10.1. Antigens
10.1.1. General information
The life activity of each macroorganism takes place in direct contact with cells foreign to it, precellular life forms and individual bioorganic molecules. Being foreign, these objects are fraught with great danger, since they can disrupt homeostasis, affect the course of biological processes in the macroorganism and even lead to its death. Contact with foreign biological objects represents an early signal of danger for the immune system; they are the main irritant and target of the acquired immune system. Such objects are called antigens(from Greek anti- against, genos- create).
The modern definition of the term “antigen” is a biopolymer of an organic nature, genetically foreign to a macroorganism, which, when it enters the latter, is recognized by its immune system and causes immune reactions aimed at its elimination. The study of antigens is key to understanding the basics of molecular genetic mechanisms immune defense macroorganism, since antigen is the driving force of the immune response, as well as the principles of immunotherapy and immunoprophylaxis.
Antigens have diverse origins. They are a product of natural biological synthesis of any foreign organism; they can be formed in one’s own body when structural changes already synthesized molecules during biodegradation, disruption of their normal biosynthesis or genetic mutation of cells. In addition, antigens may be
obtained artificially as a result of scientific work or by targeted chemical synthesis. However, in any case, the antigen molecule will be distinguished by genetic foreignness in relation to the macroorganism into which it has entered. Theoretically, an antigen can be a molecule of any organic compound.
Antigens can enter the macroorganism in a variety of ways: through the skin or mucous membranes, directly into the internal environment of the body, bypassing the integument or being formed inside it. When antigens enter a macroorganism, they are recognized by immunocompetent cells and cause a cascade of various immune reactions aimed at their inactivation, destruction and removal.
10.1.2. Properties of antigens
The characteristic properties of antigens are antigenicity, immunogenicity and specificity.
Antigenicity- this is the potential ability of an antigen molecule to activate components of the immune system and specifically interact with immune factors (antibodies, clone of effector lymphocytes). In this case, the components of the immune system do not interact with the entire antigen molecule, but only with its small section, which is called antigenic determinant, or epitope.
Distinguish linear, or sequential, antigenic determinants, for example the primary amino acid sequence of the peptide chain, and superficial, or conformational, located on the surface of an antigen molecule and resulting from a secondary or higher conformation. At the terminal portions of the antigen molecules are located terminal epitopes, and in the center of the molecule - central. There are also deep, or hidden, antigenic determinants that appear during the destruction of the biopolymer.
The size of the antigenic determinant is small. It is determined by the characteristics of the receptor part of the immunity factor and the structure of the epitope. For example, the antigen-binding region of an immunoglobulin molecule is capable of recognizing a linear antigenic determinant consisting of 5 amino acid residues. The formation of a conformational determinant requires 6-12 amino acid residues. The killer T-receptor apparatus for
determination of foreignness requires a nanopeptide included in the MHC class I, T-helper - an oligopeptide of 12-25 amino acid residues in complex with MHC class II.
The molecules of most antigens are quite large. Their structure contains many antigenic determinants that are recognized by antibodies and lymphocyte clones of different specificities. Therefore, the antigenicity of a substance depends on the presence and number of antigenic determinants in the structure of its molecule.
The structure and composition of the epitope are critical. Replacing at least one structural component of the molecule leads to the formation of a fundamentally new antigenic determinant. Denaturation leads to the loss of existing antigenic determinants or the appearance of new ones, as well as specificity.
Foreignness is prerequisite to realize antigenicity. The concept of “foreignness” is relative, since immunocompetent cells are not capable of directly analyzing foreign genetic code, but only products synthesized from a foreign genetic matrix. Normally, the immune system is immune to its own biopolymers, unless it has acquired foreign characteristics. In addition, in some pathological conditions, as a result of dysregulation of the immune response (see autoantigens, autoantibodies, autoimmunity, autoimmune diseases), one’s own biopolymers can be perceived by the immune system as foreign.
Foreignness is directly dependent on the evolutionary distance between the organism and the source of antigens. The farther organisms are from each other in taxonomic terms, the more foreign and, therefore, immunogenic their antigens are. Alienity is noticeably manifested even between individuals of the same species, since the replacement of at least one amino acid is effectively recognized by antibodies in serological reactions.
At the same time, antigenic determinants of even genetically unrelated creatures or substances may have a certain similarity and are capable of specifically interacting with the same immune factors. These antigens are called cross-reacting. Similarities were also found in the antigenic determinants of streptococcus, myocardial sarcolemma and basal
kidney membranes, Treponema pallidum and lipid extract from the myocardium of cattle, the causative agent of plague and human erythrocytes of blood group 0(I). The phenomenon when one organism is masked by the antigens of another to protect against immune factors is called antigenic mimicry.
10.1.2.1. Immunogenicity
Immunogenicity- the potential ability of an antigen to cause a specific productive response in relation to itself in the macroorganism. Immunogenicity depends on three groups of factors: the molecular characteristics of the antigen, the kinetics of the antigen in the body, and the reactivity of the macroorganism.
The first group of factors includes nature, chemical composition, molecular weight, structure and some other characteristics.
Nature antigen largely determines immunogenicity. Proteins and polysaccharides have the most pronounced immunogenicity, nucleic acids and lipids have the least. At the same time, their copolymers - lipopolysaccharides, glycoproteins, lipoproteins - are capable of sufficiently activating the immune system.
Immunogenicity depends to some extent on chemical composition antigen molecules. For protein antigens, the diversity of their amino acid composition is important. Monotonous polypeptides, built from one amino acid, practically do not activate the immune system. The presence of aromatic amino acids, such as tyrosine and tryptophan, in the structure of the protein molecule significantly increases immunogenicity.
Optical isomerism of the structural components of the antigen molecule is important. Peptides built from L-amino acids are highly immunogenic. On the contrary, a polypeptide chain built from dextrorotatory isomers of amino acids may exhibit limited immunogenicity when administered in small doses.
In the spectrum of immunogenicity, there is a certain hierarchy of antigenic determinants: epitopes differ in their ability to induce an immune response. When immunized with a certain antigen, reactions to individual antigenic determinants will predominate. This phenomenon is called immunodominance. By modern ideas it is caused by differences in the affinity of epitopes to the receptors of antigen-presenting cells.
Are of great importance size And molecular weight antigen. Small polypeptide molecules weighing less than 5 kDa are generally low immunogenic. An oligopeptide capable of inducing an immune response must consist of 6-12 amino acid residues and have a molecular weight of about 450 D. As the size of the peptide increases, its immunogenicity increases, but this dependence is not always met in practice. Thus, with equal molecular weight (about 70 kDa), albumin is a stronger antigen than hemoglobin.
It has been experimentally proven that highly dispersed colloidal solutions of antigen poorly induce an immune response. Aggregates of molecules and corpuscular antigens - whole cells (erythrocytes, bacteria, etc.) are much more immunogenic. This is due to the fact that corpuscular and highly aggregated antigens are better phagocytosed than individual molecules.
The steric stability of the antigen molecule also turned out to be significant. When proteins are denatured to gelatin, immunogenicity is lost along with conformational rigidity. Therefore, gelatin solutions are widely used for parenteral administration.
An important condition for immunogenicity is solubility antigen. For example, high-molecular compounds keratin, melanin, natural silk, etc. are insoluble in water, do not form colloidal solutions in the normal state and are not immunogens. Due to this property, horsehair, silk, catgut, etc. are used in clinical practice for stitching organs and tissues.
The second group of factors is associated with the dynamics of antigen entry into the body and its elimination. Thus, the dependence of the immunogenicity of an antigen on places And way his introductions which is due to the structural features of the immune system at the sites of antigen intervention.
The strength of the immune response depends on quantities incoming antigen: the more of it, the more pronounced the immune reaction of the macroorganism.
Third group combines factors that determine the dependence of immunogenicity on the state of the macroorganism: heredity and functional characteristics. It is well known that the result
The immunization date is to a certain extent related to the genotype of the individual. There are genera and species of animals that are sensitive and insensitive to certain antigens. For example, rabbits and rats show little or no reaction to certain bacterial antigens that can cause an extremely strong immune response in a guinea pig or mouse.
10.1.2.2. Specificity
Specificity is the ability of an antigen to induce an immune response to a strictly defined epitope. The specificity of an antigen is largely determined by the properties of its constituent epitopes.
10.1.3. Classification of antigens
Based on individual characteristic properties, the entire variety of antigens can be classified according to their origin, nature, molecular structure, degree of immunogenicity, degree of foreignness, direction of activation and availability of immune response.
By origin distinguish between exogenous (arising outside the body) and endogenous (arising inside the body) antigens. Among endogenous ones, auto- and neoantigens deserve special attention. Autogenous antigens (autoantigens) are structurally unchanged antigens of one's own body, synthesized in the body under physiological conditions. Normally, autoantigens are non-immunogenic due to the formed immunological tolerance(immunity) or their inaccessibility to contact with immunity factors - these are the so-called behind-barrier antigens. When tolerance is broken or the integrity of biological barriers is violated (inflammation, injury), the components of the immune system begin to specifically respond to autoantigens by producing specific immune factors (autoantibodies, a clone of autoreactive lymphocytes). Neoantigens, unlike autoantigens, they arise in the body as a result genetic mutations or modifications and are always foreign.
By nature: biopolymers of protein (proteids) and non-protein (polysaccharides, lipids, lipopolysaccharides, nucleic acids, etc.) nature.
By molecular structure: globular (the molecule has a spherical shape) and fibrillar (thread-shaped).
By degree of immunogenicity: complete and inferior. Full antigens have pronounced antigenicity and immunogenicity - the immune system of a sensitive organism reacts to their introduction by producing immunity factors. Such substances, as a rule, have a fairly large molecular weight (more than 10 kDa), a large molecule (particle) size in the form of a globule, and interact well with immune factors.
Defective antigens, or haptens(the term was proposed by K. Landsteiner), they are antigenic - they are able to specifically interact with ready-made immunity factors (antibodies, lymphocytes), but are not capable of inducing an immune response in the body when administered under normal conditions. Most often, haptens are low molecular weight compounds (molecular weight less than 10 kDa).
If you artificially enlarge a hapten molecule - connecting it with a strong bond to a sufficiently large protein molecule, it is possible to force the immune system of the macroorganism to specifically respond to the hapten as a full-fledged antigen and produce immunity factors. The carrier protein molecule is called schlepper(tractor). In this case, the specificity of the conjugate molecule is determined by the hapten part, and the immunogenicity is determined by the carrier protein. Using conjugates for immunization, antibodies to hormones are obtained medicines and other low-immunogenic compounds.
By degree of foreignness: xeno-, allo- and isoantigens. Xenogeneic antigens (or heterologous) - common to organisms at different stages of evolutionary development, for example, belonging to different genera and species. For the first time, the phenomenon of commonality of a number of antigens in animals different types was noted by D. Forsman (1911). By immunizing a rabbit with a suspension of guinea pig organs, the scientist obtained an immune serum capable of interacting with sheep red blood cells. It was later found that the guinea pig and the sheep have a number of structurally similar antigenic determinants that cross-react. Subsequently, the list of such xenogeneic antigens was significantly expanded and they received the general name "Forsman antigens".
Allogeneic antigens (or group) - common to genetically unrelated organisms, but belonging to the same species. Based on alloantigens, the general population of organisms can be divided into separate groups. An example of such antigens in humans are blood group antigens (AB0 system, etc.). Allogeneic tissues during transplantation are immunologically incompatible - they are rejected or lysed by the recipient. Microbes can be divided into serogroups based on group antigens, which is used in microbiological diagnostics.
Isogenic antigens (or individual) - common only to genetically identical organisms, for example, identical twins, inbred lines of animals. Isografts have almost complete immune compatibility and are not rejected. Isoantigens in humans include histocompatibility antigens, and in bacteria they are typical antigens that do not undergo further cleavage.
Within an individual organism, in certain organs or tissues, antigens specific to them are found that are not found anywhere else. These antigens are called organo- And tissue-specific.
Depending on physical and chemical properties antigen, the conditions of its introduction, the nature of the reaction and the reactivity of the macroorganism, immunogens, tolerogens and allergens are distinguished. Immunogens capable of inducing a normal productive reaction of the immune system - the production of immunity factors (antibodies, antigen-reactive clones of lymphocytes). In clinical practice, immunogens are used for immunodiagnosis, immunotherapy, and immunoprophylaxis of many pathological conditions.
