Poisoning is the body's response to inhalation, penetration through mucous membranes or skin, or ingestion of chemicals. It is considered in the form of a chemical injury, which develops as a result of a toxic dose of foreign chemicals entering the body.
First aid for poisons penetrating the skin
With this type of poisoning, it is necessary to undress the victim as soon as possible and wash the areas of skin that have been exposed to foreign chemicals with a large volume of water. This must be done very carefully so that the chemicals do not get on your skin, it is better to do this with rubber gloves. The person must be positioned so that the water drains and does not fall on clean areas of his skin. To provide assistance in case of chemical poisoning, you must immediately call an ambulance, until which arrives you must monitor the breathing and heartbeat of the victim, and, if necessary, perform resuscitation.
Help with chemicals getting into the lungs
The first thing to do is dial the ambulance number, informing that the victim may need oxygen. First of all, you need to remove the person from the area affected by volatile substances, to fresh air. Clear the trachea and other airways if necessary, and place the person in a position in which he will not harm himself. You should not give him anything to drink or eat, as food may get into the respiratory tract and the person may suffocate.
If a person is unconscious, you need to lay him on his side so that he does not choke on stomach contents in case of vomiting. Relax the airways, if necessary, tear the clothes. Examine the person. If he has no pulse or breathing, assistance must be provided in the form of chest compressions and artificial respiration.
Penetration of chemicals through the stomach, first aid
The very first aid for chemical poisoning by substances that enter the body through the mouth is gastric lavage. To do this, let the person drink as much as possible more water, in small sips, preferably salted (2 tablespoons of salt per liter of water). Only a conscious person can rinse the stomach. After this you need to induce vomiting. To induce vomiting, press your finger on the root of your tongue.
After gastric lavage, it is necessary to drink a bitter laxative to further flush out toxins from the victim’s body. After this, you can give some kind of sorbent (for example, activated carbon).
Before the ambulance arrives, you need to monitor the victim’s blood circulation and breathing. If the victim is not breathing, it is necessary to artificial respiration And indirect massage hearts. If convulsions are observed, you need to protect the person - loosen his clothes, remove potentially dangerous objects. You can roll up a rope of fabric and force a person to bite it with his teeth so that he does not bite his tongue.
Modern man uses a lot of things every day various means household chemicals, which are so effective and make life so much easier that sometimes we forget about the dangers and do not follow the rules for using and storing these substances. Neglecting the recommendations of the manufacturer of the washing powder or gel may pose a serious threat to the health of family members, especially children. It is better to know in advance what to do in such a situation.
Types of household chemicals hazardous to health:
- cosmetics (colognes, lotions) containing various alcohols (butyl, amyl, ethyl). Ingestion of such drugs causes severe alcohol poisoning, dizziness, vomiting, breathing problems and heart palpitations;
- acids (hydrochloric, acetic, carbolic, oxalic, hydrofluoric). These substances are found in bathtub and toilet cleaners, rust stain removers, and brake fluid. Such drugs can cause serious burns to the skin and mucous membrane, even burning the walls of the stomach;
- alkalis ( ammonia, caustic soda, persol), cause poisoning;
- products containing FOS (organophosphorus compounds). These are mainly insecticides (dichlorvos, chlorophos) and repellents that can be poisonous to humans;
- solvents (turpentine, acetone);
- foaming liquids (shampoo, dishwashing liquid);
- products that contain chlorinated hydrocarbons (used to remove grease stains) that damage the kidneys and liver.
- If a household chemical product is in a prominent place, then it is very likely that a small child will want to taste the bright liquid from a beautiful bottle. However, adults can mistakenly take a sip of vinegar essence instead of water. If powders are handled carelessly, there are frequent cases of them getting into the respiratory tract.
Symptoms of poisoning from household chemicals
Poisoning with household chemicals may be accompanied by the following symptoms:
- dizziness, nausea and vomiting;
- pain from chemical burn in the larynx, esophagus, stomach or respiratory tract;
- foam at the mouth;
- convulsions;
- coughing and choking;
- loss of self-control or loss of consciousness.
Why you can’t treat poisoning with traditional methods
Our grandmothers treated food poisoning using simple folk methods:
- gave the patient a solution of potassium permanganate;
- gave activated carbon;
- caused vomiting;
- washed the stomach with an enema.
In case of poisoning from household chemicals, the above treatment methods are usually not suitable. Potassium permanganate (potassium permanganate) is a strong oxidizing agent. If the powder does not dissolve well in water and the whole crystal gets into the stomach (the mucous membrane of which is already burned), potassium permanganate will further injure the mucous membrane.
Activated carbon is an excellent remedy for minor digestive problems and mild food poisoning. In serious cases, when a person has swallowed a caustic or foaming liquid, activated carbon in the usual dosage (1 tablet per 10 kg of the patient’s weight) is useless. In order for the medicine to absorb the chemicals that have entered the stomach, one would have to take charcoal at the rate of 1 tablet per kilogram of the poisoned person’s weight. For a person with a burned larynx, this would be torture. In addition, in many cases, the victim should not take anything by mouth until examined by a doctor.
It is impossible to induce vomiting if the patient has drunk a scalding liquid: the vomit, passing through the esophagus in the opposite direction, will only burn the mucous membrane even more and can injure the respiratory tract. If a foaming gel gets into the stomach, then with artificial stimulation of vomiting, the foam can clog the airways and cause suffocation.
Experts do not recommend gastric lavage with an enema. In this case, the caustic liquid from the stomach will enter the small intestine and is quickly absorbed into the blood, at the same time injuring the mucous membrane of its walls. Doctors perform gastric lavage using a special tube.
Providing first aid for poisoning of household chemicals
First of all, you need to call an ambulance, explaining in detail to the dispatcher how the person was poisoned. The packaging from the drink should be saved and given to a toxicologist.
The poisoned person must be removed from the room filled with vapors of a toxic chemical. A person who has burned their respiratory tract with toxic vapors or powder should rinse their mouth with running water.
If a toxic substance has entered the stomach, but the patient is conscious, he is placed on his stomach and his head is turned so that in case of vomiting he does not accidentally inhale the vomit and burn the respiratory tract. For a patient who has lost consciousness, the mouth is opened slightly and the lower jaw is pushed forward a little so that he does not suffocate. If a person has removable dentures or braces, they should be removed from the mouth to prevent them from oxidizing due to the caustic liquid.
The patient should thoroughly rinse his mouth several times (preferably with running water): particles of household chemicals linger on the tongue and palate, and you need to try to prevent any remaining poison from entering the stomach.
If caustic liquid gets into your eyes, they must be washed out. Lips, chin, and other areas of the body that have been in contact with acid or alkali should be kept in cold running water for at least 20 minutes. The only exceptions are hydrofluoric acid and quicklime. The area of skin burned with hydrofluoric acid should be carefully blotted with a dry cloth (do not rub or smear the substance under any circumstances), and then keep the burn area in cold running water for 20 minutes. The burn from quicklime is not moistened, but, after blotting with a dry cloth, is lubricated with glycerin.
You should not give the patient anything to drink if:
- he was poisoned by the foaming liquid;
- his stomach hurts (that is, there may be a perforation).
In other cases, the patient should drink 2-3 glasses of water so that the concentration of caustic liquid in the stomach decreases. Egg white coats well the walls of the stomach and stops the absorption of poison into the blood in case of acid poisoning. For the same purpose, the patient can drink a glass of milk.
It is not recommended to try to carry out a neutralization reaction in the victim’s stomach on your own: if he drank acid, give him soda, if he drank alkali, give him a solution of vinegar. To do this, you need to know chemistry well, and any mistake will only worsen the condition.
To avoid poisoning, all household chemicals must be stored in their original packaging, in specially designated places that children and pets do not have access to.
