratitis, blepharitis); gastrointestinal tract infections (cholangitis, cholecystitis, intestinal infections); infections of the joints and bones (osteomyelitis).
Contraindications: childhood and adolescence, epilepsy, high sensitivity to the drug.
Side effects: nausea, vomiting, abdominal pain, diarrhea, headache, dizziness, weakness, insomnia, rash, itching, swelling, fever.
Directions for use: the dosage is selected individually by the doctor. Usually 1-2 tablets orally 2 times a day. For uncomplicated urinary tract infections - 1 tablet 2 times a day. In case of severe infections and the inability to take it orally, an intravenous infusion of the solution is prescribed, 1-2 bottles 2 times a day by drip. If kidney function is impaired, on the first day - 1 bottle, then 0.5 bottles per day.
Release form: tablets of 200 mg - 10 and 20 pieces per package; solution for infusion, 100 ml in a bottle (1 ml - 2 mg).
Special instructions: treatment with the drug cannot be combined with ultraviolet irradiation.
Sparflo
Active ingredient: sparfloxacin.
Pharmacological action: has an adverse effect on the genetic apparatus of the bacterial cell and destroys its membranes, resulting in its death. Fights a large number of pathogens: intestinal bacteria, Pseudomonas aeruginosa, chlamydia, streptococci, mycoplasma, ureaplasma, etc.
Indications: respiratory diseases (bronchitis, hospital-acquired pneumonia), sinusitis, otitis, infectious conjunctivitis, keratitis, pyelonephritis, cystitis, prostatitis, inflammation of the uterine appendages, wound infection, blood poisoning, chlamydial infection, intestinal infections, pulmonary tuberculosis.
Contraindications: allergies, diseases of the central nervous system accompanied by seizures, age under 18 years, heart rhythm and conduction disorders, pregnancy and breastfeeding. In addition, the drug is not recommended for use in cases of kidney disease with insufficient kidney function.
Side effects: nausea, stool disorders, increased gas formation in the intestines, headache, sleep disorders, changes in skin sensitivity. Sometimes there is increased sweating, changes in behavior, development of heart rhythm disturbances associated with slower conduction in the ventricles, inhibition of hematopoiesis, and loss of consciousness. Possible increased body temperature, allergic reactions, increased bleeding, pain in muscles and joints, increased sensitivity to ultraviolet rays.
Directions for use: orally, the dose of the drug can range from 100 to 400 mg per day, depending on the location and severity of the infectious process. For respiratory infections, the first dose is 400 mg, then 200 mg is prescribed 1 time per day for 10–14 days. For pyelonephritis, cystitis, the drug is taken first in an amount of 200 mg, and then until the end of treatment - 100 mg 1 time per day. For gonorrhea, you need to take 200 mg of Sparflo once.
Release form: film-coated tablets, 200 mg - 6 pieces per package.
Special instructions: During treatment with Sparflo, you should try to avoid prolonged exposure to the sun and drink more fluids. The drug may cause drowsiness, which is why, while taking it, you should avoid doing work that requires increased attention and quick reaction. Concomitant use of iron supplements slows down the absorption of the antibiotic.
Sulfonamides
Lidaprim
Active ingredient: sulfametrol, trimethoprim.
Pharmacological action: a combined broad-spectrum drug that has a bactericidal effect.
Indications: acute and chronic infectious diseases of the respiratory tract (pharyngitis, tonsillitis, otitis, pneumonia), urinary tract and kidneys (pyelitis, pyelonephritis, urethritis, cystitis), gastrointestinal tract (cholecystitis, cholititis, enteritis), genital organs, skin infections (abscesses) , boils, pyoderma), etc.
Contraindications: hypersensitivity to the drug, severe renal and liver dysfunction, heart failure, children under 6 weeks of age, periods of pregnancy and lactation.
Side effects: nausea, vomiting, loss of appetite, dry mouth, allergic reactions.
Directions for use: inside after meals. Children aged 6 weeks to 5 months - 2.5 ml of suspension 2 times a day, from 6 months to 5 years - 5 ml of suspension 2 times a day, from 6 to 12 years - 10 ml of suspension or 4 tablets 2 times a day, over 12 years of age and adults - 2 tablets 2 times a day. The course of treatment is 5 days or more.
Release form: tablets (80 mg trimethoprim and 400 mg sulfametrol) - 20 pieces per package; tablets for children (20 mg trimethoprim and 100 mg sulfametrol) - 20 pieces per package; children's suspension in bottles of 100 ml for oral administration (in 5 ml - 40 mg of trimethoprim and 200 mg of sulfametrol).
Special instructions: Use lidaprim cautiously in combination with drugs that lower blood sugar.
Glycopeptides
Vancomycin
Active ingredient: vancomycin.
Pharmacological action: bactericidal antibiotic of the glycopeptide group, affects gram-positive microorganisms.