Tolerogen is the exact opposite of an immunogen. It forms immunological tolerance or unresponsiveness to epitopes of a given substance (see section 11.6). A tolerogen, as a rule, is a monomer with low molecular weight, high epitope density and high dispersity. Tolerogens are used for the prevention and treatment of immunological conflicts and allergies by inducing artificial unresponsiveness to individual antigens.
Allergen, unlike an immunogen, it forms a pathological reaction of the body in the form hypersensitivity immediate or delayed type (see section 11.4). According to its properties
an allergen is no different from an immunogen. In clinical practice, allergens are used to diagnose infectious and allergic diseases.
According to the direction of activation and availability of the immune response, i.e. the need to involve T-lymphocytes in the induction of an immune response, distinguish T-dependent And T-independent antigens. The immune reaction in response to the introduction of a T-dependent antigen is realized with the obligatory participation of T-helper cells. These include most of the known antigens. The development of an immune response to T-independent antigens does not require the involvement of T helper cells. These antigens are capable of directly stimulating B lymphocytes for antibody production, differentiation and proliferation, as well as inducing an immune response in athymic animals. T-independent antigens have a relatively simple structure. These are large molecules with a molecular weight of more than 10 3 kDa, are polyvalent and have numerous epitopes of the same type. T-independent antigens are mitogens and polyclonal activators, for example, polymeric flagellin (contractile protein of bacterial flagella), lipopolysaccharide, tuberculin, etc.
It is necessary to distinguish from T-independent antigens superantigens. This is a group of substances, mainly of microbial origin, that can nonspecifically cause a polyclonal reaction. The superantigen molecule is capable of interfering with the cooperation of the antigen-presenting cell and the T-helper cell and generating a false signal for recognizing a foreign substance.
Superantigens are capable of simultaneously nonspecifically activating a huge number of immunocompetent cells (up to 20% or more), causing hyperproduction of cytokines and low-specific immunoglobulins, massive death of lymphocytes due to apoptosis and the development of secondary functional immunodeficiency. Superantigen properties have been found in staphylococcal enterotoxin, Epstein-Barr virus proteins, rabies, HIV and some other microbial agents.
10.1.4. Antigens of the human body
The study of alloantigenic properties of tissues began with K. Landsteiner, who in 1901 discovered the system of group antigens of erythrocytes (AB0). In the human body
secrete a wide variety of antigens. They are not only needed for the full development and functioning of the entire organism as a whole, but also carry important information in clinical and laboratory diagnostics, determining the immune compatibility of organs and tissues in transplantology, as well as in scientific research. Of the greatest medical interest among allogeneic antigens are blood group antigens, among isogenic antigens - histocompatibility antigens, and in the group of organ- and tissue-specific antigens - cancer-embryonic antigens.
10.1.4.1. Human blood group antigens
Human blood group antigens are located on the cytoplasmic membrane of cells, but are most easily detected on the surface of red blood cells. That's why they got the name "erythrocyte antigens". To date, more than 250 different erythrocyte antigens are known. However, the most important clinical significance have antigens of the AB0 and Rh system (Rh factor): they must be taken into account when performing blood transfusions, organ and tissue transplants, prevention and treatment of immunoconflict complications of pregnancy, etc.
Antigens of the AB0 system are found in blood plasma, lymph, secretions of mucous membranes and other biological fluids, but are most pronounced on erythrocytes. They are synthesized by many cells of the body, including nucleated precursors of red blood cells, and are freely secreted into the intercellular space. These antigens can appear on the cell membrane either as a product of cellular biosynthesis or as a result of sorption from intercellular fluids.
Antigens of the AB0 system are highly glycosylated peptides: 85% are carbohydrate parts and 15% are polypeptide parts. The peptide component consists of 15 amino acid residues. It is constant for all ABO blood groups and is immunologically inert. The immunogenicity of the AB0 system antigen molecule is determined by its carbohydrate part.
In the AB0 antigen system, there are three variants of antigens that differ in the structure of the carbohydrate part: H, A and B. The basic molecule is the H antigen, the specificity of which is determined by three carbohydrate residues. Antigen A has an additional fourth carbohydrate residue in its structure - N-acetyl-D-galactose, and antigen B - D-galactose. Antigens of the AB0 system have independent
dependent allelic inheritance, which determines the presence of 4 blood groups in the population: 0(I), A(II), B(III) and AB(IV). In addition, antigens A and B have several allotypes (for example, A 1, A 2, A 3 ... or B 1, B 2, B 3 ...), which occur in the human population with different frequencies.
Antigens of the AB0 system are determined in an agglutination reaction. However, given the high population polymorphism of this antigenic system, before blood transfusion a biological test is required to determine the compatibility of the blood of the recipient and the donor. An error in determining group affiliation and transfusion of a patient with incompatible blood group lead to the development of acute intravascular hemolysis.
Another important system of erythrocyte antigens is Rh antigen system(Rh) or Rh factors. These antigens are synthesized by red blood cell precursors and are found primarily on red blood cells because they are water insoluble. Rh antigen is a thermolabile lipoprotein. There are 6 varieties of this antigen. Genetic information about its structure is encoded in numerous alleles of three linked loci (D/d, C/c, E/e). Depending on the presence or absence of the Rh antigen in the human population, two groups are distinguished: Rh-positive and Rh-negative individuals.
Matching the Rh antigen is important not only for blood transfusion, but also for the course and outcome of pregnancy. During the pregnancy of an Rh-negative mother, a Rh-positive fetus may develop Rhesus conflict. This pathological condition associated with the production of anti-Rhesus antibodies that can cause an immunological conflict: miscarriage or neonatal jaundice (intravascular immune lysis of red blood cells).
Due to the fact that the density of the Rh antigen on the erythrocyte membrane is low and its molecule has weak antigenicity, the Rh factor is determined on the erythrocyte membrane in an indirect agglutination reaction (Coombs reaction).
10.1.4.2. Histocompatibility antigens
On the cytoplasmic membranes of almost all cells of the macroorganism are found histocompatibility antigens. Most of them relate to the system main complex
histocompatibility, or MHC (from English. Main Hystocompatibility Complex). It has been established that histocompatibility antigens play a key role in the specific recognition of “friend or foe” and the induction of an acquired immune response, determine the compatibility of organs and tissues during transplantation within the same species and other effects. Much credit for the study of MHC belongs to J. Dosse, P. Dougherty, P. Gorer, G. Snell, R. Zinkernagel, R.V. Petrov, who became the founders immunogenetics.
MHC was first discovered in the 60s of the twentieth century in experiments on genetically pure (inbred) lines of mice during an attempt at interline transplantation of tumor tissues (P. Gorer, G. Snell). In mice, this complex was named H-2 and was mapped to chromosome 17.
In humans, the MHC was described somewhat later in the works of J. Dosset. He was designated as HLA(from English Human Leukocyte Antigen), since it is associated with leukocytes. Biosynthesis HLA is determined by genes localized in several loci of the short arm of chromosome 6.
MHC has a complex structure and high polymorphism. Histocompatibility antigens are glycoproteins tightly bound to the cytoplasmic membrane of cells. Their individual fragments are structurally similar to immunoglobulin molecules and therefore belong to a single superfamily. There are two main classes of MHC molecules (I and II), which combine many structurally similar antigens encoded by many allelic genes. No more than two varieties of each MHC gene product can be expressed simultaneously on an individual's cells. MHC class I induces predominantly a cellular immune response, and MHC class II induces a humoral response.
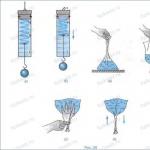
MHC class I consists of two non-covalently linked polypeptide chains (α and β) with different molecular weights (Fig. 10.1). The α-Chain has an extracellular region with a domain structure (α 1 -, α 2 - and α 3 domains), transmembrane and cytoplasmic. The β-chain is a β 2 -microglobulin adhered to the α-domain after expression of the α-chain on the cytoplasmic membrane of the cell. α 1 - and α 2 -Domains of the α chain form the Bjorkman gap - the area responsible for the sorption and presentation of molecules
Rice. 10.1. Scheme of the structure of antigens of the major histocompatibility complex: I - MHC class I; II - MHC class II
antigen. The MHC class I Bjorkmann gap accommodates a nanopeptide that is easily detected by specific antibodies.
Assembly of the MHC class I-antigen complex occurs intracellularly continuously in the endoplasmic reticulum. Its composition includes any endogenously synthesized peptides, including viral ones, where they are transferred from the cytoplasm using a special protein, proteasomes. The peptide included in the complex imparts structural stability to MHC class I. In its absence, the function of a stabilizer is performed chaperone (calnexin).
MHC class I is expressed on the surface of almost all cells, except erythrocytes and villous trophoblast cells (prevention of fetal rejection). The density of MHC class I reaches 7000 molecules per cell, and they cover about 1% of its surface. They are characterized by a high rate of biosynthesis - the process is completed in 6 hours. The expression of MHC class I is enhanced under the influence of cytokines, for example γ-interferon.
Currently, humans have more than 200 different variants HLA I class. They are encoded by genes mapped
in three main subloci of the 6th chromosome and are inherited and manifest independently: HLA-A, HLA-B and HLA-C. Locus A unites more than 60 variants, B - 130, and C - about 40. Independent inheritance of sublocus genes in a population forms an infinite number of non-repeating combinations HLA I class. Each person has a strictly unique set of histocompatibility antigens, with the only exception being identical twins. Main biological role HLA Class I - they determine biological individuality (biological passport) and are “self” markers for immunocompetent cells. Infection of a cell with a virus or its mutation changes the structure HLA Class I, which is a signal for the activation of T-killers (CD8 + lymphocytes) to destroy the object.
HLA Class I is detected on lymphocytes in the reaction of microlymphocytolysis with specific sera, which are obtained from multiparous women, patients after massive blood transfusion, and also using monoclonal antibodies.
There are a number of fundamental differences in the structure and function of MHC class II. The complex is formed by two non-covalently linked polypeptide chains (α and β), having a similar domain structure (see Fig. 10.1). Both chains are transmembrane peptides and are “anchored” in the cytoplasmic membrane. The Bjorkmann gap in MHC class II is formed simultaneously by both chains. It contains an oligopeptide of 12-25 amino acid residues in size, which is inaccessible to specific antibodies. MHC class II includes a peptide taken up from the extracellular environment by endocytosis, rather than synthesized by the cell itself. MHC class II molecules are expressed on the surface of a limited number of cells: dendritic cells, B lymphocytes, T helper cells, activated macrophages, mast cells, epithelial cells, and endothelial cells. The detection of MHC class II on atypical cells is currently regarded as immunopathology. Biosynthesis of MHC class II occurs in the endoplasmic reticulum and is expressed on the cytoplasmic membrane of the cell within 1 hour after endocytosis of the antigen. Expression of the complex can be enhanced by γ-interferon and reduced by prostaglandin E 2 .
In mice, the histocompatibility antigen is called Ia-antigen, and in humans, by analogy, it is called HLA II class.
According to available data, the human body is characterized by extremely high polymorphism HLA Class II, which is largely determined by the structural features of the β-chain. The complex includes products of three main loci: HLA- DR, DQ and DP. At the same time, the DR locus unites about 300 allelic forms, DQ - about 400, and DP - about 500.
The presence and type of MHC class II is determined by serology (microlymphocytotoxic test) on B-lymphocytes and cellular immune responses (mixed culture of lymphocytes). Specific antibodies to MHC class II are obtained in the same way as to class I. Testing in a mixed culture of lymphocytes allows the identification of minor components of MHC class II that are not detectable serologically.
MHC class II is involved in the induction of the acquired immune response. Fragments of the antigen molecule are expressed on the cytoplasmic membrane of a special group of cells, which is called antigen presenting. The main ones are dendritic cell, macrophage and B-lymphocyte. The structure of MHC class II with the peptide included in it in complex with cofactor molecules of CD antigens is perceived and analyzed by T helper cells (CD4 + lymphocytes). In case of recognition of foreignness, the T-helper begins the synthesis of the corresponding immunocytokines, and the mechanism of a specific immune response is activated: proliferation and differentiation of antigen-specific clones of lymphocytes.
In addition to the histocompatibility antigens described above, class III MHC molecules have been identified. The locus containing the genes encoding them is wedged between classes I and II and separates them. MHC class III includes some complement components (C2, C4), heat shock proteins, tumor necrosis factors, etc.