May 22, 2017 Views: 19032
What is Chemical Poisoning
Chemical poisoning is a condition caused by the ingestion of a toxic substance/poison into gastrointestinal tract and respiratory tract or upon contact with skin, eyes, mucous membranes of the mouth, nose, etc.
Toxic substances/poisons include some medicines, substances used in household, solvents, pesticides and other chemicals.
When poisoning with chemicals, symptoms can vary, because toxins affect different systems.
The main symptoms of chemical poisoning:
nausea, vomiting
cold sweat
·chills
·convulsions
Breathing disorders: shortness of breath, suffocation
increased heart rate or cardiac arrest
sudden lethargy
·drowsiness
·stomach ache
headache and dizziness
drooling and/or lacrimation
burns around the lips, on the tongue or on the skin
strange behavior of the victim
$1· constriction or dilation of the pupils (miosis and mydriasis).
Each class of substances is characterized by effects on certain organs and systems, so the signs of poisoning by chemicals are specific.
Thus, when toxic substances enter through the lungs, coughing, mucus discharge from the nose, sputum discharge, bronchospasm and the inability to exhale are possible. Also possible toxic edema lungs. If the poison enters the gastrointestinal tract, then in case of chemical poisoning, symptoms may include abdominal pain, heartburn, and vomiting.
First aid for poisoning:
- Stop or limit the flow of poison into the body.
- Remove the poison that has already entered the body as soon as possible, if possible.
- Provide the victim with a safe environment.
- Bring the victim to his senses, if necessary, carry outartificial respiration and indirect cardiac massage.
- Take the victim to a hospital as soon as possible hospital
First aid can be provided both by strangers and by the victims themselves. It often turns out that timely first aid in the treatment of poisoning helps save lives. According to statistics, in the vast majority of cases household poisoning account for 97-98%, while production is only 2-3%.
Household poisonings are divided into alcohol poisonings intoxication , domestic accidents and suicidal poisonings undertaken intentionally.
It largely depends on how the poison entered the body, as well as on the patient’s condition. first aid and treatment of poisoning.
What to do in case of poisoning depending on the route of entry of the poison
In case of poisoning alcohol, poor quality food, mushrooms, poisonous plants and their fruits, When poison enters the body through the mouth, the victim, if he is conscious, is given a large amount of liquid to drink and vomiting is induced by pressing on the root of the tongue (for persons over 6 years old) with fingers. The procedure is repeated until the wash water is clear.
After washing stomach You can give crushed activated carbon (1 tablet per 10 kg of weight), smect and other sorbents.
The victim is placed in a recovery position - on his side (so that he does not choke vomiting masses), warm the legs using heating pads. Give plenty of fluids. Tea and water are suitable for this.
You need to call an ambulance as soon as possible medical care for hospitalization of the victim, as his condition may worsen. It is advisable to save and pass on doctor substance that poisoned the patient.
In case of poisoning with acids (vinegar) and alkalis
You can’t wash your stomach!
In case of poisoning with gaseous chemicals (carbon monoxide, oxides of nitrogen, ammonia, bromine vapor, hydrogen fluoride, chlorine, sulfur dioxide, etc..), When the poison enters the body through the lungs, The victim must first be taken out into fresh air, provided with a comfortable horizontal position, and freed from restrictive clothing.
It is necessary to rub the victim’s body with your palms to improve blood circulation, then wrap him warmly, apply warming pads to his legs, let him sniff cotton wool with ammonia, if the victim is conscious, you can rinse his throat and mouth with a soda solution. In case of absence of breathing or its significant weakening, artificial respiration should be started.
Regardless of the degree of poisoning, the victim is hospitalized in a hospital in case complications from the nervous and respiratory systems arise later;
In case of poisoning with toxic substances (some poisonous plants, chemical solvents and insect repellents - organophosphorus compounds (karbofos, dichlorvos, etc.), when the poison enters the body through the skin you need to remove this substance from the surface of the skin as quickly as possible with a cotton or gauze swab, being careful not to smear it on the surface of the skin.
After this, the skin should be washed thoroughly warm water with soap or a weak solution of drinking (baking) soda, treat the affected area on the skin with a 5-10% solution of ammonia. Subject to availability wounds such as a burn, apply a clean or sterile, moist bandage. Next, rinse the stomach twice with a 2% solution of baking soda (1 teaspoon of baking soda per 1 glass of water).
Then you should drink 0.5 cups of a 2% solution of baking soda with the addition of activated carbon or a saline laxative. The victim is given strong tea to drink. Wait for the ambulance team to arrive.
If a toxic substance gets into your eyes, rinse them immediately with a stream of water with your eyelids open. Rinsing should be thorough for 20-30 minutes, since even a small amount of a toxic substance that gets into the eyes can cause them deep lesions. After rinsing the eyes, apply a dry bandage and immediately contact eye doctor.
Chemical poisoning
What is Chemical Poisoning -
Poisoning- totality adverse effects caused by the entry of a toxic substance into the gastrointestinal tract and respiratory tract or its contact with the skin, eyes or mucous membranes (orb, vagina, etc.).
What provokes / Causes of Chemical poisoning:
Poisons include some medications, household substances, solvents, pesticides and other chemicals.
Symptoms of Chemical Poisoning:
Symptoms of poisoning depend on the type and amount of poison ingested and the individual characteristics of the victim. Some poisons with low toxicity cause certain problems only with prolonged exposure or repeated exposure to the body. large quantities. Other substances are so poisonous that even one drop of such poison getting on the skin can lead to dire consequences. The toxicity of a substance in each specific case also depends on the genetic characteristics of the person. Some normally non-toxic substances are toxic to people with a certain genotype (set of genes).
The dose of the substance causing symptoms poisoning is also very dependent on age. For example, ingesting more paracetamol in a small child is more likely to cause symptoms of poisoning than the same dose in an adult. For an elderly person, a sedative from the group of benzodiazepines (seduxen, Relanium, phenazepam) can be toxic in doses that do not cause any problems in a middle-aged person.
Symptoms of poisoning can be minor but unpleasant, such as itching, dry mouth, blurred vision, pain, or they can be life-threatening, such as confusion, coma, abnormal heart rhythm, difficulty breathing and severe agitation. Some poisons take effect within seconds, while others take several hours or even days to take effect.
There are poisons that do not cause obvious symptoms until there is irreversible damage to the function of vital organs, in particular the liver or kidneys. Thus, the symptoms of poisoning are as countless as the number of poisons.
Diagnosis of Chemical Poisoning:
Optimal management of patients with poisoning requires a correct diagnosis. Although the toxic effects of some chemicals are very characteristic features, most of the syndromes observed during poisoning can be caused by other diseases.
Poisoning usually includes differential diagnosis coma, seizures, acute psychosis, acute hepatic or renal failure and bone marrow suppression. Although this should be done, the possibility of poisoning can be discounted when the patient's main symptoms are mild mental or neurological impairment, abdominal pain, bleeding, fever, hypotension, pulmonary congestion, or skin rash. In addition, the patient may not be aware of the effects of the poison on him, as is the case with chronic, latent poisoning, or after an attempt at suicide or abortion, the patient will also be reluctant to agree with such a diagnosis. Physicians should always be aware of the various manifestations of poisoning and maintain a high degree of vigilance in relation to them.
In all cases of poisoning, an attempt should be made to identify the toxic agent. It is obvious that without such identification it is impossible to carry out specific therapy with antidotes. In cases of murder, suicide or criminal abortion, the determination of poison may have legal meaning. In cases where poisoning is the result of industrial exposures or therapeutic error, accurate knowledge of the active agents is necessary to prevent similar occurrences in the future.