Indications: sepsis, infective endocarditis, lung abscess, infectious skin diseases, meningitis.
Contraindications: hypersensitivity to the drug, damage to the auditory nerve, pregnancy.
Side effects: dizziness, nausea, allergic reactions, kidney damage, thrombophlebitis, fever.
Directions for use: intravenously or intramuscularly, 500 mg 4 times a day or 1000 mg 2 times a day. Children – 40 mg/kg body weight per day for 2 or 4 administrations. Duration of 1 intravenous injection is 60 minutes.
Release form: in the form of a powder for the preparation of an injection solution in bottles of 0.5, 1 g.
Special instructions: do not use together with aminoglycosides, loop diuretics, cyclosporine, general anesthetics.
Phosphonic acid derivatives
Fosfomycin
Active ingredient: fosfomycin trometamol.
Pharmacological action: a broad-spectrum antibacterial drug that has a bactericidal effect on most gram-positive bacteria.
Indications: acute and chronic cystitis, nonspecific bacterial urethritis, massive asymptomatic bacteriuria (in pregnant women), prevention of urinary system infections during surgical and diagnostic transurethral interventions, urinary system infections in the postoperative period.
Contraindications: children under 5 years of age, hypersensitivity to the components of the drug, severe renal failure.
Side effects: nausea, heartburn, diarrhea, allergic reactions.
Directions for use: Before use, dissolve the contents of 1 sachet in 0.3 glasses of water. Take orally 2 hours before meals 1 time per day, after emptying the bladder. Adults once – 3 g per day, children once – 2 g per day. For severe and recurrent infections, repeated use of the drug every other day in the same dosage is allowed.
Release form: in the form of granules for the preparation of a solution for oral administration in bags of 2 and 3 g.
Special instructions: during pregnancy, use taking into account the potential benefit to the mother and the possible risk to the fetus. During therapy you should stop breastfeeding.
Sulfadiazine
Active ingredient: silver sulfadiazine.
Pharmacological action: broad spectrum antimicrobial effect. Affects bacteria and some fungi.
Indications: infectious skin diseases, bedsores, deep wounds, burns.
Contraindications: hypersensitivity to the drug, pregnancy, age up to 1 month.
Side effects: local skin reactions - itching, burning. With long-term use of the drug, leukopenia may develop.
Directions for use: externally. A layer of cream is applied to the treated wound or affected skin and covered with a sterile dressing. Change the bandage 2 times a day. It is possible to use the drug for up to 3 weeks.
Release form: 1% cream in tubes of 50 g or jars of 250 g.
Antiviral drugs
Medicines in this group are used in the treatment of diseases caused by viruses. They are also prescribed for preventive purposes.
Antiviral drugs are divided into several groups: interferons and their analogues, interferonogens, derivatives of purine, pyrimidine, adamantane. There are also drugs that have an antiviral effect, created on the basis of plant materials.
Interferon group drugs are obtained from biological material using genetic engineering methods.
These include ophthalmoferon, human leukocyte interferon, herpferon, viferon.
Interferons are active in any acute respiratory viral infections. Their use from the onset of the disease (during the latent period) for 1-3 days helps to significantly alleviate further symptoms. Interferonogens enhance the human body’s production of its own interferon and are classified as immunomodulators (see Chapter 10). They are used for prophylactic purposes.
Antiviral drugs such as ribavirin, arbidol, remantadine, and Tamiflu are obtained chemically. The last drug is the most famous. It is currently less used because it is only active against influenza viruses. Many newer drugs are used for a larger number of diseases. Remantadine has a good effect as a prophylactic against influenza during the cold season.
Ribavirin is similar to rimantadine, but is also used for respiratory syncytial infection. This disease often occurs in the form of pneumonia in children under 1 year of age.
Arbidol is also effective only for influenza; it inhibits the proliferation of viruses in the body.
Tamiflu is also used to treat influenza. This is a more effective drug; it is prescribed both at the onset of the disease and as it develops. The drug significantly reduces the number of complications from influenza, but has many side effects. It is prescribed only to adults and children over 12 years of age.
Chemical antiviral drugs include oxolin, bonafton, florenal, tebrofen. Most of them are used topically for various viral diseases (herpes, adenovirus infection).
Acyclovir
Active ingredient: acyclovir
Pharmacological action: the drug belongs to the acyclic analogues of guanine. It is a natural component of deoxyribonucleic acid (DNA). Effective for diseases caused by herpes simplex viruses (types 1, 2), chickenpox viruses, Epstein-Barr, cytomegalovirus.
Indications: The drug is prescribed orally or intravenously for herpes, chicken pox, as well as for their prevention. In ophthalmic practice, the drug is used for herpetic keratitis. Locally, the drug is used in the treatment of herpes and chickenpox.
Contraindications: hypersensitivity to the drug, renal failure.