10.1.4.3. Tumor-associated antigens
In 1948-1949 prominent Russian microbiologist and immunologist L.A. When developing the viral theory of cancer, Zilber proved the presence of an antigen specific to tumor tissue. Later in the 60s of the twentieth century G.I. Abelev (in experiments on mice) and Yu.S. Tatarinov (when examining people) discovered an embryonic version of serum albumin in the blood serum of patients with primary liver cancer - α-fetoprotein. To date, many tumor-associated
ny antigens. However, not all tumors contain specific marker antigens, nor do all markers have strict tissue specificity.
Tumor-associated antigens are classified by location and genesis. Distinguish whey, secreted by tumor cells into the intercellular environment, and membrane. The latter were called tumor-specific transplantation antigens, or TSTA(from English Tumor-Specific Transplantation Antigen).
Viral, embryonic, normal overexpressed and mutant tumor-associated antigens are also distinguished. Viral- are products of oncoviruses, embryonic are normally synthesized in the embryonic period. Well known α-fetoprotein (fetal albumin), a normal testicular protein (MAGE 1,2,3, etc.), markers of melanoma, breast cancer, etc. Chorionic gonadotropin, normally synthesized in the placenta, is found in choriocarcinoma and other tumors. In melanoma, the normal enzyme tyrosinase is synthesized in large quantities. From mutant proteins should be noted protein Ras- GTP-binding protein involved in transmembrane signal transmission. Markers of breast and pancreatic cancer, intestinal carcinoma are modified mucins (MUC 1, 2, etc.).
In most cases, tumor-associated antigens are products of the expression of genes that are normally turned on during the embryonic period. They are weak immunogens, although in some cases they can induce a reaction of cytotoxic T-lymphocytes (killer T-lymphocytes) and are recognized as part of MHC molecules (HLA) I class. Specific antibodies synthesized to tumor-associated antigens do not inhibit tumor growth.
10.1.4.4. CD antigens
Group antigens are found on the cell membrane, uniting cells with certain morphofunctional characteristics. These molecules are called cell differentiation cluster antigens, or CD antigens. Cell Differentiation Antigens, or Cluster Definition). Structurally, they are glycoproteins and mostly belong to the immunoglobulin superfamily.
The list of CD markers is quite extensive and has about 200 options. Among the variety of CD antigens, the most widely used are markers of immunocompetent cells. For example, CD3 is expressed in the population of T-lymphocytes, CD4 - T-helper cells, and CD8 - cytotoxic T-lymphocytes - killer T-lymphocytes, CD11a - mono- and granulocytes, CD11b - natural killer cells, CD19-22 - B-lymphocytes. Information about the structure is encoded in various parts of the genome, and expression depends on the stage of cell differentiation and its functional state.
CD antigens are important in the diagnosis of immunodeficiency states. Determination of CD markers is carried out in immunological reactions using monoclonal antibodies.
10.1.5. Antigens of microbes
10.1.5.1. Antigens of bacteria
In the structure of a bacterial cell, flagellar, somatic, capsular and some other antigens are distinguished (Fig. 10.2). Flagellates, or H-antigens are localized in their flagella and represent epitopes of the contractile protein flagellin. When heated, flagellin denatures and the H antigen loses its specificity. Phenol has no effect on this antigen.
Somatic, or O-antigen, associated with the bacterial cell wall. It is based on lipopolysaccharides. O-antigen is heat stable and is not destroyed by prolonged boiling. However, aldehydes (for example, formaldehyde) and alcohols disrupt its structure.
If you immunize an animal with live bacteria that have flagella, antibodies will be produced simultaneously to the O- and H-antigens. Introducing a boiled culture to an animal stimulates the biosynthesis of antibodies to a somatic antigen. A bacterial culture treated with phenol will induce the formation of antibodies to flagellar antigens.
Capsule, or K-antigens found in capsule-forming bacteria. As a rule, K-antigens consist of acidic polysaccharides (uronic acids). At the same time, in the anthrax bacillus, this antigen is built from polypeptide chains. Based on sensitivity to heat, there are three types of K-antigen: A, B and L.
 Rice. 10.2. Main bacterial antigens (explanation in text)
Rice. 10.2. Main bacterial antigens (explanation in text)
The greatest thermal stability is characteristic of group A - they do not denature even with prolonged boiling. Group B can withstand short heating (about 1 hour) to 60 °C. Group L breaks down quickly at this temperature. Therefore, partial removal of the K-antigen is possible by prolonged boiling of the bacterial culture.
On the surface of the pathogen typhoid fever and other enterobacteria that are highly virulent, a special version of the capsular antigen can be detected. It got the name virulence antigen, or Vi-antigen. Detection of this antigen or antibodies specific to it is of great diagnostic importance.
Bacterial bacteria also have antigenic properties. protein toxins, enzymes and some other substances that are secreted by bacteria into the environment (for example, tuberculosis
kulin). Tetanus, diphtheria and botulinum toxins are among the strong full-fledged antigens, so they are used to produce molecular vaccines - toxoids.
In the antigenic composition of some bacteria, there is a group of antigens with strongly expressed immunogenicity, whose biological activity plays a key role in the formation of the pathogenicity of the pathogen - the binding of such antigens by specific antibodies almost completely inactivates the virulent properties of the microorganism and provides immunity to it. These antigens are called protective.
10.1.5.2. Antigens of viruses
In the structure of the viral particle there are nuclear(or cows), capsid(or shell) and supercapsid antigens. On the surface of some viral particles there are special V antigens- hemagglutinin and neuraminidase enzyme. Viral antigens differ in origin. Some of them are virus-specific, encoded in the nucleic acid of the virus. Others, which are components of the host cell (carbohydrates, lipids), form the supercapsid of the virus at its birth by budding.
The antigenic composition of the virion depends on the structure of the viral particle itself. In simply organized viruses, antigens are associated with nucleoproteins. These substances are highly soluble in water and are therefore designated as S-antigens (from lat. solutio- solution). In complex viruses, some of the antigens are associated with the nucleocapsid, and the other is located in the outer shell, or supercapsid.
The antigens of many viruses are characterized by a high degree of variability, which is associated with constant mutations in the genetic material of viruses. An example is the influenza virus,
10.1.6. Processes occurring with the antigen in the macroorganism
Antigenic intervention is a process that occurs in stages with certain dynamics over time. Moreover, at each stage of the appearance and spread in the macroorganism, the antigen faces powerful resistance from a developed network of various immune factors (Table 10.1).
Table 10.1. Antigen processing in the macroorganism
 There are several ways of penetration and spread of antigen in the macroorganism. They can appear within the macroorganism itself (endogenous origin) or come from outside (exogenous origin). Exogenous antigens can penetrate the macroorganism:
There are several ways of penetration and spread of antigen in the macroorganism. They can appear within the macroorganism itself (endogenous origin) or come from outside (exogenous origin). Exogenous antigens can penetrate the macroorganism:
Through defects of the skin and mucous membranes (as a result of wounds, microtraumas, insect bites, scratching, etc.);
By absorption in the gastrointestinal tract (endocytosis by epithelial cells);
Intercellular (with incomplete phagocytosis);
In the body, the antigen can spread with lymph (lymphogenous pathway) and blood (hematogenous pathway) to various organs and tissues. In this case, it is most often filtered in the lymph nodes, spleen, as well as in the lymphoid accumulations of the liver, intestines and other organs, where it comes into contact with immune defense factors.
The response of these factors occurs almost immediately. The factors of innate immunity come into play first, since this system does not require a long time to activate. If the antigen has not been inactivated or eliminated within 4 hours, the acquired immune system is activated: specific recognition is ensured "friend or foe" regulatory factors (cytokines) and immune defense (specific antibodies, clones of antigen-reactive lymphocytes) are produced.
The cumulative effect of all links and levels of the immune defense of the macroorganism, regardless of the degree of their involvement in the process, is aimed at:
Binding and blocking biologically active sites of the antigen molecule;
Antigen destruction or rejection;
Disposal, isolation (encapsulation) or removal of antigen remnants from the macroorganism.
As a result, restoration of homeostasis and structural integrity of the macroorganism is achieved. At the same time, immune memory, tolerance or allergy is formed.
10.2. Human immune system
The specific function of monitoring the genetic constancy of the internal environment of the body and preserving its biological and species individuality is performed by the immune system.
10.2.1. Structural and functional elements of the immune system
The immune system is a specialized, anatomically distinct lymphoid tissue. It is distributed throughout the body in the form of various lymphoid formations and individual cells, and accounts for 1-2% of body weight. Anatomically, the immune system is divided into central and peripheral organs, and functionally into organs of cell reproduction and selection ( bone marrow, thymus), control of the external environment or exogenous intervention (lymphoid systems of the skin and mucous membranes), control of the genetic constancy of the internal environment (spleen, lymph nodes, liver, blood, lymph).
The main functional cells are lymphocytes. Their number in the body reaches 10 12. To the number functional cells The immune system also includes mononuclear and granular leukocytes, mast and dendritic cells. Some cells are concentrated in individual organs of the immune system, while others move freely throughout the body. The schematic structure of the immune system is shown in Fig. 10.3.
10.2.1.1. Central organs of the immune system
The central organs of the immune system, the bone marrow and the thymus gland or thymus, are the organs of reproduction and selection of cells of the immune system. Happening here lymphopoiesis- birth, reproduction (proliferation) and differentiation of lymphocytes to the stage of precursors or mature non-immune (naive) cells, as well as their “training”. In birds, the central organs of the immune system include the bursa of Fabricius. (bursa fabricii), localized in the cloaca area.
Bone marrow located in the spongy substance of bones (epiphyses tubular bones, sternum, ribs, etc.). Here are pluripotent stem cells (PPSCs), which are ro-
 Rice. 10.3. Organs of the human immune system
Rice. 10.3. Organs of the human immune system
the predecessors of all shaped elements blood, including immunocompetent cells. Precursors of B- and T-lymphocytes are formed in the bone marrow stroma, which subsequently migrate to the B-zones of the macroorganism and the thymus, respectively. Phagocytes and some dendritic cells are also produced in the bone marrow. Plasma cells can also be found in it - the result of terminal differentiation of B lymphocytes.
Thymus gland, thymus, or thymus gland, located in the upper part of the retrosternal space. This organ is distinguished by its special morphogenesis. The thymus is formed during intrauterine development. By the time of birth, the mass of the thymus reaches 10-15 g, it finally matures by the age of five, and maximum size reaches 10-12 years of age (weight 30-40 g). After puberty, organ involution begins - replacement occurs lymphoid tissue fatty and connective.
The thymus has a lobular structure. Its structure distinguishes between the medulla and cortical layers. In the stroma of the cortical layer there is a large number of epithelial cells of the cortex, called “nurse cells”, which with their processes form a fine-mesh network where maturing lymphocytes are located. In the border, cortical-medullary layer, dendritic cells of the thymus are located, and in the medulla - epithelial cells medulla.
T-lymphocyte precursors come from the bone marrow to the thymus cortex. Here, under the influence of thymic factors, they actively multiply, differentiate (transform) into mature T-lymphocytes and “learn” to recognize foreign antigenic determinants.
The learning process includes positive And negative selection. The criterion for “learning” is the quality of T-cell antigen reception (specificity and affinity) and cell viability.
Positive selection occurs in the cortex with the help of epithelial cells. Its essence is to support clones of T-lymphocytes, the receptors of which effectively bind to MHC molecules expressed on epithelial cells, regardless of the structure of their own incorporated oligopeptides. Cortical epithelial cells secrete thymic growth factors that activate the proliferation of T-lymphocytes.
Negative selection carried out by dendritic cells in the border cortical-medullary zone of the thymus. Its goal is to cull autoreactive T-lymphocyte clones. Cells that react positively to the MHC-autologous peptide complex are destroyed by inducing apoptosis.
As a result of selection, more than 99% of T-lymphocytes do not withstand the tests and die. Only less than 1% of cells turn into mature forms capable of recognizing only foreign biopolymers in combination with autologous MHC. Every day, about 10 6 mature “trained” T-lymphocytes leave the thymus with the blood and lymph flow and migrate to various organs and tissues.
The maturation and “training” of T lymphocytes in the thymus is important for the formation of immunity. Absence or underdevelopment of the thymus gland with a congenital defect in the development of the thymus gland - aplasia or hypoplasia of the organ, its surgical removal or radiation damage leads to a sharp decrease in the effectiveness of the immune defense of the macroorganism. Meanwhile, thymectomy in adults practically does not lead to serious defects in the immune system.