In case of acute accidental poisoning, the active substance may be known to the patient. In many other cases, information can be obtained from relatives or friends, by examining containers located at the site of poisoning, or by interviewing the patient’s attending physician or his pharmacist. Often such actions allow you to install only trade name product, which does not allow one to know its chemical composition. The bibliography at the end of this chapter lists a number of books that list the active constituents of substances used in household, agricultural, patent medicines and poisonous plants. Every doctor should carry a small reference book of this type in his briefcase. The latest information of this kind can also be obtained from Poison Treatment Centers and from representatives of manufacturers of these substances. In case of chronic poisoning, it is often impossible to quickly determine the toxic agent based on medical history. Less urgency therapeutic measures in these cases it usually allows for the necessary thorough examination of the patient's habits and condition environment.
Some poisons can cause the development of characteristic clinical signs, sufficient for strong assumptions about accurate diagnosis. Upon careful examination of the patient, a characteristic odor of cyanide can be detected; cherry staining skin and mucous membranes, revealing the presence of carboxyhemoglobin; constriction of the pupil, drooling and gastrointestinal hyperactivity caused by insecticides containing cholinesterase inhibitors; lead rim and extensor muscle paralysis characteristic of chronic lead poisoning. Unfortunately, these typical signs are not always present and in case of chemical poisoning their presence is rather an exception.
Chemical analysis of body fluids provides the most correct determination of the substance that caused the poisoning. Some common poisons, such as acetylsalicylic acid (aspirin) and barbiturates, can be identified and even quantified using relatively simple laboratory tests. Detection of other poisons requires more complex toxicological tests, such as high-performance gas or liquid chromatography, which are carried out only in specialized laboratories. In addition, the results of toxicological studies are rarely available in a timely manner to address the issue of initial treatment in case of acute poisoning. However, samples of vomit, gastric aspirate, blood, urine, and stool should be reserved for toxicology testing if diagnostic or legal questions arise. Chemical analysis of body fluids or tissues is especially important in diagnosis and severity assessment chronic poisoning. Ultimately, the results of such analyzes are useful for assessing the long-term results of certain types of therapy.
Treatment of Chemical Poisoning:
For proper treatment a patient with poisoning needs to know both the basic principles of managing such patients and the details of therapy for specific poisonings. The treatment process includes:
- prevention of further absorption of poison;
- removal of absorbed poison from the body;
- symptomatic maintenance therapy or symptomatic treatment for circulatory, respiratory disorders, neurological disorders and renal dysfunction;
- introduction of systemic antidotes.
The first three steps apply to most types of poisoning. The fourth stage is most often used only when the toxic agent is known and a specific antidote is available. However, sometimes, if there is a high degree of suspicion that the patient is overdosing on opiates, he is given naloxone. It should be realized that for most poisons there are no specific antidotes, and to carry out the necessary maintenance therapy it is not necessary to know which toxic agent caused the poisoning. Thus, although the physician should always attempt to identify the active poison, these attempts should not delay life-saving therapeutic measures. .
Prevention of absorption of ingested poisons. If a significant amount of poison has been ingested, an attempt should be made to minimize its absorption from the gastrointestinal tract. The success of such attempts depends on the time elapsed after ingestion of the poison and on the site and speed of absorption.
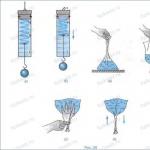
- Evacuation of stomach contents
Always, unless there are specific contraindications, you should try to empty the stomach. These attempts can be very successful if done soon after the poison is ingested. Significant amounts of poison may still be cleared from the stomach several hours after ingestion because emptying may be delayed by gastric atony or pylorospasm. This occurs in poisoning with phenothiazines, antihistamines and tricyclic antidepressants.
After swallowing many poisons, vomiting occurs spontaneously. In a minority of cases, it can be induced at home by mechanical irritation of the back of the throat. The emetic effect of ipecac syrup (the concentration should not exceed 14 times the concentration of the liquid extract), given in a dose of 15 - 30 ml, is more effective and safe even at home. Its action begins on average 20 minutes after administration and depends partly on absorption in the gastrointestinal tract, so simultaneous administration of activated carbon, which is an adsorbent, should be avoided. A second dose of ipecac syrup should be given to the patient if he does not vomit 20 minutes after taking the first dose (after taking two doses, vomiting will develop in 90-95% of patients). If ipecac syrup is not available, every effort should be made to find it, even if this means taking the patient to the hospital. Apomorphine, administered intramuscularly at a dose of 0.06 mg/kg, acts within 5 minutes, but can cause prolonged vomiting. At intravenous administration At a dose of 0.01 mg/kg, apomorphine causes vomiting almost immediately, with no further effects on the central nervous system subsequently observed. Sometimes it may not be possible to induce vomiting and valuable time should not be wasted waiting. Attempting to induce vomiting should not be attempted in victims who are convulsive, in patients with severe central nervous system depression, or (due to the risk of gastric or esophageal perforation or because of aspiration of vomit into the trachea) in those who have ingested a potent, caustic chemical. or small quantities (less than 100 ml) of liquid hydrocarbons that are strong lung irritants (eg, kerosene, polish).
Compared to vomiting, gastric lavage is preferable and has an immediate effect, but it usually does not remove poison from the stomach more effectively than vomiting. It can be performed in unconscious patients; evacuation of the stomach contents reduces the risk of aspiration of vomit. Its implementation, however, is contraindicated after ingestion of strong corrosive substances, due to the risk of perforation of damaged tissue. At correct execution Gastric lavage carries a small risk of aspiration of stomach contents into the lungs. The patient should lie on his stomach with his head and shoulders bowed. Using a mouth dilator, a gastric tube is inserted into the stomach, the diameter of which is sufficient to pass solid particles (30 gauge). If the functions of the central nervous system are depressed, if the insertion of the tube causes vomiting, or if a substance that is a lung irritant has been swallowed, then before performing gastric lavage it is reasonable to insert an endotracheal tube with a cuff into the trachea. The contents of the stomach are aspirated with a large syringe, and with it most of the poison is removed from the body. After this, 200 ml (less in children) of warm water or liquid solution and suction until the aspirated liquid becomes clear.
Interference with absorption in the gastrointestinal tract.
Since neither vomiting nor gastric lavage completely empties the stomach, an attempt should be made to reduce absorption by introducing substances that bind toxins that have entered the body. Many poisons are adsorbed by powdered activated carbon. High quality activated carbon can adsorb 50% of the mass of many common poisons. Liquid activated carbon (20-50 g in 100 * 200 ml) should be administered after gastric emptying.
Adsorption by activated carbon is a reversible process and the adsorption efficiency of many poisons varies depending on the pH value. Acidic substances are adsorbed better solutions acids and can therefore be released in the small intestine. It is desirable that the activated charcoal with the adsorbed poison pass through the intestine as quickly as possible. This will also reduce the intestinal absorption of any unabsorbed poison that passes through the pylorus. In patients with good renal and cardiac function, this is best achieved by oral or intramuscular injection osmotic laxatives such as magnesia or sodium sulfate (10 - 30 g in a solution with a concentration of 10% or less).
Prevention of absorption of poison from other organs and systems. Most topically applied poisons can be removed from the body by abundant rinsing with water. In certain cases, weak acids or alkalis or alcohol in combination with soap are more effective, but rapid and copious rinsing with water must be carried out until these solutions are available to doctors. Chemical antidotes are dangerous because the heat generated during chemical reaction, may cause tissue damage.
The systemic distribution of injected venoms can be slowed by applying a cold compress or ice to the injection site or by applying a tourniquet proximal to the injection site.
After inhalation of toxic gases, vapors or dust, it is necessary to remove the victim to clean air and maintain adequate ventilation. The patient cannot move and must wear a protective mask.