Side effects: When using the drug internally, dysfunction of the gastrointestinal tract and abdominal pain are observed. There may be dizziness and headache, increased body temperature. More rarely, hair loss and skin rashes, impaired renal and liver function are observed.
Intravenous administration of the drug can lead to damage to the central nervous system (convulsions, mental and consciousness disorders). Possible acute renal dysfunction.
Local use of the drug in ophthalmic practice can cause inflammation of the conjunctiva, eyelids, and cornea. When applied to the skin, there may be burning, redness and flaking of the skin, itching.
Directions for use: Orally prescribed for adults and children over 2 years old - 200-400 mg 3-5 times a day. In severe cases, you can increase the single dose to 800 mg and take it 4 times a day. For children under 2 years of age, the dose is reduced by 2 times. The duration of treatment is 5-10 days.
The drug is administered intravenously to adults and children over 12 years of age at a dose of 5-10 mg/kg body weight 3 times a day. The maximum daily dose for adults is 30 mg/kg body weight per day. For children from 3 months to 12 years, the drug is administered 3 times a day at a dose of 250–500 mg/m2 of body surface.
The drug is used externally and locally 5 times a day. The duration of treatment is determined individually.
Release form: tablets of 200, 400 mg - 20 pieces per package, 5% ointment - 5 g in a tube (50 mg in 1 g), 5% cream - 2, 5, 20 g in a tube (in 1 g 50 mg), powder for the preparation of injection solution - in a bottle of 250, 500 mg.
Special instructions: the drug is prescribed with caution for kidney disease and elderly people. During treatment it is necessary to drink more fluid. It is not advisable to prescribe the drug during pregnancy and breastfeeding. Cream and ointment are not used for application to the mucous membranes of the eyes, mouth, or vagina.
Valtrex
Active ingredient: valacyclovir.
Pharmacological action: inhibits the proliferation of herpes viruses. In the human body, the drug is converted into acyclovir and valine.
Indications: treatment and prevention of exacerbations of diseases caused by herpes simplex viruses, herpes zoster.
Contraindications: hypersensitivity to the drug and acyclovir.
Side effects: in rare cases, headache and nausea are observed. In severe immunodeficiency conditions, use of the drug in large doses and for a long time can cause impaired renal function and hemolytic anemia.
Directions for use: inside. For herpes zoster, the drug is prescribed 1 g 3 times a day for 7 days. In the case of herpes simplex, the drug is recommended to be taken 2 times a day, 500 mg. The duration of treatment is 5-10 days. If renal function is impaired, the dose of the drug is selected individually depending on creatinine clearance (1 g 1-2 times a day).
Release form: tablets of 500 mg - 10 or 42 pieces per package.
Special instructions: There is no information on the safety of treatment with the drug during pregnancy and breastfeeding. Elderly people are advised to drink more fluids during treatment. The drug is not prescribed for children.
Trizivir
Active ingredient: abacavir sulfate, lamivudine, zidovudine.
Pharmacological action: effectiveness against human immunodeficiency viruses (HIV) types 1 and 2. Reduced sensitivity to abacavir was detected in nosocomial HIV strains.
Indications: treatment of HIV infection.
Contraindications: hypersensitivity to the components of the drug, age under 12 years, significant impairment of liver function, decrease in hemoglobin level less than 75 g/l, number of neutrophils less than 0.75 × 10 /l in the blood, period of breastfeeding.
Side effects: damage to the heart muscle (cardiomyopathy), severe anemia, decreased number of leukocytes, including neutrophils, platelets in the blood. When treated with high doses of the drug, suppression of red bone marrow function is possible. There may be disturbances in the function of the stomach and intestines (lack of appetite, nausea, vomiting, pain in the upper abdomen, diarrhea, increased gas formation in the intestines). Pigment spots may appear on the oral mucosa. Dysfunction of the liver and pancreas is determined by an increase in the blood levels of bilirubin, aspartate aminotransferase, alanine aminotransferase, and lactic acid. Sometimes an increase in the size of the liver is detected. Pain in muscles and joints is possible. When treated with the drug, there may be mental and neurological disorders (sleep disorders, dizziness and headache, convulsions, slowing down of thinking processes, depression, sensitivity disorders). Respiratory side effects may include shortness of breath and cough. The skin may experience pigmentation, redness, toxic ulcerating blisters and other rashes, itching and increased sweating. More rarely, weakness, increased body temperature, chills, enlarged mammary glands in men, and taste perversions are observed.
Directions for use: inside, regardless of food intake. Adults and children over 12 years of age weighing more than 40 kg are prescribed 1 tablet 2 times a day. Tablets must not be broken!
If renal function decreases, the level of hemoglobin in the blood decreases to less than 90 g/l and the number of neutrophils less than 1000 per 1 μl, it is recommended to prescribe the components of the drug separately. If blood side effects occur, reduce the dose of zidovudine.