10.2.1.2. Peripheral organs of the immune system
Peripheral organs of the immune system include the spleen, lymph nodes, appendix, liver, tonsils pharyngeal ring, group lymphatic follicles, blood, lymph, etc. In these organs, immunogenesis takes place - reproduction and final maturation of the precursors of immunocompetent cells and immunological surveillance is carried out. In functional terms, the peripheral organs of the immune system can be divided into organs that control the internal environment of the body (lymph nodes, spleen, tissue migrating cells) and its skin and mucous membranes (appendix, lymph follicles and accumulations).
Lymph nodes- small round anatomical bean-shaped formations that are located along the lymphatic vessels. Each part of the body has regional lymph nodes. In total, there are up to 1000 lymph nodes in the human body. Lymph nodes perform the function of a biological sieve - lymph is filtered through them and antigens are retained and concentrated. On average, about 10 9 lymphocytes pass through the lymph node per hour.
In the structure of the lymph node, a distinction is made between the cortex and medulla. The cortical stroma is divided into sectors by connective tissue trabeculae. It is divided into a superficial cortical layer and a paracortical zone. In the sectors of the superficial cortical layer there are lymphatic follicles with centers for the reproduction of B-lymphocytes (germinal centers). Follicular dendritic cells are also found here, promoting the maturation of B lymphocytes. The paracortical layer is a zone of T lymphocytes and interdigital dendritic cells, descendants of dermal Langerhans cells. The medulla is formed by strands of connective tissue, between which macrophages and plasma cells are located.
Within the lymph node, antigenic stimulation of immunocompetent cells occurs and a specific immune response system is activated, aimed at neutralizing the antigen.
Spleen- This is the organ through which all blood is filtered. It is located in the left iliac region and has a lobular structure. Lymphoid tissue forms white pulp. In structure, there are primary, periarterial lymphoid follicles (surrounding the arteries along their course) and secondary ones, located on the borders of the primary follicles. Primary lymphoid accumulations are populated predominantly by T-lymphocytes, and secondary ones - by B-lymphocytes and plasma cells. In addition, phagocytes and reticular dendritic cells are found in the stroma of the spleen.
The spleen, like a sieve, retains antigens that are in the bloodstream and aged red blood cells. This organ is called the red blood cell cemetery. Here antigenic stimulation of immunocompetent cells occurs, the development of a specific immune response to the antigen and its neutralization.
Liver plays a special role in the immune system. It contains more than half of all tissue macrophages and most of the natural killer cells. Lymphoid populations of the liver provide tolerance to food antigens, and macrophages utilize immune complexes, including those sorbed on aging erythrocytes.
Group lymphatic follicles(Peyer's patches) are accumulations of lymphoid tissue in the mucous membrane of the small intestine. Such formations are also found in the vermiform appendix of the cecum - the appendix. In addition, throughout
Along the gastrointestinal tract, from the esophagus to the anus, there are single lymphatic follicles. They provide local immunity to the intestinal mucosa and its lumen and regulate the species and quantitative composition of its normal microflora.
Accumulation of lymphoid elements in the form pharyngeal ring tonsils provides local immunity in the nasopharynx, oral cavity and upper respiratory tract, protects their mucous membranes from the introduction of microbes and other genetically foreign agents transmitted by airborne droplets or dust, and regulates local normal flora.
Lymph- liquid tissue of the body, which is contained in lymphatic vessels and nodes. It includes all compounds coming from the interstitial fluid. The main and practically the only cells of lymph are lymphocytes. In its composition, these cells carry out circulation in the body.
IN blood precursors and mature T- and B-lymphocytes, polymorphonuclear leukocytes, and monocytes circulate. Lymphocytes make up 30% total number leukocytes. At one time, less than 2% of the total number of lymphocytes is present in the blood.
10.2.1.3. Immune system cells
The specific function of immune defense is directly carried out by a large pool of cells of the myeloid and lymphoid blood lineages: lymphocytes, phagocytes and dendritic cells. These are the main cells of the immune system. In addition to them, many other cell populations (epithelium, endothelium, fibroblasts, etc.) can be involved in the immune response. The listed cells differ morphologically, in functional activity, markers (specific molecular marks), receptor apparatus and biosynthesis products. However, most cells of the immune system are closely related genetically: they have a common precursor, a pluripotent bone marrow stem cell (Fig. 10.4).
On the surface of the cytoplasmic membrane of immune system cells there are special molecules that serve as their markers. In the 80s of the last century, an international nomenclature of membrane markers of human leukocytes was adopted, called "CD antigens"(Table 10.2)
 Rice. 10.4. Scheme of immunogenesis (explanations in the text)
Rice. 10.4. Scheme of immunogenesis (explanations in the text)
Table 10.2. Main CD markers of cells involved in the immune response
 Continuation of the table. 10.2
Continuation of the table. 10.2
 End of table. 10.2
End of table. 10.2
 Note. ADCT - antibody-dependent cell-mediated cytotoxicity; APCs are antigen presenting cells.
Note. ADCT - antibody-dependent cell-mediated cytotoxicity; APCs are antigen presenting cells.
Based on their functional activity, cells participating in the immune response are divided into regulatory (inducer), effector, and antigen-presenting. Regulatory cells control the functioning of the components of the immune system by producing mediators - immunocytokines and ligands. These cells determine the direction of development of the immune response, its intensity and duration. Effectors are direct executors of immune defense through direct impact on the object or through the biosynthesis of biologically active substances with a specific effect (antibodies, toxic substances, mediators, etc.).
Antigen presenting cells perform a responsible task: they capture, process (process by limited proteolysis) and present the antigen to immunocompetent T cells as part of a complex with MHC class II. APCs lack specificity for the antigen itself. The MHC class II molecule can include any oligopeptides endocytosed from the intercellular environment, both its own and foreign. It has been established that most of the MHC class II complexes contain autogenous molecules and only a small proportion contains foreign material.
In addition to MHC class II, APCs express costimulatory factors (CD40, 80, 86) and many adhesion molecules. The latter provide close, spatially stable and long-lasting contact of the APC with the T-helper. In addition, APCs express CD1 molecules, which can be used to present lipid or polysaccharide antigens.
The main professional APCs are dendritic cells of bone marrow origin, B lymphocytes and macro-
phages. Dendritic cells are almost 100 times more effective than macrophages. The function of non-professional APCs can also be performed by some other cells in a state of activation - epithelial cells and endothelial cells.
The implementation of targeted immune protection of the macroorganism is possible due to the presence of specific antigen receptors (immunoreceptors) on the cells of the immune system. According to the mechanism of functioning, they are divided into direct and indirect. Direct immunoreceptors directly bind to the antigen molecule. Indirect immunoreceptors interact with the antigen molecule indirectly - through the Fc fragment of the immunoglobulin molecule (see section 11.1.2). This is the so-called Fc receptor (FcR).
Fc receptors vary in affinity. A high-affinity receptor can bind to intact IgE or IgG4 molecules and form a receptor complex in which the antigen-specific co-receptor function is performed by an immunoglobulin molecule. Basophils and mast cells have such a receptor. Low affinity FcR recognizes immunoglobulin molecules that have already formed immune complexes. It is found on macrophages, natural killer cells, epithelial cells, dendritic cells, and a variety of other cells.
The immune response is based on the close interaction of different cell populations. This is achieved through the biosynthesis by cells of the immune system of a wide range of immunocytokines. The vast majority of cells of the immune system constantly move in the internal environments of the body with blood and lymph flow and due to amoeboid motility.
The cellular elemental composition of the immune system is constantly renewed due to the division of stem cells. Those who have grown old and have worn out their biological resource, falsely activated, infected and genetically transformed cells are destroyed.
10.2.1.3.1. Lymphocytes
Lymphocytes are motile mononuclear cells. Depending on the place of maturation, these cells are divided into two populations: T- (thymus) and B- (bursa of Fabricius, bone marrow) lymphocytes. Lymphocytes play a key role in providing acquired (adaptive) immunity. They carry out
specific recognition of antigen, induction of cellular and humoral immune responses, various forms of immune response.
Lymphocyte populations are continuously renewed in the body, cells actively migrate between various organs and fabrics. However, the migration and settlement of lymphocytes in tissues is not a chaotic process. It is directional in nature and is strictly regulated by the expression of special adhesion molecules (integrins, selectins, etc.) on the membrane of lymphocytes, vascular endothelium and cellular elements of the stroma. Thus, immature T lymphocytes actively migrate to the thymus. Mature non-immune (“naive”) lymphocytes are tropic towards peripheral lymphoid organs and tissues. In this case, T- and B-lymphocytes populate only “their” areas - this is the so-called homing reception effect (from the English. home- house). Mature immune (activated) lymphocytes recognize the epithelium at the site of inflammation. Immunological memory cells always return to their places of origin.
The lifespan of non-immune lymphocytes is quite long. In T lymphocytes it reaches several months or years, and in B cells it lasts weeks or months. Immunological memory cells live the longest (see section 11.5) - up to 10 years or more. However, activated or terminally differentiated lymphocytes have a short life span (several days). Aged, falsely activated and autoreactive (reacting to self-antigens) lymphocytes are destroyed by inducing apoptosis. Dead lymphocytes are constantly replaced by new ones due to their proliferation in the central and peripheral organs immune system. The number of lymphoid populations is under strict control of the cells of the immune system itself.
To perform a specific function, lymphocytes carry direct antigen receptors on their surface and are immunocompetent cells. The immunoreceptor of the B lymphocyte and a special γδT lymphocyte recognizes the native epitope, i.e. directly distinguishes foreign substances. The immunoreceptor of a traditional T-lymphocyte is focused on oligopeptides in the MHC, i.e. recognizes the changed “own”.
Antigen-specific receptors of lymphocytes have a complex molecular structure, unique to each cell. For example
Measures, in T lymphocytes they consist of several polypeptide subunits that have polygenic coding. The number of genes that determine the structure of the V-region of this receptor (the variable region responsible for specific recognition) in an immature cell reaches 100. When a lymphocyte matures, as a result of recombination rearrangements in the V-genes, individual for each cell, an infinitely large number of variants of antigen specificity are formed receptor, reaching 10 12, which is comparable to the total population of T-lymphocytes. The formation of the B-cell receptor follows the same patterns. The biological meaning of the phenomenon is extremely important: the body constantly maintains a wide repertoire of specific lymphoid receptors, and cells are ready at any time to respond with a protective reaction to any possible antigen.
In such a situation, the appearance of T-lymphocytes specific for antigens of one’s own body is natural. However, they must be eliminated in the thymus at the early stages of their development. Therefore, they distinguish primary And secondary antigen recognition repertoire lymphoid populations. Primary is characterized by a set of receptor specificities that are formed during the formation of lymphocytes in the bone marrow of an individual. The secondary, or clonal, repertoire is the collection of receptor variants after the selection of autoreactive cell clones.
Antigen-specific reception in lymphocytes has standard mechanisms of implementation. The signal from the irritant (antigen) received by the extracellular part of the receptor is transmitted through the transmembrane region to its intracellular part, which already activates intracellular enzymes (tyrosine kinase, phosphorylase, etc.).
To trigger a productive reaction of a lymphocyte, aggregation of its receptors is necessary. In addition, auxiliary molecules are required to stabilize receptor-ligand interaction and perception of the co-stimulatory signal.
Among the lymphocytes, there are cells without the distinctive features of T- and B-lymphocytes. They got the name zero cells. In the bone marrow they account for about 50% of all lymphocytes, and in the blood - about 5%. Functional activity remains unclear.
B lymphocytes. B lymphocytes are predominantly effector immunocompetent cells, which account for about 15% of the total number of lymphocytes. There are two subpopulations of B lymphocytes: traditional B cells that do not have the CD5 - marker, and CD5 + B1 lymphocytes.
By electron microscopy, CD5 - B lymphocytes have rough surface, it detects CD19-22 and some others. Antigen-specific receptor function (BCR) perform special membrane forms of immunoglobulins. Cells express MHC class II, co-stimulatory molecules CD40, 80, 86, FcR to immune complexes and native molecules of class G immunoglobulin, receptor for mouse erythrocytes, immunocytokines, etc.