Removing absorbed poison from the body. In contrast to preventing or slowing absorption, measures that accelerate the elimination of the toxic agent and the body rarely have a major effect on the peak concentration of the poison in the body. However, they can significantly reduce the time during which the concentration of many poisons remains above a certain level, and thereby reduce the risk of complications and the death of the patient. When assessing the need to carry out such measures, it is necessary to take into account the clinical condition of the patient, the properties and pathways of metabolism of the poison and the amount of absorbed poison based on medical history and the results of determining its concentration in the blood. The administration of some poisons can be accelerated various methods; The choice of method depends on the condition of the patient, the amount of poison in the body and the availability of experienced personnel and equipment.
- Bile excretion
Certain organic acids and active drugs are secreted into bile in a direction opposite to the large concentration gradient. This process takes some time and cannot be accelerated. However, the absorption in the intestine of substances already secreted into bile, such as glutethimide, can be reduced by introducing activated carbon every 6 hours. The organochlorine pesticide - chlordenone - is slowly eliminated from the body (half-life from the blood is 165 days). Cholestyramine (16 g per day) significantly accelerates its elimination (half-life from the blood is 80 days).
- Urine excretion
Acceleration of renal excretion is justified in cases of poisoning much a large number poisons Renal excretion of toxic substances depends on glomerular filtration, active tubular secretion and passive tubular resorption. The first two of these processes can be protected by maintaining adequate circulation and kidney function, but as a practical matter they cannot be accelerated. On the other hand, passive tubular resorption of many poisons plays a role important role in increasing the period of their action and it can often be reduced by easily accessible methods. In case of poisoning with drugs such as salicylic acid preparations and long-acting barbiturates, increased diuresis induced by the administration of large volumes of electrolyte solutions in combination with intravenous furosemide has been demonstrated to enhance renal excretion.
A change in urine pH can also inhibit the passive reversible diffusion of some poisons and increase their renal clearance. The renal tubular epithelium is more permeable to uncharged particles than to ionized solutions. Weak organic acids and bases diffuse easily from the tubular fluid in their non-ionized form, but are retained in the tubules if they are ionized. Acidic poisons are ionized only at a pH higher than their pK. Alkalinization of urine sharply increases the ionization of organic acids such as phenobarbital and salicylate in the tubular fluid. In contrast, the pK values of pentobarbital (8.1) and secobarbital (8.0) are so high that renal clearance does not increase appreciably as urine pH increases within the physiological alkaline range. Alkalinization of urine is achieved by infusion of sodium bicarbonate at a rate determined by the pH value of urine and blood. The development of severe systemic alkalosis or electrolyte imbalance should be avoided. The combination of controlled diuresis with urine alkalinization can increase the renal clearance of some acid poisons by 10-fold or more, and these measures have been found to be very effective in poisoning with salicylates, phenobarbital, and 2,4-dichlorophenoxyacetic acid. Conversely, lowering the pH value below its normal values has been shown to increase the clearance of amphetamines, phencyclidines, fenfluramine and quinine.
In conclusion, it should be noted that the renal excretion of certain poisons can be increased by highly specific methods. An example of this is the removal of bromide from the body through the administration of chloride and chloruretics. These methods are discussed when considering individual poisons.
- Dialysis and hemosorption
Dialysis has been found to be effective in removing many substances from the body, including barbiturates, borate, chlorate, ethanol, glycols, methanol, salicylates, sulfonamides, theophylline, and thiocyanate. Theoretically, it should accelerate the elimination from the body of any dialyzable toxin that is not irreversibly bound to tissues. Its effectiveness does not apply to large molecules, non-dialyzable poisons and is reduced to a large extent by the binding of the toxic substance to proteins or its solubility in fats.
Peritoneal dialysis can be easily performed in any hospital and can be done over a long period of time. However, performing it for the purpose of removing poisons from the body is justified only if the patient has impaired renal function, hemodialysis or hemosorption is impossible, or forced diuresis cannot be used.
Hemodialysis is undoubtedly more effective in terms of elimination from the body large quantities dialyzable poisons. For barbiturates, dialysis rates of 50 - 100 ml/min have been achieved, while the rate of their elimination from the body is 2 - 10 times higher than with peritoneal dialysis or forced diuresis. When blood is perfused through activated carbon or ion exchange resin, even greater rates of clearance of most poisons are achieved than with hemodialysis. It is clear that extracorporeal dialysis and hemosorption may be considered the procedures of choice for the rapid removal of poisons from the body of patients who have absorbed quantities of poison that make it unlikely that they will survive even with the best supportive care provided. Since the equipment and experienced personnel necessary for hemodialysis and hemosorption are not available in every hospital, the possibility of transferring such patients to a facility that has such capabilities should be considered.
Complexation and chemical bonding. The elimination of some poisons from the body is accelerated by chemical interaction. actions with other substances followed by excretion through the kidneys. These substances are considered systemic antidotes and are discussed when considering individual poisons.
Maintenance therapy. Most chemical poisonings are reversible, self-limiting disease states. Skilful supportive care can save the lives of many severely poisoned patients and keep their detoxifying and excretory mechanisms functioning until the poison concentration is reduced to safe levels. Symptomatic measures are especially important when the active poison belongs to the category of substances for which a specific antidote is unknown. Even when an antidote is available, the possibility of life-threatening impairment should be prevented. important functions or control them with appropriate supportive care.
A patient with poisoning may suffer from various physiological disorders. Most of them are not specific to chemical poisoning and the management of such patients is discussed in other sections. This section briefly discusses only those aspects of supportive care that are specifically relevant to the treatment of poisoning.
Depression of the central nervous system. Specific therapy aimed at combating the inhibitory effect of poisons on the central nervous system is usually not necessary and difficult. Most patients with poisoning emerge from a coma, as if from a long-term anesthesia. Careful care is required during the unconscious period nurse and close monitoring of the patient. If the oppression of centers located in medulla oblongata, occurs as a result of circulatory or respiratory problems, then it is necessary to immediately and energetically begin measures to maintain these vital functions using chemicals and mechanical procedures. The use of analeptics in the treatment of patients with venom-induced central nervous system depression has been largely abandoned. It is certain that these substances should never be used to awaken consciousness, and it is doubtful that their use to hasten the restoration of spontaneous breathing and active reflexes has ever been justified. In contrast, the drug antagonist naloxone, administered intravenously in adequate doses, usually reverses the central nervous system depression associated with drug overdose.
Cramps. Many poisons (for example, chlorinated hydrocarbons, insecticides, strychnine) cause the development of seizures due to their specific stimulating effect. In patients with poisoning, convulsions may also occur due to hypoxia, hypoglycemia, cerebral edema or metabolic disorders. In such cases, these violations should be corrected as far as possible. Regardless of the cause of seizures, the use of anticonvulsants is often necessary. Intravenous diazepam, phenobarbital, or phenytoin are usually effective.
Brain swelling. Promotion intracranial pressure caused by cerebral edema is also characteristic feature the effects of some poisons and a nonspecific consequence of other chemical poisonings. For example, cerebral edema occurs with lead, carbon monoxide, and methanol poisoning. Symptomatic treatment consists of the use of adrenocorticosteroids and, when necessary, intravenous administration of hypertonic solutions of mannitol or urea.
Hypotension. The causes of hypotension and shock in a patient with poisoning are numerous and often several causes occur simultaneously. Poisons can cause depression of vasomotor centers in the medulla, block autonomic ganglia or adrenergic receptors, directly inhibit the tone of smooth muscles of arteries or veins, reduce myocardial contractility or induce the appearance of cardiac arrhythmias. Less specific is the condition when the patient with poisoning is in shock due to tissue hypoxia, extensive tissue destruction by corrosive substances, loss of blood and fluid, or metabolic disorders. If possible, these violations must be corrected. If central venous pressure is low, then the first therapeutic action should be to replenish fluid volume in the body. Vasoactive drugs are often useful and sometimes necessary to treat a poisoned patient who has developed hypotension, especially in shock due to central nervous system depression. As with shock caused by other causes, choosing the most appropriate drug requires an analysis of hemodynamic disturbances, which is carried out after measuring blood pressure.