Release form: coated tablets (300 mg abacavir sulfate, 150 mg lamivudine, 300 mg zidovudine) – 60 pieces per bottle.
Special instructions: There are no data on the safety of using the drug during pregnancy. During the period of breastfeeding, the child is transferred to artificial or donor feeding. Pregnant women are prescribed the drug only in extreme cases, when the benefit to the mother is greater than the risk to the fetus. If there is a significant increase in the level of lactic acid in the body and signs of toxic damage to the liver, inflammation of the pancreas, the drug is discontinued. During the treatment process, the blood is tested 2 times a week for the first 3 months, then once a month.
Side effects may reduce your ability to drive and perform other activities requiring increased alertness. There is no information about the effect of the drug on the ability of women to conceive.
Viramune
Active ingredient: nevirapine anhydrate.
Pharmacological action: has an antiviral effect against HIV-1. The drug is quickly absorbed after internal use and excreted through the kidneys.
Indications: HIV-1 infection in adults and children. Prevention of infection of newborns in mothers who are carriers of HIV-1.
Contraindications: hypersensitivity to the drug.
Side effects: various skin rashes (reddened spots, bumps, diffuse redness) and itching. Allergic reactions may include muscle and joint pain, fever, swollen lymph nodes, hepatitis, and an increase in the number of eosinophils in the blood. In rare cases, allergies are accompanied by impaired renal function, the development of Quincke's edema, and toxic blistering skin lesions. Possible dysfunction of the stomach and intestines, increased blood levels of enzymes (?-glutamyl transpeptidase, alkaline phosphatase, alanine aminotransferase, aspartate aminotransferase), hepatitis, abdominal pain. A decrease in the number of granulocytes in the blood is observed mainly in children. Possible disturbances in the activity of the central nervous system (headache, increased fatigue, drowsiness).
Directions for use: inside. For adults, the drug is prescribed 200 mg once a day for 2 weeks. Then the drug is taken in the same dose 2 times a day. For children from 2 months to 8 years, the drug is prescribed 4 mg/kg body weight 1 time per day in the first 2 weeks, then 3.5 mg/kg body weight 2 times a day. For older children, the drug is prescribed at 4 mg/kg body weight 2 times a day. The maximum daily dose, regardless of age, is 400 mg. The total duration of treatment is determined individually.
To prevent the transmission of HIV infection from mother to child during childbirth, a woman is given 200 mg of the drug orally once. Then, within 3 days after birth, the child is given the drug orally at a single dose of 2 mg/kg body weight.
Release form: tablets of 200 mg - 60 and 100 pieces per package, suspension - in a bottle of 240 ml (5 ml 50 mg).
Special instructions: Taking the drug during pregnancy and breastfeeding is undesirable and is allowed as a last resort. In this case, it is necessary to transfer the child to donor or artificial feeding. The drug is prescribed in combination with 2-3 other antiretroviral drugs, since viruses develop resistance to it. If allergic reactions occur, the drug is discontinued. If there is a break in treatment for more than 7 days, then the drug is then started with introductory dosages (smaller). The drug does not reduce the risk of infection of sexual partners. It reduces the effectiveness of hormonal contraceptives. Monitoring the condition of the liver is mandatory. There is no information on the safety and effectiveness of viramune in children. The drug reduces the ability to drive vehicles.
Antifungal drugs
Antifungal drugs are used to treat fungal diseases of the skin and hair, nails, mucous membranes and internal organs. They are used topically and externally, consumed orally, intravaginally, and administered intravenously. Antifungal drugs suppress the proliferation of fungi and cause their death. Azoles, allylamines and polyene antibiotics are of primary importance in the treatment of fungal diseases.
Azoles
Azoles are drugs related to triazole and imidazole derivatives. They are obtained synthetically. Azoles for systemic use (orally, intravenously) include fluconazole, voriconazole, itraconazole, and ketoconazole. Among the azoles, isaconazole, miconazole, clotrimazole, bifonazole, oxyconazole, and ketoconazole are used topically. The most famous of them (ketoconazole) is currently used orally less and less due to its high toxicity. It is most often prescribed locally.
Azole drugs damage the membrane of fungal cells, which mainly leads to slowing down and stopping their reproduction. Drugs in this group are effective against diseases caused by fungi Candida albicans, cryptococci, histoplasma, blastomycetes, coccidioides, and paracoccidioides. Resistance to azoles is found in the fungi Candida glabrata, Candida cruzei, zygomycetes and aspergillus.
Azoles for internal use are well absorbed from the gastrointestinal tract. Side effects most often include nausea and vomiting, abdominal pain, headache, stool disorders, and allergic rashes. Topical azoles accumulate in the skin.
Fluconazole
Active ingredient: fluconazole.
Pharmacological action: triazole derivative. Slows down the formation of ergosterol and disrupts the transport of substances through the fungal cell membrane. Affects cryptococci, Candida fungi, fungi that cause microsporia, trichophytosis.