 Rice. 10.5. B-lymphocyte differentiation scheme: P - plasma cell; MB - B-lymphocyte of immunological memory; Bαα - synthesizes polymeric immunoglobulin A in the mucous membranes
Rice. 10.5. B-lymphocyte differentiation scheme: P - plasma cell; MB - B-lymphocyte of immunological memory; Bαα - synthesizes polymeric immunoglobulin A in the mucous membranes
The function of mature CD5 - B lymphocytes and their descendants (plasmocytes) is the production of immunoglobulins. In addition, B lymphocytes are professional APCs. They participate in the formation of humoral immunity, B-cell immunological memory and immediate hypersensitivity.
Differentiation and maturation of B lymphocytes (Fig. 10.5) occur first in the bone marrow and then in the peripheral organs of the immune system, where they are resettled at the precursor stage. The descendants of B lymphocytes are immunological memory cells and plasma cells. The main morphological features of the latter are the developed endoplasmic reticulum and the Golgi apparatus with a large number ribo-
catfish Plasmocytes have a short life span - no more than 2-3 days.
B1 lymphocytes are considered phylogenetically the most ancient branch of antibody-producing cells. The precursors of these cells migrate early to the tissues of the mucous membranes, where they maintain their population independently from the central organs of the immune system. The cells express CD5, synthesize low-affinity IgA and IgM to polysaccharide and lipid antigens of microbes and provide immune protection of mucous membranes from opportunistic bacteria.
The functional activity of B lymphocytes is controlled by molecular antigens and immunocytokines of T helper cells, macrophages and other cells.
T lymphocytes.T lymphocytes is a complex group of cells that originates from a pluripotent bone marrow stem cell, and matures and differentiates from precursors in the thymus. These cells account for about 75% of the entire lymphoid population. On the electron diffraction pattern, all T-lymphocytes have a smooth surface, their common marker is CD3, as well as the receptor for sheep erythrocytes. Depending on the structure of the antigen receptor (TCR) and functional orientation, the T-lymphocyte community can be divided into groups.
There are two types of TCRs: αβ and γδ. The first type is a heterodimer, which consists of two polypeptide chains - α and β. It is characteristic of traditional T lymphocytes known as helper T cells and killer T cells. The second is found on the surface of a special population of γδT lymphocytes.
T lymphocytes are also functionally divided into two subpopulations: immunoregulators and effectors. The task of regulating the immune response is performed by T helper cells. Previously, it was assumed that there are T-suppressors that can inhibit the development of the immune response (suppression). However, the cell has not yet been morphologically identified, although the suppressor effect itself exists. The effector function is carried out by cytotoxic lymphocytes T-killers.
In the body, T-lymphocytes provide cellular forms of the immune response (delayed-type hypersensitivity, transplantation immunity, etc.), determine the strength and duration of the immune reaction. Their maturation, differentiation and activity are controlled by cytokines and macrophages.
T-helpers. T-helpers or T-helpers are a subpopulation of T-lymphocytes that perform a regulatory function. They account for about 75% of the entire T-lymphocyte population. They carry the CD4 marker as well as αβ TCR, with the help of which the nature of the antigen presented to it by the APC is analyzed.
Reception of antigen by T-helper, i.e. analysis of its foreignness is a very complex process that requires high accuracy. It is promoted (Fig. 10.6) by the CD3 molecule (complexed with TCR), CD4 co-receptor molecules (have an affinity for the MHC class II molecular complex), adhesion molecules (stabilize intercellular contact), receptors (interact with costimulatory factors of the APC - CD28, 40L).
 Rice. 10.6. T-helper activation scheme (explanation in the text)
Rice. 10.6. T-helper activation scheme (explanation in the text)
Activated helper T cells produce a wide range of immunocytocytes, with which they control the biological activity of many cells involved in the immune response.
The population of T helper cells is heterogeneous. An activated CD4 + T lymphocyte (T Ω helper) differentiates into one of its descendants: T 1 or T 2 helper (Fig. 10.7). This differentiation is alternative and cytokine-directed. T 1 - or T 2 - helpers differ only functionally in the spectrum of cytokines produced.
T 1 helper produces IL-2, 3, γ-IFN, TNF, etc., necessary for the development of a cellular immune response, delayed-type hypersensitivity, and immune inflammation. The formation of this cell is determined by activated macrophage, natural and T-killer cells that synthesize IL-12 and γ-IFN.
T 2 helper produces IL-4, 5, 6, 9, 10, 13, etc., which support the humoral immune response, as well as hypersensitivity
 Rice. 10.7. T-helper differentiation scheme: T-x - T-helper; aM - activated macrophage; T-k - T-killer; aEK - activated natural killer; E - eosinophil; B - basophil; T - mast cell; γδT - γδT lymphocyte
Rice. 10.7. T-helper differentiation scheme: T-x - T-helper; aM - activated macrophage; T-k - T-killer; aEK - activated natural killer; E - eosinophil; B - basophil; T - mast cell; γδT - γδT lymphocyte
reality of immediate type. Differentiation towards the T2 helper is potentiated by γδT cells, basophils, mast cells and eosinophils that synthesize IL-4 and 13.
The body maintains a balance of T 1 -/T 2 helper cells, which is necessary for the development of an adequate immune response. T 1 - and T 2 - helpers are antagonists and inhibit each other's development. It has been established that T2 helper cells predominate in the body of newborns. Violation of the colonization of the gastrointestinal tract by normal microflora inhibits the development of the T 1 helper subpopulation and leads to allergization of the body.
Killer T cells (cytotoxic T lymphocytes). Killer T is a subpopulation of effector T lymphocytes, which account for approximately 25% of all T lymphocytes. CD8 molecules, as well as αβ, are detected on the surface of the killer T cell TCR to an antigen in combination with MHC class I, which distinguishes “self” cells from “foreign” cells. The CD3 molecule, which complexes with TCR and MHC class I-tropic CD8 co-receptor molecules (Fig. 10.8).
The killer T cell analyzes the cells of its own body in search of foreign MHC class I. Mutant cells, infected with a virus, or an allogeneic transplant carry on their surface such signs of genetic foreignness, and therefore are the target of the T-killer.
 Rice. 10.8. T-killer activation scheme (explanations in the text)
Rice. 10.8. T-killer activation scheme (explanations in the text)
Killer T eliminates target cells by antibody-independent cell-mediated cytotoxicity (ANCCT) (see section 11.3.2), for which it synthesizes a number of toxic substances: perforin, granzymes and granulysin. Perforin- a toxic protein that is synthesized by cytotoxic lymphocytes-T killers and natural killer cells. It has a non-specific property. Produced only by mature activated cells. Perforin is formed as a soluble precursor protein and accumulates in the cytoplasm in granules that are concentrated around TCR contacting the target cell to ensure local, targeted damage to the target cell. The contents of the granules are released into a narrow synaptic cleft formed by close contact between the cytotoxic lymphocyte and the target cell. Due to hydrophobic regions, perforin is integrated into the cytoplasmic membrane of the target cell, where, in the presence of Ca 2+ ions, it polymerizes into a transmembrane pore with a diameter of 16 nm. The resulting channel can cause osmotic lysis of the target cell (necrosis) and/or allow granzymes and granulysin to penetrate into it.
Granzymes is a general name for serine proteases synthesized by mature activated cytotoxic lymphocytes. There are three types of granzymes: A, B and C. After synthesis, granzymes accumulate in granules like perforin and together
Granulisin- an effector molecule with enzymatic activity, synthesized by cytotoxic lymphocytes. It is capable of triggering apoptosis in target cells, damaging the membrane of their mitochondria.
T-killer has enormous biological potential - it is called a serial killer. For short term it can destroy several target cells, spending about 5 minutes on each one. The effector function of the killer T cell is stimulated by the T 1 helper, although in some cases its help is not required. In addition to its effector function, activated killer T cells synthesize γ-IFN and TNF, which stimulate macrophages and potentiate immune inflammation.
γδ T lymphocytes. Among T-lymphocytes, there is a small population of cells with the CD4 - CD8 - phenotype, which carry on their surface a special TCRγδ-type - γδT-lymphocytes. Localized in the epidermis and mucous membrane of the gastrointestinal tract. Their total number does not exceed 1% of the total pool of T-lymphocytes, but in the integumentary tissues it can reach 10%.
γδT lymphocytes originate from an autonomous lineage of stem cells that migrated into the integumentary tissues at the early stages of embryogenesis. When mature, they bypass the thymus. Activated by cells of damaged epithelium of the gastrointestinal tract and epidermis, reproduction is enhanced by IL-7.
The antigen receptor of the γδT lymphocyte is similar to BCR, its active center directly binds to the epitope of the antigen without its preliminary processing and MHC participation. Antigenic determinants can be represented, for example, by CD1 molecules. γδTCRs are focused on recognizing some widespread microbial antigens (lipoproteins, heat shock proteins, bacterial superantigens, etc.).
γδT lymphocytes can be both effector, cytotoxic cells (take part in the removal of pathogens in the early stages of anti-infective defense), and regulators of immunoreactivity. They synthesize cytokines that activate local immunity and a local inflammatory response, including enhancing the formation of T2 helper cells. In addition, γδ cells produce IL-7 and control their own population.
The MHC class I receptor analyzes the density of its expression on the cell membrane. The deficiency of these molecules, observed during cancer cell transformation, also potentiates the cytotoxicity of NK.
Fabric ECs lead a more sedentary lifestyle and are found in large numbers in the liver and decidual membrane of the pregnant uterus. They carry the marker CD16 - CD56 a lot and a lot Fas-ligand. Implement ANCCT (see section 11.3.2). Target cells are lymphocytes that are activated, for example, by food antigens or fetal alloantigens and express Fas.
In addition to cytotoxic functions, EC produce cytokines (IL-5, 8, γ-IFN, TNF, granulocyte-monocyte-colony-stimulating factor-GM-CSF, etc.), activates the macrophage-phagocytic link, the development of the immune response and immune inflammation. The effector function of NK is enhanced by cytokines (IL-2, 4, 10, 12, γ-IFN, etc.).
Phagocytes(see section 9.2.3.1) - the most numerous morphologically heterogeneous fraction of immunocompetent cells. Perform regulatory and effector functions. Produce immunocytokines, enzymes, radical ions and other biological active substances, carry out extra- and intracellular killing and phagocytosis. In addition, macrophages are APCs - they provide processing and presentation of antigen to T helper cells.
Eosinophils- granular blood leukocytes. Contained in the blood, loose connective tissue, accumulate in large quantities in areas of local inflammation caused by helminths, and provide ADCT.
Eosinophils also synthesize cytokines (IL-3, 5, 8, GM-CSF, etc.), which stimulate the cellular immune system and the formation of T2 helper cells, and lipid mediators (leukotrienes, platelet-activating factor, etc.), which trigger an inflammatory reaction in the area. introduction of helminth.
Mast cells- non-migratory morphological elements of unknown origin, located sedentary along barrier tissues (lamina propria mucous membranes, in subcutaneous connective tissue) and in the connective tissue of blood vessels. Based on the set of biologically active compounds synthesized and localization, two types of mast cells are distinguished - cells mucous membranes And connective tissue.
Basophils- granulocytes derived from bone marrow stem cells and related to eosinophils. Their differentiation is alternatively determined by cytokines. They constantly migrate with the bloodstream, are attracted to the site of inflammation by anaphylotoxins (C3a, C4a and C5a) and are retained there with the help of corresponding homing receptors.
Basophil and mast cell synthesize a similar set of biologically active substances. They produce, accumulating in granules, vasoactive amines (histamine in humans and serotonin in rodents), sulfated glycosaminoglycans (chondroitin sulfate, heparin), enzymes (serine proteases, etc.), as well as the cytokine α-TNF. Leukotrienes (C4, D4, E4), prostaglandins are directly released into the intercellular space (PGD2, PGE2), cytokines (IL-3, 4, 5, 13 and GM-CSF) and platelet activating factor.
On the surface, basophils and mast cells carry high-affinity FcR to IgE and G4. The formed receptor complex specifically interacts with the epitope of the antigen/allergen. They also express FcR to IgG as part of the immune complex. The basophil and mast cell are activated by allergens, anaphylotoxins, mediators of activated neutrophils, norepinephrine, and inhibited by immune complexes.
The binding of the allergen to the receptor complex causes degranulation of the basophil and mast cell - a volley of biologically active compounds contained in the granules into the intercellular space, which cause the development of immediate hypersensitivity (type I allergic reaction).
The basophil and mast cell direct the differentiation of T helper cells towards the T 2 subpopulation and enhance eosinophilogenesis.