Cardiac arrhythmias. Disturbances in the generation of excitation waves or cardiac conduction in patients with poisoning arise as a result of the action of certain poisons on electrical properties cardiac fibers or as a result of myocardial hypoxia or metabolic disorders in the myocardium. The latter need to be corrected, and antiarrhythmic drugs are used according to indications, based on the nature of the arrhythmia.
Pulmonary edema. A patient with poisoning may develop pulmonary edema due to inhibition of myocardial contractility or damage to the alveoli by irritating gases or aspirated liquids. The latter type of edema is less treatable and may be accompanied by laryngeal edema. Therapeutic measures include suctioning of exudate, giving oxygen in high concentrations under positive pressure, administering aerosols of surfactants, bronchodilators and adrenocorticosteroids.
Hypoxia. Poisoning can cause the development of tissue hypoxia through various mechanisms, and several of these mechanisms can operate simultaneously in one patient. Inadequate ventilation may result from central respiratory depression, muscle paralysis or airway obstruction from accumulated secretions, laryngeal edema, or bronchospasm. Alveolar-capillary diffusion may be impaired during pulmonary edema. Anemia, methemoglobinemia, carboxyhemoglobinemia, or shock may impair oxygen transport. Inhibition of cellular oxidation (eg, cyanide, fluoroacetate) may occur. Adequate patency must be maintained for treatment airways. The clinical situation and location of the obstruction may indicate frequent suctioning, insertion of an oropharyngeal airway or endotracheal tube, or tracheotomy. If, despite normal airway patency, ventilation remains inadequate, as confirmed by clinical condition or measuring minute volume or blood gas composition, the imperative is to carry out artificial ventilation with the help of appropriate mechanical means. In case of tissue hypoxia, the introduction of high concentrations of oxygen is always indicated. In cases where severe depression of the central nervous system occurs, the administration of oxygen often leads to respiratory arrest and must be accompanied by artificial ventilation.
Acute renal failure. Renal failure with oliguria or anuria may develop in a patient with poisoning due to shock, dehydration, or electrolyte imbalance. In more specific cases, it may be due to the nephrotoxic action of certain poisons (eg, mercury, phosphorus, carbon tetrachloride, bromate), many of which are concentrated and excreted by the kidneys. Kidney damage caused by poisons is usually reversible.
Electrolyte and water balance disorders. Electrolyte and water imbalances are common signs chemical poisoning. They may be caused by vomiting, diarrhea, renal failure or therapeutic measures such as bowel cleansing with laxatives, forced diuresis or dialysis. These disorders can be corrected or prevented with appropriate therapy. Certain poisons have a more specific effect, causing the development of metabolic acidosis (eg, methanol, phenol, salicylate) or hypocalcemia (eg, fluoride, oxalate). These disorders and all specific treatments are described in the sections devoted to individual poisons.
Acute liver failure. Primary manifestation Some poisonings (eg, chlorinated hydrocarbons, phosphorus, hypophen, certain mushrooms) cause acute liver failure.
Administration of systemic antidotes. Specific antidote therapy is possible only for poisoning with a small number of poisons. Some systemic antidotes are chemical substances that have their own therapeutic effect, reducing the concentration of a toxic substance. This is achieved by combining the antidote with a specific poison (eg, ethylenediaminetetraacetate with lead, dimercaprol with mercury, reagents having sulfhydryl groups with the toxic metabolite of acetaminophen) or by increasing the excretion of poisons (eg, choride or mercuric diuretics for bromide poisonings). Other systemic antidotes compete with the venom for receptors at the site of their action (for example, atropine with muscarine, naloxone with morphine, physostigmine eliminates some of the anticholinergic effects of tricyclic antidepressants as well as antihistamines, belladonna and other atropine-like substances). Specific antidotes are discussed in the sections on individual poisons.
Which doctors should you contact if you have Chemical poisoning:
- Surgeon
- Infectious disease specialist
Is something bothering you? Do you want to know more detailed information about Chemical poisoning, its causes, symptoms, methods of treatment and prevention, the course of the disease and diet after it? Or do you need an inspection? You can make an appointment with a doctor– clinic Eurolab always at your service! The best doctors will examine you and study you external signs and will help you identify the disease by symptoms, advise you and provide the necessary assistance and make a diagnosis. You can also call a doctor at home. Clinic Eurolab open for you around the clock.
How to contact the clinic:
Phone number of our clinic in Kyiv: (+38 044) 206-20-00 (multi-channel). The clinic secretary will select a convenient day and time for you to visit the doctor. Our coordinates and directions are indicated. Look in more detail about all the clinic’s services on it.
(+38 044) 206-20-00
If you have previously performed any research, Be sure to take their results to a doctor for consultation. If the studies have not been performed, we will do everything necessary in our clinic or with our colleagues in other clinics.
At yours? It is necessary to take a very careful approach to your overall health. People don't pay enough attention symptoms of diseases and do not realize that these diseases can be life-threatening. There are many diseases that at first do not manifest themselves in our body, but in the end it turns out that, unfortunately, it is too late to treat them. Each disease has its own specific signs, characteristic external manifestations - the so-called symptoms of the disease. Identifying symptoms is the first step in diagnosing diseases in general. To do this, you just need to do it several times a year. be examined by a doctor to not only prevent terrible disease, but also support healthy mind in the body and the organism as a whole.
If you want to ask a doctor a question, use the online consultation section, perhaps you will find answers to your questions there and read self care tips. If you are interested in reviews about clinics and doctors, try to find the information you need in the section. Also register on the medical portal Eurolab to stay up to date latest news and information updates on the website, which will be automatically sent to you by email.