Indications: candidal diseases, systemic and local (stomatitis, vaginitis), cryptococcosis (including cryptococcal meningitis). Used for fungal infections of the skin in the groin area, nails, pityriasis versicolor, paracoccidioidomycosis, histoplasmosis, sporotrichosis. Prescribed for prophylactic purposes in immunodeficiency conditions, including acquired immunodeficiency syndrome (AIDS).
Contraindications: hypersensitivity to the drug and other triazoles, pregnancy. The drug is not prescribed to children under 1 year of age.
Side effects: On the part of the digestive system, abdominal pain, increased gas formation in the intestines, nausea, and diarrhea are noted. There may be dizziness and headache. Sometimes allergic reactions ranging from skin rash to anaphylactic shock are observed.
Directions for use: orally or intravenously. The drug is prescribed 50-400 mg 1 time per day. The frequency of administration and duration of treatment are determined individually. In case of renal failure, the dose of the drug is reduced.
Release form: capsules of 50 mg - 7 pieces per package, or 150 mg - 1 piece per package.
Special instructions: when the drug is prescribed during breastfeeding, the child is transferred to donor or artificial feeding. Taking fluconazole together with oral hypoglycemic drugs may result in an excessive decrease in blood glucose levels.
Itraconazole
Active ingredient: itraconazole
Pharmacological action: triazole derivative. The drug disrupts the formation of ergosterol in the cell membrane of the fungus. Affects aspergillus, blastomycetes, cryptococci, histoplasma, paracoccidioides, microsporia and trichophytosis fungi, Candida fungi.
Indications: fungal diseases of the skin, including the genitals, nails, mucous membranes (oral cavity, eyes, vagina).
Contraindications: hypersensitivity to the drug, internal use of astemizole, midazolam, cisapride, triazolam, terfenadine, pregnancy.
Side effects: dysfunction of the stomach and intestines, liver, obstructive jaundice. There may be dizziness and headache. Allergic manifestations are often observed in the form of skin rash, itching, and Quincke's edema. Long-term treatment leads to menstrual irregularities, decreased potassium levels in the blood and hair loss.
Directions for use: orally, after meals, 100 mg 1 time per day or 200 mg 1–2 times per day.
The duration of treatment is determined individually (from one week to 12 months).
Release form: 100 mg capsules – 7 pieces per package.
Special instructions: the drug causes fetal malformations, so women of childbearing age must use contraceptives during treatment. When the drug is prescribed during breastfeeding, the child is transferred to donor or artificial feeding. The drug is prescribed with caution for liver and kidney diseases. If there are signs of liver failure, the drug is discontinued. The absorption of fluconazole decreases while taking drugs that reduce the acidity of gastric juice.
Clotrimazole
Active ingredient: clotrimazole.
Pharmacological action: antifungal drug of the imidazole group. It disrupts the formation of ergosterol in the fungal cell membrane, leading to metabolic disorders in it and further death. Affects mold and yeast fungi, dermatophytes, fungi that cause erythrasma and lichen versicolor. In addition, the drug has an antibacterial effect against staphylococci and streptococci, bacteroides, gardnerella, corynebacteria, and trichomonas.
Indications: erythrasma, lichen versicolor, fungal infections of the skin, including the feet.
Contraindications: hypersensitivity to the components of the drug.
Side effects: There may be redness, itching, and burning at the site of application of the drug.
Directions for use: externally. A thin layer of cream is applied 2-3 times a day to clean, dry skin, which is pre-washed with neutral soap. The duration of treatment is determined individually, usually 4 weeks or more. For fungal infections of the feet, it is recommended to continue treatment for another 2 weeks after the signs of the disease disappear. Treatment for tinea versicolor usually lasts 1–3 weeks.
Release form: 1% cream – 20 g in a tube (1 g contains 10 mg).
Special instructions: During pregnancy and lactation, the drug is prescribed in extreme cases. The drug is not used in ophthalmic practice. Co-administration of nystatin reduces the effectiveness of clotrimazole.
Triderm
Active ingredient: betamethasone dipropionate, clotrimazole, gentamicin.
Pharmacological action: external combination drug. Betamethasone reduces inflammation and allergies, swelling and itching of the skin. Clotrimazole has an antifungal effect against trichophytes, epidermophytes, microsporia, and Candida fungi. Gentamicin affects gram-negative (pseudomonas, aerobacteria, E. coli, Proteus, Klebsiella) and gram-positive (Staphylococcus aureus, streptococcus) bacteria. It slows down their growth and development.
Indications: dermatophytosis, including in the groin area, athlete's foot, fungal skin lesions in combination with a bacterial infection.
Contraindications: hypersensitivity to the components of the drug, period of breastfeeding.
Side effects: Redness, swelling, burning, itching, and pigmentation changes may occur at the site of application of the drug.