Dendritic cells- process cells of bone marrow origin. Localized in lymphoid organs and barrier tissues. They express MHC class II and costimulatory factors (CD40, 80, 86) on their surface. Capable of absorbing
spare by endocytosis, process (process) and present (present) the antigen to T helper cells in combination with MHC class II. It is the most active agricultural sector. Among the dendritic cells, Langerhans cells (in the epidermis), interdigital cells (in the lymph nodes) and dendritic cells of the thymus are well known.
10.2.2. Organization of the functioning of the immune system
The immune system has a complex organization - many different cell populations and soluble immune factors are involved in performing a specific function. Cells constantly circulate in the body, die in the process of vital activity and reproduce.
Depending on the specific need, a specific function of the immune system can be activated or suppressed (suppressed). However, any response of the immune system is carried out only with the constant interaction of almost all types of its cells, i.e. in conditions of intercellular cooperation. The irritant (activating signal) is an antigen. In the development of any immune response, a cascade of successively changing stages can be traced.
10.2.2.1. Interaction between cells of the immune system
A necessary condition for the functioning of the immune system is close intercellular cooperation, the basis of which is the receptor-ligand interaction. To communicate with each other, cells use various distant soluble factors and direct contact.
The synthesis of soluble factors is one of the universal methods of cell commutation with each other. These include cytokines, of which more than 25 are currently known. They represent a heterogeneous family of biologically active molecules that are diverse in structure and function and have a number of common properties:
As a rule, cytokines are not stored in the cell, but are synthesized after an appropriate stimulus;
To perceive a cytokine signal, the cell expresses a corresponding receptor that can interact with several different cytokines;
Cytokines are synthesized by cells of different lineages, levels and directions of differentiation;
Subpopulations of cells of the immune system differ in the range of synthesized cytokines and their receptors;
Cytokines have versatility, multiple effects and synergism;
Cytokines can affect both a nearby cell (paracrine regulation) and the producer itself (autocrine regulation);
Cytokine regulation is cascade in nature: activation of a cell by one cytokine causes the synthesis of another;
The vast majority of these are short-distance mediators - their effects manifest themselves at the site of production. At the same time, a number of pro-inflammatory cytokines (IL-1, 6, α-TNF, etc.) can have a systemic effect.
Cytokines differ in their leading functional orientation:
Mediators of preimmune inflammation (IL-1, 6,12, α-TNF);
Mediators of immune inflammation (IL-5, 9, 10, γ-IFN
Stimulators of proliferation and differentiation of lymphocytes (IL-2, 4, 13, transforming growth factor - β-TGF
Cell growth factors or colony stimulating factors
(IL-3, 7, GM-CSF, etc.);
Chemokines, or cellular chemoattractants (IL-8, etc.). A brief description of some cytokines is given in
Direct intercellular interaction is based on the reception of structures expressed on the membrane of the opponent cell. This requires sufficiently long and stable cell contact. This method of switching is used by T-helpers and T-killers when analyzing the foreignness of presented structures. The mechanism of action of costimulatory factors (pairs CD40-CD40-ligand, CD28-CD80, 86) also requires direct contact.
10.2.2.2. Activation of the immune system
Activation of the immune system implies the development of a productive immune response in response to antigenic irritation
Table 10.3. Characteristics of the main cytokines
 Continuation of the table. 10.3
Continuation of the table. 10.3
 Continuation of the table. 10.3
Continuation of the table. 10.3
 End of table. 10.3
End of table. 10.3
 Note. MIF - migration inhibitory factor.
Note. MIF - migration inhibitory factor.
and the appearance of products of destruction of tissues of the macroorganism. This is a complex multi-stage process that requires a long time for its induction - about 4 days. A critical event is the inability to eliminate the antigen by innate immune factors within a specified period.
The triggering mechanism of adaptive immunity is the recognition of “friend or foe”, which is carried out by T-lymphocytes with the help of their direct immunoreceptors - TCR. If the foreignness of a bioorganic molecule is determined, the second stage of the response is activated - intensive replication of a clone of highly antigen-specific lymphocyte effectors capable of interrupting antigenic intervention is launched. This phenomenon is called "clone expansion" In parallel, but somewhat later than proliferation, the differentiation of immune lymphocytes and the formation of immunological memory cells from it are stimulated, guaranteeing survival in the future.
Thus, productive activation of the immune system is associated with the proliferation and differentiation of antigen-reactive clones of immunocompetent cells. The antigen in this process plays the role of an inducer and a clonal selection factor. The mechanisms of the main stages of activation of the immune system are discussed below.
T-helper activation. The process (see Fig. 10.6) is carried out with the direct participation of APCs (dendritic cells, B lymphocytes and macrophages). After endocytosis and antigen processing in intracellular vesicles, APC integrates the resulting oligopeptide into an MHC class II molecule and displays the resulting complex on the outer membrane. On the surface of APCs, costimulatory factors are also expressed - molecules CD40, 80, 86, the powerful inducers of which are the products of destruction of integumentary tissues at the stage of preimmune inflammation.
T-helper with the help of adhesion molecules firmly connects to the surface of the APC. The T-helper immunoreceptor, together with the CD3 molecule, with the support of the CD4 co-receptor molecule, interacts with the antigen-MHC class II complex and analyzes the foreignness of its structure. Reception productivity depends on costimulatory effects in the CD28-CD80/86 and CD40-ligand-CD40 pairs.
If the antigen-MHC class II complex is recognized as foreign (more precisely, “not self”), the T-helper is activated. He is expressive
creates a receptor for IL-2 and begins to synthesize IL-2 and other cytokines. The result of T-helper activation is its reproduction and differentiation into one of its descendants - T 1 - or T 2 - helper (see Fig. 10.2). Any change in reception conditions stops the activation of the T-helper and can induce apoptosis in it.
B-lymphocyte activation. To activate a B lymphocyte (Fig. 10.9), the summation of three consecutive signals is necessary. The first signal is the result of the interaction of an antigen molecule with a specific BCR, the second is the interleukin stimulus of activated T helper cells and the third is the result of the interaction of costimulatory CD40 molecules with the CD40 ligand.
Activation initiates the proliferation and differentiation of the antigen-specific B lymphocyte (see Fig. 10.2). As a result, a clone of specific antibody producers appears within the germinal centers of lymphoid follicles. Differentiation allows you to switch the biosynthesis of immunoglobulins from classes M and D to more economical ones: G, A or E (rarely), increase the affinity of synthesized antibodies and form immunological memory B cells or plasma cells.
B-lymphocyte activation is a very delicate process. The absence of at least one of the stimuli (impaired intercellular cooperation, nonspecificity of the B-lymphocyte receptor, or antigen elimination) blocks the development of the antibody immune response.
Activation of killer T-cell. To perform the supervisory function, the T-killer comes into close and lasting contact with the potential
 Rice. 10.9. Scheme of B-lymphocyte activation (explanations in the text)
Rice. 10.9. Scheme of B-lymphocyte activation (explanations in the text)
target cell using adhesion molecules (see Fig. 10.8). Then the killer T cell immunoreceptor (αβ TCR) together with the CD3 molecule, with the support of the co-receptor molecule CD8, interacts with the MHC class I antigenic complex and analyzes its structure. Detection of deviations in favor of allogenicity activates killer T-cell to express the receptor for IL-2 and synthesize IL-2 and release effector molecules (perforin, granzymes, granulysin) from cytoplasmic granules into the synaptic cleft of intercellular contact.
For adequate development of the cellular form of the immune response, activating stimuli from the T1 helper are required. Killer T cells can function autonomously, independently initiating and maintaining clone formation due to autocrine stimulation of IL-2. However, this property is rarely realized.
10.2.2.3. Suppression of the immune response
Suppression or suppression of the immune response is a physiological reaction of the body, which normally completes the immune response and is aimed at inhibiting the expansion of antigen-specific clones of lymphocytes. Unlike immunological tolerance, an already initiated immune response is subject to suppression. There are three mechanisms of immunosuppression: destruction of clones of immunocompetent cells, inhibition of the activity of immunocompetent cells, elimination of the antigenic stimulus.
Immunocompetent cells can be eliminated by apoptosis. In this case, the following groups of cells are eliminated:
Terminal differentiated lymphocytes that have completed their biological program;
Activated lymphocytes that have not received an antigenic stimulus;
“worn out” lymphocytes;
Autoreactive cells.
Natural factors that initiate apoptosis are glucocorticoid hormones, Fas-ligand, α-TNF and other immunocytokines, granzymes and granulysin. Apoptotic destruction of target cells can be activated by killer T cells, NK cells with the CD16 - CD56 phenotype and T 1 helper cells.
In addition to apoptosis, antibody-dependent lymphocytolysis is possible. For example, with medical purpose use antilymphocyte
serum, which in the presence of complement causes lysis of lymphocytes. It is also possible to eliminate the lymphoid population by exposure to ionizing radiation or cytostatics.
The functional activity of immunocompetent cells can be inhibited by soluble factors of their competitors or descendants. The leading role belongs to immunocytokines with multiple effects. It is known, for example, that T2 helpers, γδT lymphocytes and mast cells with the help of IL-4, 13 prevent the differentiation of T0 helper cells into T1 cells. The latter, in turn, can block the formation of T2 helper by synthesizing γ-IFN. The proliferation of T and B lymphocytes is limited by β-TGF, which is produced by terminally differentiated T helper cells. The already mentioned T2 helper products (IL-4, 13 and β-TGF) suppress biological activity macrophages.
Suppression of the humoral immune system can be caused by immunoglobulins. Excessive concentrations of immunoglobulin G, binding to special receptors on the membrane of the B-lymphocyte, inhibit the biological activity of the cell and its ability to differentiate into a plasma cell.
The elimination of an antigen from the body in nature is observed when the body is completely freed from the pathogen with the development of sterile immunity. In clinical practice, the effect is achieved by cleansing the body by plasma or lymphosorption, as well as by neutralizing the antigen with antibodies specific for highly immunogenic epitopes.
10.2.2.4. Age-related changes immune system
There are two distinct stages in the development of the immune system. First, antigen independent, which starts with embryonic period development and partly continues throughout life. During this period, stem cells and a variety of antigen-specific lymphocyte clones are formed. Precursors of γδT and B1 lymphocytes migrate into the integumentary tissues and form autonomous lymphoid lineages.
Second stage, antigen dependent, continues from the moment of birth of an individual until its death. During this period, the immune system becomes familiar with the diversity of antigens around us. As biological experience accumulates, i.e. quantity and quality of productive contacts with antigens, selection occurs
and replication of individual clones of immunocompetent cells. Particularly intense expansion of clones is characteristic of childhood. During the first 5 years of life, the child's immune system has to absorb approximately 90% of biological information. Another 9% is perceived before puberty, at adult state only about 1% remains.
The child’s immune system has to cope with monstrous loads, which mainly fall on the humoral part of the immune system. In places with high population density and frequent inter-individual contacts (large cities), conditions are created for the long-term persistence of high concentrations of various pathogens. That's why children in big cities often get sick. However, one gets the impression of a total immunodeficiency generated by extreme environmental distress. Meanwhile, the evolutionarily inherent mechanisms of immune defense allow the child’s body to successfully cope with difficult natural tests of viability and adequately respond to vaccine prevention.
With age, the immune system changes its structure. In the adult body, up to 50% of the total lymphoid pool is represented by clones of cells that have undergone antigenic stimulation. The biological experience accumulated by the immune system is manifested by the formation of a narrow “library” of vital (actual) clones of lymphocytes specific to the main pathogens. Due to the longevity of immunological memory cells, actual clones become self-sufficient over time. They acquire the ability to self-sustain and become independent of the central organs of the immune system. The functional load on the thymus decreases, which is manifested by its age-related involution. Nevertheless, the body retains a wide range of unclaimed “naive” cells. They are able to respond to any new antigenic aggression.
precise elements of the body. Therefore, after birth, the system of adaptive cellular immunity begins to intensively develop, and with it the formation of clones of T 1 helper and T killer cells. It has been noted that disruption of postnatal colonization of the gastrointestinal tract by normal flora inhibits the process of adequate formation of the T 1 helper population in favor of T 2 cells. Excessive activity of the latter results in allergization of children's organisms.
A productive immune response, after its completion (neutralization and elimination of the antigen from the body), is also accompanied by changes in the clonal structure of antigen-reactive lymphocytes. In the absence of activating stimuli, the clone involutes. Unused cells die over time due to senescence or induction of apoptosis, and this process begins with more differentiated effector lymphocytes. The number of clones gradually decreases and is manifested by a gradual decline in the immune response. However, immunological memory cells persist in the body for a long time.