Other diseases from the group Trauma, poisoning and some other consequences of external causes:
| Arrhythmias and heart block in cardiotropic poisonings |
| Depressed skull fractures |
| Intra- and periarticular fractures of the femur and tibia |
| Congenital muscular torticollis |
| Congenital malformations of the skeleton. Dysplasia |
| Lunate dislocation |
| Dislocation of the lunate and proximal half of the scaphoid (de Quervain's fracture dislocation) |
| Tooth luxation |
| Dislocation of the scaphoid |
| Dislocations of the upper limb |
| Dislocations of the upper limb |
| Dislocations and subluxations of the radial head |
| Dislocations of the hand |
| Dislocations of the foot bones |
| Shoulder dislocations |
| Vertebral dislocations |
| Forearm dislocations |
| Metacarpal dislocations |
| Foot dislocations at the Chopart joint |
| Dislocations of the phalanges of the toes |
| Diaphyseal fractures of the leg bones |
| Diaphyseal fractures of the leg bones |
| Old dislocations and subluxations of the forearm |
| Isolated fracture of the ulnar shaft |
| Deviated nasal septum |
| Tick paralysis |
| Combined damage |
| Bone forms of torticollis |
| Posture disorders |
| Knee instability |
| Gunshot fractures in combination with soft tissue defects of the limb |
| Gunshot injuries to bones and joints |
| Gunshot injuries to the pelvis |
| Gunshot injuries to the pelvis |
| Gunshot wounds of the upper limb |
| Gunshot wounds of the lower limb |
| Gunshot wounds to joints |
| Gunshot wounds |
| Burns from contact with Portuguese man-of-war and jellyfish |
| Complicated fractures of the thoracic and lumbar spine |
| Open injuries to the diaphysis of the leg |
| Open injuries to the diaphysis of the leg |
| Open injuries to the bones of the hand and fingers |
| Open injuries to the bones of the hand and fingers |
| Open injuries of the elbow joint |
| Open foot injuries |
| Open foot injuries |
| Frostbite |
| Wolfsbane poisoning |
| Aniline poisoning |
| Antihistamine poisoning |
| Antimuscarinic drug poisoning |
| Acetaminophen poisoning |
| Acetone poisoning |
| Poisoning with benzene, toluene |
| Toadstool poisoning |
| Poisoning with poisonous wech (hemlock) |
| Halogenated hydrocarbon poisoning |
| Glycol poisoning |
| Mushroom poisoning |
| Dichloroethane poisoning |
| Smoke poisoning |
| Iron poisoning |
| Isopropyl alcohol poisoning |
| Insecticide poisoning |
| Iodine poisoning |
| Cadmium poisoning |
| Acid poisoning |
| Cocaine poisoning |
| Poisoning with belladonna, henbane, datura, cross, mandrake |
| Magnesium poisoning |
| Methanol poisoning |
| Methyl alcohol poisoning |
| Arsenic poisoning |
| Indian hemp drug poisoning |
| Poisoning with hellebore tincture |
| Nicotine poisoning |
| Carbon monoxide poisoning |
| Paraquat poisoning |
| Poisoning by smoke vapors from concentrated acids and alkalis |
| Poisoning by oil distillation products |
| Poisoning with anti-depressant drugs |
| Salicylate poisoning |
| Lead poisoning |
| Hydrogen sulfide poisoning |
| Carbon disulfide poisoning |
| Poisoning with sleeping pills (barbiturates) |
| Poisoning with fluoride salts |
| Poisoning by central nervous system stimulants |
| Strychnine poisoning |
| Tobacco smoke poisoning |
| Thallium poisoning |
| Tranquilizer poisoning |
| Acetic acid poisoning |
| Phenol poisoning |
| Phenothiazine poisoning |
| Phosphorus poisoning |
| Poisoning with chlorine-containing insecticides |
| Poisoning with chlorine-containing insecticides |
| Cyanide poisoning |
| Ethylene glycol poisoning |
| Ethylene glycol ether poisoning |
| Poisoning with calcium ion antagonists |
| Barbiturate poisoning |
| Poisoning with beta-blockers |
| Poisoning with methemoglobin formers |
| Poisoning with opiates and narcotic analgesics |
| Poisoning with quinidine drugs |
| Pathological fractures |
| Maxillary fracture |
| Fracture of the distal radius |
| Tooth fracture |
| Fracture of the nasal bones |
| Scaphoid fracture |
| Fracture of the radius in the lower third and dislocation in the distal radial-ulnar joint (Galeazzi injury) |
| Fracture of the lower jaw |
| Fracture of the base of the skull |
| Proximal femur fracture |
| Calvarial fracture |
| Jaw fracture |
| Fracture of the jaw in the area of the alveolar process |
| Skull fracture |
| Fracture-dislocations in the Lisfranc joint |
| Fractures and dislocations of the talus |
| Fractures and dislocations of the cervical vertebrae |
| Fractures of the II-V metacarpal bones |
| Fractures of the femur in the area of the knee joint |
| Femur fractures |
| Fractures in the trochanteric region |
| Fractures of the coronoid process of the ulna |
| Acetabular fractures |
| Acetabular fractures |
| Fractures of the head and neck of the radius |
Food intoxication traditionally occupies the top of the ranking among the most common types of intoxication. But this does not mean that poisoning with household chemicals is less dangerous. In some cases, such a sharp deterioration in well-being has a more serious negative effect on the body than food intoxication that has become habitual.
Another pitfall is the fact that this intoxication format can provoke chronic diseases almost all internal organs. A few days of illness can result not only in hospitalization in intensive care, but also in a new illness that will remain with the victim for life.
Classification of detergents and cleaning products
 The most common reason for contacting a doctor in this case is ignoring safety rules. This extends not only to recommendations for storing powders away from curious children, but also to a reluctance to adhere to a certain pattern of behavior during their direct use. But still, more often than not, curious children who try everything to their teeth become victims of multi-colored bottles and bags.
The most common reason for contacting a doctor in this case is ignoring safety rules. This extends not only to recommendations for storing powders away from curious children, but also to a reluctance to adhere to a certain pattern of behavior during their direct use. But still, more often than not, curious children who try everything to their teeth become victims of multi-colored bottles and bags.
In order to provide high-quality first aid to a victim of any age, you must first understand what category the toxic agent belonged to. Schematically, all chemicals used in everyday life can be divided into several large groups:
- cosmetics,
- preparations for neutralizing pests,
- detergents;
- varnishes, paints;
- stain removers.
The main components of cosmetics are usually various alcohols. After penetrating inside, they immediately begin their destructive effects. Sometimes such intoxication does not make itself felt immediately, which adds problems to parents of curious children.
Somewhat less frequently recorded are cases where insecticides became sources of toxins that entered the body in any way. These components are the basis for products aimed at combating insects and other pests. Due to organophosphorus compounds, the danger from human contact with them increases significantly.
One of the most dangerous situations is intoxication with liquids used to clean metal surfaces such as plumbing fixtures. Their composition offers acids and alkalis in abundance for better cleansing of the entrusted territory. But when ingested, they provoke the most severe consequences.
Stain removers are no less dangerous. This is explained by the chlorine-containing composition.
But, regardless of what exactly caused the poisoning from household chemicals, experts strongly recommend immediately seeking help from specialists. The longer the victim delays consultation, the higher the risk of remaining disabled, or even losing his life due to severe complications or anaphylactic shock.
Main causes for chemical intoxication
 Depending on what exactly served as the source sharp deterioration well-being, the reasons will differ. But even taking into account the spectrum of action of household chemicals, most often young children become its victims. The adults are to blame for this because they did not put bright bottles and bags in advance in places where the baby could not reach.
Depending on what exactly served as the source sharp deterioration well-being, the reasons will differ. But even taking into account the spectrum of action of household chemicals, most often young children become its victims. The adults are to blame for this because they did not put bright bottles and bags in advance in places where the baby could not reach.
When choosing a place for the future storage of all household cleaning products and other similar purposes, you should definitely take into account not only the accessibility of young family members to them. The selected cabinet should be located away from areas where heaters are operating or there is any other heat source.
You should also ensure that all containers for subsequent storage are tightly sealed. It's about not just about liquid bottles that have stoppers. It is better to pour bulk products into separate containers with tight-fitting lids. You can find them in any hardware department of the supermarket, or use those packages that are left over from other products.
You should also not ignore the instructions for use, which are indicated on back side containers with hazardous contents. If it says that working with the solution should be done strictly with rubber gloves, you should not skimp on buying them. Some liquids should even be used with safety glasses. This applies to cases of washing plastic ceilings with chlorine-containing mixtures.
Special attention must be paid to the mandatory ventilation of the room where work is carried out with various washing and cleaning solutions. And here it doesn’t matter whether ventilation will be carried out naturally when the window is open, or a special ventilation system will work.
Not all fans of clean surfaces are aware that frequent use detergents provoke the accumulation of toxic components in the blood and tissues. This applies to both people whose professional activities are closely related to household chemicals, and ordinary housewives. Accumulating in the body, the elements will first gradually poison the cells unnoticed, and then begin to manifest themselves more aggressively.
This will be expressed as:
- allergic reactions,
- skin inflammations,
- reduction of protective forces.
Depending on the specifics of the means, other negative manifestations like loss of concentration, increased irritability or problems with destabilization of lung function.
Much less common are cases where a person deliberately ingests a toxic substance. This is usually characteristic of people with some deviations in psychological health, or those who decide to commit suicide. If the powder or mixture was taken orally through negligence, then this is usually limited to a small dosage. With correctly provided first aid and subsequent hospitalization in a hospital, reduce the risks possible complications it will be to a minimum.
One should not discount situations when a toxic substance enters the body through non-oral routes. We are talking about inhalation, penetration through the skin or mucous membranes. In this situation, the harm caused is no less noticeable, and the algorithm for providing assistance changes dramatically.