Directions for use: locally. A thin layer of the drug is applied to the affected skin and healthy skin around it 2 times a day. Duration of treatment is 3–4 weeks.
Release form: cream or ointment - 15 g in a tube (1 g contains 640 mcg of betamethasone dipropionate, 10 mcg of clotrimazole, 1 mg of gentamicin).
Special instructions: It is not recommended to prescribe the drug during pregnancy. The drug is not used in ophthalmic practice. Avoid contact with wounds and damaged skin. It is possible that microflora may develop resistance to the drug. In this case it is cancelled. The use of the drug in children is possible only under the supervision of a doctor.
Allylamines
Allylamines are antifungal drugs obtained synthetically. They affect many fungi and cause their death. Basically, drugs in this group are used to treat fungal diseases of the skin and its derivatives. Use internally and externally.
Lamisil
Active ingredient: Terbinafine hydrochloride.
Pharmacological action: an antifungal drug from the group of allylamines with a broad spectrum of action. It affects fungi that affect the skin, nails and hair: different types of trichophytes, microsporia, Candida fungi, phytosporia, epidermophytes. In relation to yeast fungi, the drug can have different effects - suppress cell growth or cause their death. The specific action depends on the type of yeast. When the drug is taken orally, it accumulates in the skin, hair and nails in a concentration sufficient to kill fungi.
Indications: onychomycosis (dermatophytoses), fungal infections of the scalp, fungal infections of the skin on the torso and limbs. For lichen versicolor, the drug is effective only when applied topically.
Contraindications: hypersensitivity to the drug. The drug is not prescribed to children under 2 years of age or weighing less than 12 kg.
Side effects: dysfunction of the gastrointestinal tract (discomfort in the stomach, significant loss of appetite, nausea, abdominal pain, stool disorders). There may be skin rashes like urticaria, pain in muscles and joints. Sometimes taste sensitivity is impaired. In rare cases, liver function is disrupted and jaundice develops. Very rarely there is a decrease in the number of neutrophils, granulocytes, and platelets in the blood. In general, the drug is well tolerated, and side effects are rare and mild.
Directions for use: orally, adults are prescribed 250 mg once a day. Children weighing up to 20 kg are prescribed 62.5 mg, children weighing 20–40 kg are prescribed 125 mg, and children weighing over 40 kg are prescribed 250 mg. The drug is taken 1 time per day. The duration of treatment for fungal infections of the feet is 2–6 weeks, and for skin lesions in other places – 2–4 weeks. Treatment for onychomycosis is longer - 6-12 weeks.
Release form: tablets of 125, 250 mg - 14 and 28 pieces per package.
Special instructions: It is not recommended to prescribe the drug during pregnancy and breastfeeding. In the latter case, it is necessary to transfer the child to donor or artificial feeding. An overdose of the drug is manifested by dizziness, nausea and pain in the epigastric region. For chronic liver diseases and impaired renal function, the drug is prescribed at half the dose.
Exoderil
Active ingredient: naftifine hydrochloride.
Pharmacological action: external antifungal drug belonging to the allylamine group. It has a detrimental effect on mold fungi, dermatophytes, and causative agents of sporotrichosis. Effective against trichophytes, microsporia, aspergillus, epidermophytes. The effect on yeast fungi can be destructive or manifest itself in inhibition of their growth and development. The drug has an antimicrobial effect on gram-negative and gram-positive microorganisms. In addition, it has anti-inflammatory activity and reduces itching. Has a long-lasting effect (up to 24 hours).
Indications: fungal skin diseases, including candidiasis, pityriasis versicolor, onychomycosis, fungal infections of interdigital skin folds. The drug is used for a combination of fungal and bacterial infections.
Contraindications: hypersensitivity to the drug.
Side effects: Redness and dryness of the skin and burning are rarely observed. In these cases, the drug continues to be used.
Directions for use: externally. The cream is applied to the skin in the affected area once a day. The skin is first cleaned and dried. The duration of treatment for candidiasis is 4 weeks, for dermatomycosis – 2–4 weeks. For the treatment of onychomycosis, the drug is prescribed 2 times a day for up to 6 months. After the signs of the disease disappear, treatment is continued for another 2 weeks.
Release form: 1% solution for external use - in a bottle of 10 ml (10 mg in 1 ml), 1% cream - in tubes of 15 and 30 g (10 mg in 1 g).
Special instructions: If the treatment rules are followed, the drug does not have a negative effect on the fetus and newborn. Avoid getting the medicine into your eyes or wounds.
Antifungal antibiotics
Some antibiotics, such as polyene antibiotics, have an antifungal effect. They are of natural origin - produced by microorganisms. Medicines in this group act on the membrane of the fungal cell, disrupt metabolic processes in it and thus cause death. They have the widest spectrum of action.
Almost all drugs in this group are not absorbed from the intestine when taken orally and from the surface of the skin when used externally.
Pimafucin
Active ingredient: natamycin.