The senile period of life is characterized by the dominance of actual clones of antigen-specific lymphocytes in the immune system, combined with increasing immunosuppression and a decrease in general reactivity. Infections caused even by opportunistic microbes often become protracted or threatening. Cellular immunity also loses its effectiveness, and the volume of malignantly transformed cells gradually increases. Therefore, neoplasms are common in older people.
Tasks for self-preparation (self-control)
A. Label the effector cells of the immune system:
1. Dendritic cells.
2. B lymphocytes.
3. T-helpers.
4. T-killers. B. Mark APK:
1. Dendritic cells.
2. B lymphocytes.
3. Macrophages.
4. T-helpers.
IN. Mark the cells on which MHC class 2 receptor is expressed:
1. T-killers.
2. Dendritic cells.
3. Macrophages.
4. B lymphocytes.
G. Note the B cell markers:
1. MNS 2nd class.
D. Label the T helper receptor molecules:
E. Name the cells and mediators that take part in the formation of T 1 helper cells:
2. T-killers.
3. γ-Interferon.
4. Activated macrophage.
5. Mast cell.
AND. Name the cells and mediators that take part in the formation of T2 helper cells:
1. Basophils.
2. T-killers.
3. Mast cells.
Z. Name the receptor-ligase pair necessary for costimulation of T-helper APCs. Without this co-stimulation, presentation of the antigen to the helper T cell may lead to its functional inactivation:
2. MHC class2/CD4.
3. MHC class 1CD8.
4. MHC class2/TCR
AND. Name the receptor-ligase pair necessary for stimulation of killer T cell (CD8):
1. MHC class 2/CD4.
2. MHC class 1/CD8.
TO. Some viruses and bacterial toxins have the property of superantigens, causing nonspecific activation of lymphocytes, leading to their death. Explain the mechanism of their action.
An antigen is a substance or forms of a substance that, when it enters the body, can cause (induce) an immune response. Such substances are often called immunogens in the medical literature. The procedure for introducing an antigen into the body is called immunization.
Antigens (immunogens) are large molecules with a large molecular weight. But there are exceptions when the immune system responds to molecules that are not too large. An antigen can be obtained by binding small molecules (for example, aromatic molecules) with a large molecule (macromolecule), which will be the carrier, and the small molecule in this case is called hapten. Cases of immediate or delayed allergic reactions are often associated with haptens.

In the role antigen There can be a variety of objects containing the corresponding substances. These can be food, pollen, insecticidal, household objects, latex, dyes, xenobiotics, various types of implants, tumor cells and many other objects. By their chemical nature, antigens are proteins, polysaccharides, phospholipids and their combinations.
Antigens carry signs of foreign information. But what exactly and how does the body’s immune system recognize it? The immune system has a diverse arsenal of cellular structures to recognize and destabilize antigens. T- and B-lymphocytes play an important role in antigen identification; they are endowed with special receptors (analyzers) for antigen recognition. And with the help of these receptors, lymphocytes analyze the molecules of the outer membranes of cells and intercellular tissues of a foreign object. Originating in the organs of the immune system, lymphocytes are endowed with receptors that are initially “sharpened” to detect any type of antigen entering the body, even potentially unknown to the immune system.
The B-lymphocyte finds the antigen, absorbs and begins the process of cleaving the antigen, turning it into an antigen-presenting complex (a set of substances “digestible” for the T-lymphocyte), preparing it for presentation to the T-lymphocyte (without such preparatory work, the T-lymphocyte is not able to recognize antigen). The T-lymphocyte recognizes a prepared antigen suitable for it and begins to divide, that is, to form a clone of a similar T-lymphocyte. The number of such clones can reach several million, and each has specific receptors for the same antigen. Clones are necessary to ensure that there are enough T-lymphocyte cells for all antigen molecules. By eliminating antigen molecules, T lymphocytes recruit other phagocytes to work in order to remove antigens from the body with their help. The whole process is called humoral immune response.
Exists interesting feature The immune system builds an immune response to antigens using T lymphocytes and B lymphocytes or using only B lymphocytes. In this sense, all antigens are divided into thymus-dependent, when T- and B-lymphocytes are involved, and thymus-independent, when only B-lymphocytes are involved. Thymus-independent antigens are referred to as TH antigens.
Antibodies are the immune system's response to the presence of an antigen in the body. Antibodies are molecules of immunoglobulins, special soluble proteins. B lymphocytes are responsible for the production of antibodies. Immunoglobulins bind antigen molecules, neutralizing them. Next, by phagocytosis, the molecules are eliminated (removed) from the body. Antibodies, that is, immunoglobulins, have the unique ability to bind antigen molecules in the form in which these molecules enter the body (without pre-processing the molecule, as in the case of T lymphocytes), therefore immunoglobulins are called antigen-recognizing and antigen-binding molecules. In such cases, less time is spent on the body's immune response. Such immunoglobulins (antibodies) are involved in the immune response when we're talking about about the presence of thymus-independent antigens (TH-antigens) in the body.
This rather intricate scheme of how the immune system works when an antigen enters the body allows a person to fight harmful microorganisms and substances, ensuring his future life.
Exogenous, endogenous;
Complete and inferior (haptens, semi-haptens);
Thymus-dependent and thymus-independent;
Superantigens;
Heterogeneous;
Autoantigens;
Tumors;
Bacterial (group-specific, species-specific, type-specific, O-, K-, H-antigens and others);
Viral;
Fungal;
Protective;
Isoantigens;
Major histocompatibility complex antigens.
Exogenous antigens – enter the body from the environment, undergo endocytosis and cleavage in Ag-presenting cells (macrophages, dendritic cells of the thymus, follicular process cells of the lymph nodes and spleen, M-cells of the lymphatic follicles of the digestive tract, Langerhans cells of the skin). Then the Ag determinant (epitope), in complex with an MHC class II molecule, is inserted into the plasma membrane of the Ag-presenting cell and presented to CD 4 + T lymphocytes (T helper cells);
Endogenous antigens - products of the body's own cells. Most often, these are abnormal proteins of tumor cells and viral proteins synthesized by virus-infected host cells. Their antigenic determinants (epitopes) are presented in complex with the MHC class I molecule to CD 8 + T-lymphocytes (T-killer cells).
Full Ag – have the ability to induce the formation of antibodies and interact with them;
Defective Ag (haptens) – low-molecular substances that do not have the ability to induce the formation of antibodies and, but interact with ready-made specific antibodies. Haptens acquire the properties of full-fledged antigens when they bind to high-molecular substances, such as proteins (schleppers). Haptens include drugs, such as antibiotics, that are capable of triggering an immune response when they bind to proteins in the body (albumin) as well as proteins on the surface of cells (red blood cells, white blood cells). As a result, antibodies are formed that can interact with the hapten. When a hapten is reintroduced into the body, a secondary immune response occurs, often in the form of an allergic reaction, such as anaphylaxis;
Half-haptens – inorganic substances – iodine, bromine, chromium, nickel, nitro group, nitrogen, etc. – by binding to proteins, for example, the skin, they can cause allergic contact dermatitis (HCT), which develops when the skin comes into repeated contact with chrome-plated, nickel-plated objects, application of iodine to the skin, etc.
Thymus-dependent antigens – these are antigens that require the participation of T-lymphocytes to induce an immune response; these are the majority of antigens;
Thymus-independent – antigens that can stimulate the synthesis of antibodies without the help of T cells, for example, LPS of bacterial cell walls, high molecular weight synthetic polymers.
Superantigens (bacterial enterotoxins (staphylococcal, cholera), some viruses (rotaviruses), etc. - a special group of antigens that, in significantly lower doses than other antigens, cause polyclonal activation and proliferation of a large number of T-lymphocytes (more than 20%, whereas ordinary antigens stimulate 0.01% of T lymphocytes). This produces a lot of IL-2 and other cytokines that cause inflammation and tissue damage.
Heterogeneous Ag – these are cross-reacting Ags, common antigens in different types of microbes, animals and humans. This phenomenon is called antigenic mimicry. For example, group A hemolytic streptococci contain cross-reacting antigens (in particular, M-protein), common with antigens of the endocardium and glomeruli of human kidneys. Such bacterial antigens cause the formation of antibodies that cross-react with human cells, leading to the development of rheumatism and post-streptococcal glomerulonephritis. The causative agent of syphilis There are phospholipid antigens similar to phospholipids of the heart of humans and animals, therefore the cardiolipin antigen of the bovine heart is used to detect antibodies to Treponema pallidum in the serodiagnosis of syphilis (Wassermann reaction). Forsman antigen – detected in erythrocytes of sheep, cats, dogs, kidneys of guinea pigs, salmonella.
Autoantigens – these are endogenous antigens that cause the production of autoantibodies. There are:
- natural primary (normal tissue of the eye lens, nervous tissue, etc.), which is associated with a violation of autotolerance,
Acquired secondary - products of tissue damage by microbes, viruses, burns, radiation, cold, which arise from one’s own tissues as a result of tissue changes due to burns, frostbite, and exposure to radioactive radiation.
Tumor (oncoantigens, T-antigens ( tumor - tumor ) - as a result of malignant transformation of normal cells into tumor cells, they begin to express (manifest) specific abnormal antigens that are absent in normal cells. Detection of tumor antigens by immunological methods will make it possible to early diagnose cancer.
Bacterial antigens:
group-specific – common antigens in different species of the same genus or family,
species-specific – antigens characteristic of representatives of one species,
type-specific – determine serological variants (serovars, serotypes) within one species,
H-antigens (flagellate) – the protein flagellin, which is part of bacterial flagella, is thermolabile;
O-antigens (somatic) – is LPS of Gr-bacteria, thermostable. Epitopes of somatic antigen are represented by hexoses (galactorse, rhamnose, etc.) and amino sugars (N-acetylglucosamine, N-acetylgalactosamine). In Gr+ bacteria, the somatic antigen is represented by glyceryl teichoic and ribitol teichoic acids.
K-antigens (capsule antigens) – are located in the capsule and are associated with the surface layer of lipopolysaccharide of the cell wall. They contain acidic polysaccharides, which include galacturonic, glucuronic and iduronic acids. Capsule antigens are used to prepare vaccines against meningococci, pneumococci, and Klebsiella. However, administration of large doses of polysaccharide antigens can cause tolerance. In E. coli, the K-antigen is divided into fractions A (heat-stable), B, L (heat-labile). A type of K-antigen is the surface Vi-antigen (in Salmonella), which determines the virulence of the microbe and the persistence of the pathogen in bacterial carriers.
Antigens of bacteria are also their toxins, ribosomes, and enzymes.
Viral – a) supercapsid (protein and glycoprotein, for example hemagglutinin and neuraminidase of the influenza virus), b) capsid (protein), c) core (nucleoprotein).
Fungal – yeast-like fungi Candida albicans contain cell wall polysaccharide – mannan, cytoplasmic and nuclear proteins. Among them, 80 antigens were identified. These antigens cause immediate (antibodies Ig m, Ig G, Ig A, Ig E classes) and delayed (T-cell) reactions and sensitization without clinical manifestations. Fungal antigens have immunostimulating and immunosuppressive effects.
Protective – these are antigenic determinants (epitopes) of microorganisms that cause the most powerful immune response, which provides immunity to the corresponding pathogen during repeated infection. They were first discovered in the exudate of affected tissue during anthrax. The most immunogenic, protective peptides of viruses are used to create synthetic vaccines.
Isoantigens – antigens by which individuals of the same species differ from each other (for example, erythrocyte antigens - the ABO blood group system, Rh factor, leukocyte antigens - the major histocompatibility complex).
Major histocompatibility complex antigens – glycoproteins of cell membranes, which play an important role in the immune response, transplant rejection, and determine predisposition to certain diseases. The spectrum of molecules of the major histocompatibility complex is unique for each organism and determines its biological individuality, which makes it possible to distinguish “self” (histocompatible) from “foreign” (incompatible). The major histocompatibility complex is designated as MHC (Major Histocompability Complex). MHC antigens are designated differently in different animal species: in mice - H2 system, in dogs - DLA, in rabbits - RLA, in pigs - SLA. In humans, antigens of the major histocompatibility complex are designated HLA (Human leucocyte antigenes), since for clinical and experimental purposes leukocyte antigens are defined as antigens of the major histocompatibility complex. Human leukocyte antigens are encoded by genes localized on chromosome 6. Based on their chemical structure and functional purpose, HLA is divided into two classes.