But, regardless of how exactly the toxins caused damage to the victim’s body, they provoke an imbalance in the functioning of organs, tissues and cells. In the worst case scenario, even respiratory arrest is possible.
Main and secondary signs of intoxication
To recognize poisoning from household chemicals in time and seek treatment qualified help, you need to know exactly the main signs of intoxication. Classical clinical picture looks as follows:
- nausea,
- vomit,
- pain syndrome in the abdominal area,
- disorders digestive tract,
- lethargy,
- headache,
- cough,
- pain in the throat,
- impaired vision,
- foam at the mouth,
- convulsive syndrome,
- fainting.
All of the above refers to the standard set, but since all representatives of household chemicals have their own characteristics, attention should be paid to them.
So, plumbing fluids provoke not only nausea. They cause severe irritation of the respiratory tract, which results in coughing and even suffocation.
Almost the same thing happens when exposed to chlorine-containing substances that block normal functioning respiratory function and blood circulation.
The last point is explained by the fact that a number of toxins are killers for red cells. Because of this, access to the oxygen supply to the cells is almost completely blocked. If you delay assistance at this stage, the picture will end with brain hypoxia.
Chemical vapor poisoning
With respiratory intoxication, foam from the mouth is not the worst outcome. Such poisoned people constantly faint, and also suffer from convulsive syndrome and muscle spasms.
Regardless of the name of the product that served as the source of toxins, the victim must first get out into the fresh air. Having laid the patient on a flat surface, it is worth ridding him of all constricting parts of clothing such as scarves and ties. Usually, the influx of fresh air revives even those who were previously in a faint state. Immediately after “waking up” they complain of dizziness and sudden headache, pain in the eyes.
If, along with vapor intoxication, poisons are ingested, the patient should be immediately given a saline laxative. But doing gastric lavage in such cases is strictly prohibited. It is better to call an ambulance and make sure that the victim is conscious.
If you try to call gag reflex artificially, this once again injures the esophagus and mucous membranes of the stomach and oral cavity. If the swelling is extensive, it may cause breathing to stop.
It will be possible to rinse the stomach only after the patient is hospitalized. In a hospital setting, healthcare workers use a probe and special rinsing water.
Exposure to acid, alkaline and organophosphorus agents
First characteristic symptom intoxication due to acids and alkalis causes profuse vomiting. Moreover, the discharged vomit will have bloody inclusions. This happens due to bleeding in the intestines. At the very dangerous development events, even swelling of the larynx is possible, so it is extremely important to immediately transport the patient to the hospital. In such victims, the urine has a specific dark color or even a reddish tint.
In case of alkaline or acid intoxication, it is strictly forbidden to induce vomiting. Despite the fact that doctors usually prohibit giving any medications to a poisoned person, here it is allowed to use painkillers before the arrival of a team of specialists. But an attempt to block the effect of an acid or alkali with a chemical antidote can result in death.
With organophosphates, the primary care regimen is more similar to that recommended for exposure to turpentine or gasoline. First, the patient is taken to open air, getting rid of clothes that restrict breathing.
Experts say that, unlike many other toxins, it is organophosphorus solutions that can settle on clothing. Because of this, the victim may take much longer to recover than expected. If the patient is conscious, then he is recommended:
- remove contaminated clothing,
- take a warm shower,
- change into clean clothes.
If during washing it is noticed that a substance has come into contact with a certain area of the skin, this area is washed with regular soap.
Skin contact with formaldehyde-containing components
 When toxins come into contact with the skin, their negative effects do not immediately make themselves felt. But the absence of pronounced signs of damage to the epidermis or deeper layers of the skin does not mean that everything is in order.
When toxins come into contact with the skin, their negative effects do not immediately make themselves felt. But the absence of pronounced signs of damage to the epidermis or deeper layers of the skin does not mean that everything is in order.
Doctors advise immediately after getting the substance on the skin to thoroughly rinse the affected area with a solution of ammonia. If, in addition to splashes on open areas of the body, the patient inhaled poisoned fumes, then he must immediately leave the contaminated area.
In addition to washing the skin, you need to take special care to rinse your throat, as well as your mouth and nasal cavity. Before the doctors arrive, you should drink a lot of Borjomi-type mineral water, or warm milk with a little soda added. Any other drinks should be excluded.
Particular attention should be paid to the patient’s complaints about damage to the organs of vision. In this case, you need to rinse your eyes with running, slightly warm water for at least twenty minutes.
medtox.net
Chemical poisoning - First aid for chemical poisoning
In everyday life, people constantly come into contact with toxic chemicals. Poisoning with them can occur if handled incorrectly, dosage and rules for safe use are not followed. This is a fairly serious type of poisoning, during which a person may remain disabled or die if medical attention is not provided in a timely manner.
What is it?

Chemical poisoning is the process of damage to the human body by toxic substances when they enter the blood, stomach and intestines through the respiratory system.
Poisoning can occur by inhaling vapors or ingesting the product.
The following lists the main number of human objects that cause poisoning:
- acetic acid. May cause severe poisoning if ingested or inhaled;
- oil- or acetone-based paints and varnishes;
- all types of solvents;
- glue;
- pesticides and herbicides (products for treating plants and killing insects);
- toxic aerosols;
- means for exterminating rodents;
- acetone;
- fuels and lubricants.
Almost all of them contain poisons that are harmful to the human body. When working with the above substances in confined spaces with poor ventilation, chemical poisoning occurs upon contact with mucous membranes, inhalation of vapors or ingestion. Most often, this type of poisoning occurs when basic safety rules when handling materials are not followed. toxic substances.
Symptoms of toxic chemical poisoning
Manifestation of chemical poisoning. substances depends on the weight and age of the patient, his state of health and the amount of toxic substance that has entered the body.
Many toxic substances affect the body within long period time with minimal signs. It depends on the level of toxicity of the poison. The more toxic the poison, the more signs and the faster they appear. And the more destructive their effect on the entire body. Often the same poison causes chemical poisoning in one person while another experiences nothing. This is due to the level of immunity, genetics and susceptibility to toxic substances.
For example, children are more susceptible to poisoning than adults. This is due to the fact that per 1 kg child weight there is more poison than an adult. And because of low level immunity and weakness of the human body old age will be more susceptible to the toxic composition than a 30 year old man.
The effects of poison and signs of chemical poisoning are very individual and depend on many factors, including those listed above. If people have previously suffered from allergies or bronchial asthma, then they are more sensitive to pronounced smells, therefore, their body reacts faster to a toxic substance.
Signs of chemical poisoning depends on its severity
For mild types:
- dizziness;
- nausea, vomiting;
- redness, dryness, itching of the skin;
- tearfulness;
- nasal congestion;
- with moderate and severe poisoning;
- nausea, vomiting;
- temperature;
- swelling of the respiratory tract mucosa;
- Quincke's edema;
- bronchospasms;
- convulsions;
- fainting;
- blurred vision;
- paralysis of limbs;
- loss of speech;
- disorientation;
- hallucinations;
- coma;
In addition, poisoning with chemicals or other poisons can lead to burns of the mucous membrane, respiratory tract and esophagus. Lead to irreversible processes in the gastrointestinal tract. Lead to pulmonary edema, paralysis of the central nervous system. If the patient is not provided with timely medical assistance, a poisoning situation can end in death.
In case of severe poisoning, all these signs can occur simultaneously, aggravating the patient’s health condition. Symptoms of chemical poisoning do not appear immediately. A person may feel unwell after several hours or several days. Poisoning may appear the next day. The more time passes from the moment of poisoning to the moment of diagnosis, the more difficult it is to provide assistance to the poisoned person.