Pharmacological action: polyene antibacterial drug of the macrolide group, which has an antifungal effect. It has a detrimental effect on fungi. Candida fungi are resistant to the drug. Reduced sensitivity to the drug in dermatophytes. Complete resistance to pimafucin does not develop.
Indications: fungal diseases of the skin and mucous membranes, including the intestines, genitals, nails, as well as those developing during treatment with glucocorticosteroids, antibiotics, and cytostatics.
Contraindications: hypersensitivity to the drug.
Side effects: if taken orally, there may be nausea and stool disorders. Topical use of pimafucin, especially vaginally, may cause irritation and burning.
Directions for use: inside, locally. For fungal infections of the intestines, adults are prescribed the drug orally at 100 mg 4 times a day, and for children - 100 mg 2 times a day for 7 days. For fungal diseases of the skin and nails, the drug is applied once a day to the affected areas. The duration of treatment is determined individually.
The drug is used vaginally for 3–6 days – 100 mg per day. Suppositories are inserted into the vagina before bed, while lying down, deeply. If necessary, pimafucin is additionally prescribed orally - 100 mg 4 times a day for 10–20 days.
Release form: 100 mg tablets - 20 pieces per package, 2% cream - 30 g in a tube (1 g contains 20 mg), 100 mg suppositories - 3 pieces per package.
Special instructions: The use of the drug during pregnancy and breastfeeding is allowed. Treatment is interrupted during menstruation. During treatment, sexual intercourse is excluded.
Antiseptics
Antiseptics are a group of drugs widely used in the treatment and prevention of infectious diseases. They prevent or slow down the development of microbial flora, which makes them indispensable in many medical specialties. In addition, antiseptics are used to disinfect surgical instruments and treat hospital premises.
Septolete plus
Active ingredient: benzocaine + cetylpyridinium chloride.
Pharmacological action: has an analgesic and antiseptic effect. Cetylpyridinium belongs to the group of antiseptics and is active against bacteria, some viruses and fungi. Benzocaine has analgesic properties, reduces the sensitivity of the mucous membrane of the oral cavity and pharynx, relieves pain when swallowing, eliminates burning of the mucous membrane and other unpleasant sensations caused by the infectious-inflammatory process.
Indications: inflammatory diseases of the oral mucosa, gums, pharynx, larynx (acute respiratory viral infections, sore throat). For sore throat, the drug can only be used in the first 2-3 days, otherwise the degree of infection becomes too strong for the drug to have its effect.
Contraindications: allergy to the drug, children under 6 years of age, pregnancy and lactation. For superficial wounds of the mucous membrane, it is undesirable to use Septolete Plus, since cetylpyridinium, while providing an antimicrobial effect, simultaneously slows down the recovery process. In addition, a contraindication is intolerance to fructose, which is contained in the drug.
Side effects: allergic reactions, nausea, stool disorders. Undesirable effects occur very rarely, but if they occur, use of the product should be discontinued.
Directions for use: Children under 12 years old take 1 lozenge up to 4 times a day, dissolving it in the mouth until completely dissolved. It is advisable to take the medication at regular intervals. For patients over 12 years of age, the drug can be used up to 8 times a day, also 1 lozenge.
Release form: lozenges (contain 5 mg of benzocaine and 1 mg of cetylpyridinium chloride) - 10 pieces per package.
Special instructions: The drug should not be taken during or shortly before meals or washed down. The use of the drug in small doses is safe for patients with diabetes, since Septolet Plus does not contain sugar.
Picloxidine
Active ingredient: Picloxidine hydrochloride.
Pharmacological action: has a disinfecting effect, fights against bacteria, viruses and fungi, and has found its use in ophthalmic practice.
Indications: prevention and treatment of keratitis, conjunctivitis (including allergic ones to prevent the development of purulent complications), blepharitis, trachoma. Can be used to prevent infection after eye surgery. Not used for iritis, iridocyclitis.
Contraindications: individual intolerance to the drug.
Side effects: allergies, redness of the conjunctiva, temporary lacrimation and decreased visual acuity.
Directions for use: the solution is instilled 1 drop into each eye, gently pulling back the lower eyelid. The procedure is carried out 2–6 times a day, preferably at regular intervals. The course of treatment is 3-10 days.
Release form: 0.05% eye drops – in a 10 ml bottle.
Special instructions: when using the drug together with other eye products (drops, ointments), at least 15 minutes should pass between treatments. If after instillation of the drug the patient notices a decrease in visual acuity, then for half an hour you should not perform work that requires increased attentiveness and reaction speed.
Hexamidine
Active ingredient: hexamidine.
Pharmacological action: has antiseptic properties and is used externally. Hexamidine is usually used in complex preparations.
Indications: for the prevention of bacterial, viral or fungal infections of the skin, mouth and nose, genitals; treatment of wounds during dressings; mild forms of bacterial skin infection (pyoderma, juvenile acne).