MHC class l antigens presented on the surface of all nucleated cells. They regulate the interaction between killer T cells and target cells. The main biological role of class l antigens is that they are markers of “one’s own”. Cells carrying class I antigens are not attacked by their own T-killers due to the fact that during embryogenesis, autoreactive T-killers that recognize class I antigens on their own cells are destroyed. Class I antigens interact with the CD 8 molecule on the killer T cell membrane.
MHC class ll antigens located predominantly on the membrane of immunocompetent cells (macrophages, monocytes, B- and activated T-lymphocytes. Class II antigens interact with the CD 4 molecule of the T-helper membrane, which causes the release of lymphokines that stimulate the proliferation and maturation of T-killer cells and plasma cells.
Determination of HLA antigens is necessary in the following situations:
When typing tissues for the purpose of selecting a donor for a recipient;
To establish a connection between the presence of certain MHC antigens and predisposition to a particular disease. The most pronounced correlation was found between the presence of HLA-B27 and ankylosing spondylitis (ankylosing spondylitis): 95% of patients have this antigen.
When assessing immune status(detection of a) activated T-lymphocytes carrying HLA-DR antigens and b) mononuclear cells involved in antigen recognition.
Undoubtedly, you have heard about the concepts of antigen and antibody. But, if you are not involved in medicine or biology, then most likely you do not know about the role of antigens and antibodies. Most people have general idea about what antibodies do, but they are not aware of their crucial relationship with antigens. In this article we will look at the difference between these two formations and learn about their functions in the body.
What are the differences between antigen and antibody?
The easiest way to get a better understanding of the difference between an antigen and an antibody is to compare the two entities. They have different structures, functions and locations in the body. Some, as a rule, have positive qualities, because they protect the body, while others can cause a negative reaction.
What is it?
An antigen is a foreign particle that can trigger an immune response in the human body. They are mainly composed of proteins, but they can also be nucleic acids, carbohydrates or lipids. Antigens are also known as immunogens. These include chemical compounds, pollen, viruses, bacteria and other substances of biological origin.
Antibodies may be called immunoglobulins. These are proteins synthesized by the body. Their products are necessary to combat antigens.
What are the types and functions of antigen and antibody?
All antigens are divided into external and internal. Self-antigens, such as cancer cells, are formed inside the body. External antigens enter the body from the external environment. They stimulate the immune system to produce more antibodies that protect the body from various types of damage.
There are only 5 different types of antibodies. These are IgA, IgE, IgG, IgM and IgD.
IgA protects the body surface from external substances.
IgE causes defensive reaction in the body against foreign substances, including animal origin, plant pollen and fungal spores. These antibodies are part of allergic reactions to certain poisons and medications. Those with allergies tend to have large amounts of this type of antibody.
IgG plays a key role in fighting bacterial or viral nature. These are the only antibodies that are able to penetrate the placenta of a pregnant woman, providing protection to the fetus while still in the womb.
When an infection develops, IgM antibodies are the very first type of antibodies that are produced in the body as an immune response. They will lead to other immune system cells destroying foreign substances.
Scientists are still not clear what exactly IgD antibodies do.
Where can they be found antigen and antibody?
Another difference between antigen and antibody is where they are located. Antigens are like “hooks” on the surface of cells and are found in almost every cell.
You can find IgA antibodies in the vagina, eyes, ears, digestive tract, respiratory passages and nose, as well as in blood, tears and saliva. Approximately 10-15% of antibodies in the body are IgA. There are a small number of people who do not synthesize IgA antibodies.
IgD antibodies can be found in small quantities in the fatty tissue of the chest or abdomen.
You will find IgE antibodies in the mucous membranes, skin and lungs.
IgG antibodies are found in all body fluids. They are the most abundant and smallest antibodies in the body.
IgM antibodies are the largest antibodies and can be found in lymph fluid and blood. They make up 5-10% of the antibodies in the body.
How antigens and antibodies work: immune response
To better understand the difference between antigen and antibody, it helps to understand the immune response. All healthy adults have thousands of different antibodies in small amounts throughout the body. Each antibody is highly specialized, recognizing a single type of foreign substance. Most antibody molecules are Y-shaped, with a binding site along each arm. Each binding site has a specific shape and will only accept antigens with the same shape. Antibodies are designed to bind to antigens. When they bind, they render antigens inactive, allowing other processes in the body to take up foreign substances, removing and destroying them.
The first time a foreign substance enters the body, you may experience symptoms of illness. This occurs when the immune system creates antibodies that will fight the foreign substance. In the future, when the same antigen attacks the body again, immune memory is stimulated. This results in the immediate production of large amounts of the antibodies that were created in the first attack. A quick response to further attacks means you may no longer experience any symptoms of the disease or even know that you were exposed to the antigen. This is why most people do not get diseases like chickenpox again.
From the above difference between antigen and antibody, antibody testing can provide the doctor with useful information during the diagnostic process.
Your doctor may test your blood for antibodies for a number of reasons, including:
- diagnosis of allergies or autoimmune diseases
- identification of a current infection or one of the past infections
- diagnosis of recurrent infections, causes of relapses due to low levels of IgG antibodies or other immunoglobulins
- testing an immunization response as a way to make sure you are still immune to a particular disease
- diagnosing the effectiveness of treatment for various types of cancer, especially those that affect the human bone marrow
- Diagnosis of specific types of cancer, including macroglobulinemia or multiple myeloma.
Read more:
Long-term low-grade fever: causes and treatment
Leukopenia: causes, symptoms, treatment
What is the difference between innate and acquired immunity?
In the body, when an immune response occurs, antibodies and antigens interact. However, under certain conditions, the latter can cause a state of so-called specific irresponsibility - tolerance. Antibodies and antigens contribute to the formation of immunological memory. Next we will consider the second type of substances. In this article we will find out what an antigen is.
General information
What is an antigen? Simply put, these are usually foreign compounds. These include polysaccharides, proteins and their complexes. When altered through chemical modification, "conjugated" substances can be obtained. Such compounds can be formed on the basis of proteins that belong directly to the recipient itself. An autologous substance denatured by chemical or physical means can also be converted into an antigen.
Definition
Biopolymers or their synthetic analogues can enter the body and cause an immune response. These compounds are called antigens. They promote the production of thymic effector cells. Antibodies that appear against the background of an immune reaction begin to interact in a specific way with antigens or chemical compounds that have a similar structure. If the latter do not provoke a protective response, then they are called haptens. They are the ones who provoke immunological tolerance. Synthetic polypeptides have the ability to cause a protective reaction, acting as protein antigens. However, their primary and spatial structure does not necessarily have to be similar to that of any particular protein compound. An essential factor in the manifestation of antigenic properties in these substances is the formation of a stable spatial structure. In this regard, polymers formed from a single amino acid (homopolymers) do not have the properties to induce an immune response. Antigenic abilities appear in polypeptides, the formation of which involves 2 amino acids.

Research Questions
What is an antigen? Classical immunology calls a whole cell of animal or bacterial origin such a substance. However, this is not true from a chemical point of view. It is said above what an antigen essentially is. This is not a cell in which there are a large number of nucleic acids, proteins, and polysaccharides. Human antigens obtained in purified form can be used to induce an immune response. Moreover, it will be specific to a particular biopolymer. Considering the purified structure as an individual antigen, any combination of them must be described as a family of individual compounds. This term can be used to refer to a specific biopolymer that spontaneously aggregates. An example is some antigens of viruses or bacteria. Thus, flagellin can be found in both polymerized and monomeric forms on the flagella of gram-negative microorganisms of the genus Salmonella. In both cases, this antigen can induce the formation of antibodies, although the conditions for this are different. In particular, the phelagelin polymer is thymus-independent, while the monomer is thymus-dependent.

Relationship to molecular weight
It can only be established by comparing substances of the same class. For example, this applies to various proteins with the same type of tertiary and secondary structures: fibrillar and globular. In such cases, a direct relationship can be established between the ability of a polymer to induce antibody formation and its molecular weight. This pattern, however, is not absolute. Among other things, it depends on other properties of the compound, both chemical and biological.
Degree of manifestation of properties
The severity of the antigenic characteristics of proteins, which act as the most extensive and significant class, will depend on the degree of evolutionary distance between the donor from whom the compound was received and the recipient to whom it is administered. It will be correct only if substances of the same type are used in the assessment. For example, if mice are immunized with rat and human serum albumin, the first response will be more pronounced. If a biopolymer is characterized by increased sensitivity to splitting, then its properties will be less pronounced than those of a substance exhibiting greater durability To enzymatic hydrolysis. Thus, in the case of using synthetic polypeptides or protein conjugates as antigens, the response to a substance that contains unnatural D-amino acids will be more pronounced. Decisive role in the manifestation of the immune response is attributed to the genotype of the recipient.

Determinant groups
They denote molecular regions of a biopolymer, its synthetic analogue or conjugated antigen, which are recognized by antigen-binding B-lymphocyte receptors and antibodies. The molecule usually contains several determinant groups, different in structure. Each of them can be repeated several times. If there is only one group with a certain structure in the compound molecule, antibodies will not be formed against it. As identical complexes increase, the immune response to them will also increase. However, this process will continue until certain point, after which it will decrease and may not be observed at all subsequently. This phenomenon was studied in the process of using conjugated antigens with different numbers of substituents that performed the task of a determinant group. The absence of an immune response to biopolymers with increased epitope density is due to the mechanism of activation of B-group lymphocytes.

Carcinoembryonic antigen
It is a type of normal tissue protein that is produced in small amounts by the cells of some organs in healthy people. CEA in its chemical structure is a combination of carbohydrates and protein. Its purpose in adults is unknown. However, during the period of intrauterine formation, it is quite intensively synthesized by the organs of the digestive system, while performing quite important tasks. They are associated with stimulation of cell reproduction. Carcinoembryonic antigen is detected in the tissues of the digestive organs, but in fairly small quantities. The name of this tumor marker partly characterizes its biological nature, but for the most part it still has properties that are valuable in laboratory research. The term “embryonic” has a connection with physiological tasks during development in the prenatal period, “antigen” indicates the possibility of identifying it in biological environments using an immunochemical binding method. However, it does not exhibit any properties directly in the body. Normally, in a healthy body, the concentration of CEA is quite low. Against the background of the oncological process, its level increases quite sharply, reaching quite high levels. In this regard, it is characterized as a tissue marker of oncological pathologies, or tumor marker.

REA level
Antigen testing is used in the diagnosis of various malignant neoplasms, mainly rectal and colon cancer. The study is carried out in the early stages of pathologies, in the process of monitoring the course of the disease and monitoring the effectiveness of therapeutic measures. Against the background of colon and rectal cancer, the test has the highest sensitivity. This is what allows it to be used in primary diagnosis. After successful surgery to remove all tumor tissue, the CEA concentration returns to normal after a maximum of two months. Regular tests subsequently allow the patient's condition to be assessed after they have received treatment. Detection of high levels of CEA allows for timely detection of relapse of pathology. When the antigen content decreases during therapy, experts draw a conclusion about the effectiveness of the therapeutic effect.
Increased concentration of CEA: range of pathologies
However, the test is not considered absolutely specific for tumors. An increase in the level of CEA may be observed against the background various diseases internal organs of inflammatory and other nature. In 20-50% of patients with benign pathologies of the pancreas, intestines, lungs and liver, the antigen concentration increases slightly. The same is observed against the background of cirrhosis, chronic hepatitis, ulcerative colitis, cystic fibrosis, emphysema, bronchitis, Crohn's disease, pancreatitis, pneumonia, autoimmune diseases, tuberculosis. In addition, an increase in level may not be caused by a disease, but, for example, by regular drinking or smoking.

Features of blood transfusion
The main one is the specificity and individuality that erythrocyte antigens possess. If the biopolymers of the recipient and the donor are incompatible, it is strictly prohibited. Otherwise, pathological processes and even the death of the patient are inevitable. In immunogenetics, methods are used to test and study erythrocyte antigens. These include, in particular, hemolysis, precipitation, and agglutination reactions. Erythrocyte genes are presented in the form of complex biopolymer macromolecules. They accumulate on the stroma (sheath) and combine with other compound molecules. Each individual has an individual chemical composition and its own structure.