Contraindications: individual intolerance to the drug. Hexamidine is not suitable for the prevention and treatment of eye infections due to its too strong irritant effect on the conjunctiva. In addition, it cannot be used to treat infectious and inflammatory processes of the ear. The antiseptic has relatively weak disinfection properties, so it cannot be used to treat the skin before injections or disinfect surgical instruments.
Side effects: allergic reactions (itching, redness of the skin and mucous membranes at the site of application of the drug); when treating skin with wounds and abrasions, irritation, the appearance of eczema, and allergic dermatitis are possible.
Directions for use: The solution is applied to a cotton or gauze swab, and the required area of the skin or mucous membranes is treated with it. When preventing oral diseases, rinse with the solution for 10–15 seconds. Antiseptic treatment is carried out 2–6 times a day.
Release form: solution for external use - in a 250 ml bottle.
Special instructions: Hexamidine loses its effectiveness if you treat the skin with it at the same time as soap.
Prikhodko Valentin Ivanovich, Copyright © 2010 - 2016 E-mail: [email protected]
, Ukraine.
Reprinting of materials with a mandatory link to the site is WELCOME!
All materials on the site are provided for informational and educational purposes only.
The site administration does not claim their authorship and is not responsible for their content.
Despite the undoubted successes and achievements of modern medicine in the fight against infections caused by pathogenic fungi, the number of people suffering from such diseases is not decreasing.
In addition to superficial and urogenital mycoses, deep lesions associated with HIV, organ donation, hemato-oncology, and nursing newborns are quite often recorded today.
Antimycotic drugs, used in various regimens for the treatment and prevention of fungal infections, must exhibit high activity against the pathogen, have a prolonged effect, have a minimal frequency of formation of resistance of the pathogenic organism, have good compatibility with pharmaceuticals from other groups, be effective, safe, and easy to use.
These requirements are met, in particular, by an antimycotic from the azole group - fluconazole, which acts as the active substance of broad-spectrum antifungal drugs. One of them is a drug Diflucan.
Inflammatory diseases of the genitourinary system most often occur due to pathogenic microorganisms.
The most common pathogens are chlamydia, trichomonas, mycoplasma, ureaplasma, and fungi.
A person can be a carrier of pathogenic bacteria and not know it. Often a person becomes infected with several types of microorganisms at once.
Treatment of such conditions requires a comprehensive approach. The drug Safocid includes three drugs with different spectrum of action.
For most infections, a single dose of the drug complex is sufficient. But only a doctor can determine the advisability of using Safocid.
Cefuroxime is an antibacterial drug from the group of cephalosporins. It has an extended spectrum of action.
Shows effectiveness against gram-positive and gram-negative bacteria. Prescribed for various ailments, including diseases of the pancreas, as well as tonsillitis, bronchitis, infectious diseases of the skin, and many others.
Its advantage over other drugs is its fairly rapid and stable effect. When exposed to pathogenic microorganisms, it has a destructive effect on the synthesis of bacterial cell walls.
In addition, like all drugs of the cephalosporin group, this drug is less likely than other antibiotics to provoke the development of bacterial resistance.
Antibiotics play a priority role in the fight against infectious bacterial diseases. Of the 6,000 antibiotics of various groups known today, no more than 10% are not only effective, but also safe in the treatment of human infections.
Macrolides, widely used in the treatment of diseases caused by pathogenic microorganisms, are considered to be the safest antibacterial drugs. A characteristic feature of macrolides, which distinguishes them, for example, from penicillins or cephalosporins, is primarily hypoallergenic.
In addition, antibiotics of this group have a high potential for antimicrobial activity, as well as an intracellular pharmacokinetic effect, which makes it easier for the macroorganism to tolerate their effects.
The first representative of macrolides was the drug Erythromycin.
Mikosist It is considered one of the most effective drugs for the treatment of fungal diseases.
The main active ingredient of the drug is fluconazole.
The drug can be used for both acute and chronic (recurrent) forms of diseases caused by Candida, Microsporum, Trichophyton fungi, as well as some other types of mycoses.
A special feature of the drug is its high bioavailability and rapid absorption. In some cases, taking Mikosist may be indicated for preventive purposes (in particular, in the presence of malignant tumors or treatment with antibiotics that affect the intestinal microflora).
Most people at least once in their lives encounter fungal infections of the mucous membranes and skin.
You can get rid of fungal diseases with the help of special medications.
One of the effective means is "Candide".
This is an external antifungal drug, the main component of which is clotrimazole.
But you should not prescribe the remedy yourself; if problems arise, you should initially consult with doctors.
Preparations based on clotrimazole can cope with most fungal infections.
Before starting use, make sure that the infection is sensitive to clotrimazole.
To do this, if unpleasant symptoms appear, you should consult a doctor.
He must determine the cause of the problem and select the appropriate drug.