Some types of poisoning may not have any visible signs. Toxins settle in the body and affect the functioning of the liver and kidneys. A person may not know that pesticides have caused damage to his health. This most often occurs due to involuntary inhalation of chemical vapors. The person feels weakness and nausea, which quickly disappear.
Depending on the poison, after the ingestion or use of which poisoning occurred, the signs are classified. Some poisons primarily affect the central nervous system and brain, other respiratory tracts and the gastrointestinal tract, and the musculoskeletal system. Depending on the type of poisoning, the further actions, such as providing assistance, diagnosing and selecting drug therapy.
First aid for poisoning

When providing first aid, it is important to understand the patient’s condition so as not to harm him. If a patient has convulsions, severe hallucinations, or breathing problems, then he needs qualified medical care. In addition, when vomiting and emptying the stomach, you need to remember that the patient may choke on the vomit or it will enter the respiratory tract.
If there is a coma or signs of hemorrhage, you should also not disturb the patient so as not to worsen his condition. If the poisoning is not severe, then you can provide first aid to the poisoned person at home. It all depends on the toxicity and volume of the chemical consumed. If a person is poisoned by vapors or touches the mucous membrane, it is necessary to provide access to fresh air, rinse the mucous membranes and skin with running water, take activated charcoal and seek medical help. If chemicals have entered the body through the respiratory tract and esophagus, it is important to try as quickly as possible to eliminate further absorption of the poison and its remnants from the stomach.
To do this, you need to induce vomiting by pressing on the inner part larynx. The poison that enters the stomach cavity is initially absorbed by only one third. It takes several hours for the remaining chemical to be absorbed. In this regard, it is necessary to quickly remove the contents of the esophagus and stomach.
To facilitate the removal of vomit, you can drink more water. Water will remove the contents of the stomach faster. You can also give activated charcoal to the poisoned person; it very quickly absorbs toxins and promotes their successful removal from the body. Activated carbon is most often used in powder or tablets; unlike liquid, it absorbs toxins better. In the absence of activated carbon, you can use Polysorb or Polyphepan. They also help eliminate intoxication, but a little slower than coal.
Such assistance can be provided to patients who do not have breathing problems, seizures or disorders of the musculoskeletal system. If such changes are present, then the patient should be placed in a horizontal position face down to remove vomit and wait for the ambulance to arrive.
If there is a medical facility nearby, it is necessary to transport the patient there for gastric lavage. For these purposes, a probe is inserted into the stomach through the esophagus, with the help of which the contents of the stomach are emptied. But even after lavage, there may be residual toxins in the stomach cavity. To remove them, you need to take activated carbon.
It is important to understand that the life and health of the patient depend on correctly provided first aid. The bulk of the poison is absorbed in the first minutes, when it is necessary to provide assistance.
If the poisoning was mild and the person feels a slight discomfort in the form of dizziness and nausea, it is necessary to give him activated charcoal. Subsequently, you can take Enterosgel, Polysorb, Polyphepan for several days. Drink fresh milk daily and stay in the fresh air. But in any case, if the causes and circumstances of poisoning are known, it is necessary to seek medical help and provide information to the doctor.
The situation is more complicated when those around the unconscious patient or the person himself do not understand what happened and the poisoning becomes known only in the doctor’s office or after the ambulance arrives. This means that the patient will not receive timely help and the bulk of the toxic substance that has entered the body has already been absorbed into the walls of the stomach and spread throughout the body. Consequently, the destructive process of damage to organs by poisons has already been launched to the maximum.
Diagnosis of chemical poisoning
If poisoning is known, then diagnosis is carried out in a minimal way, a visual examination, blood and urine tests. In such cases, doctors see the picture more clearly and identify tools to combat the disease. When determining the poison from which the poisoning occurred, it is more clear what drug therapy should be used. The esophagus, stomach and intestines are washed. Drug therapy is carried out to remove poison from the body.
It is worse when doctors do not know about the poisoning and the etiology of the poison. In this case, diagnosis is initially made on the basis of the patient’s symptoms. Based on biochemical analysis blood, urine, gastric juice more happens accurate diagnosis. But this takes a certain time, during which the toxins affect the body even more. But unfortunately, in case of severe poisoning, if time is lost during transportation and diagnosis, the patient may be in a comatose or unconscious state, and maximum negative changes occur in the body.
Poisoning with chemical substances falls into the category of dangerous poisoning. In addition to death, a person risks remaining disabled after hemorrhage or paralysis suffered due to poisoning.
Timely diagnosis and treatment play a huge role in the final outcome after chemical poisoning.
Treatment methods
When treating chemical poisoning, classical medication and auxiliary therapy are used. This is a set of measures aimed at removing toxins from the body, eliminating negative consequences and restoring the patient.
Basic therapy can be divided into several stages:
- elimination of the process of absorption of toxic substances;
- measures to remove toxic chemicals;
- drug elimination of symptoms of poisoning in the form of disruption of the functioning of various organs (gastrointestinal tract, liver, kidneys, central nervous system, respiratory organs);
- removal of systemic antidotes from the body. These stages of therapy are used for poisoning with almost any poisons and toxic substances.
But the last stage is only when the toxic chemical with which the patient was poisoned due to the mechanism of action is known. The first stage includes the removal of vomit, active gastric lavage using a probe, absorption using powdered activated carbon.
To quickly and successfully remove the absorbed poison, the patient is prescribed laxatives. As it moves from the stomach to the intestines and through the rectum, activated charcoal is also effective against partially trapped toxins. The removal of absorbed charcoal has virtually no effect on the level of poison entering the blood, but helps to improve the general condition of the patient and reduces further intoxication. In case of poisoning with certain types of toxic substances, methods are used in therapy to accelerate the process of bile formation, kidney and bladder function.
To cleanse the body of toxins in case of poisoning with ethyl alcohol, methanol and other poisons, dialysis and hemosorption are used. That's enough effective methods in the treatment of poisoning. But unfortunately, the equipment necessary for this cannot be found in all medical institutions, which makes its use difficult. Depending on the etiology of the poison, when it enters the body, poisoning occurs, the choice of therapy, medications and methods of removing poison toxins is made. In addition to therapy aimed at combating toxins, treatment is carried out concomitant diseases which were the result of poisoning. For example, treatment of burns of the respiratory tract and esophagus, restoration of affected areas of the walls of the stomach and intestines, maintaining healthy liver and kidney function, eliminating pulmonary edema, raising protective functions the body as a whole, etc. The most complex cases Poisoning with highly concentrated poisons is recognized, which instantly affects the body and is absorbed. For example, pesticides used to treat plants in fields using aircraft. Sometimes in such cases, medical care is no longer effective.
Poisoning prevention measures:
It is important to understand that a person can get chemical poisoning in standard living conditions if basic safety rules are not followed. Toxic chemicals are contained in almost all cleaning, washing, grease, descaling, etc. products. Gasoline and diesel fuel that a driver encounters every day can also lead to severe poisoning. All paints and solvents that we use to paint windows, doors and fences in the country and at home are not safe. Vinegar essence used in home preparations can be fatal if consumed. Almost all aerosols from mosquitoes, flies and other insects are toxic. Even deodorant that comes in an aerosol can contains poison. Many types of medications contain toxic chemicals. Therefore, an overdose or use of expired tablets can also lead to severe poisoning. A person comes into contact with dangerous toxic substances almost every hour and risks getting poisoned.
otravlenie103.ru
Chemical poisoning
Poisons include some medications, household substances, solvents, pesticides and other chemicals.
Symptoms of poisoning depend on the type and amount of poison ingested and the individual characteristics of the victim. Some poisons with low toxicity cause certain problems only with prolonged exposure or repeated exposure to the body in large quantities. Other substances are so poisonous that even one drop of such poison getting on the skin can lead to dire consequences. The toxicity of a substance in each specific case also depends on the genetic characteristics of the person. Some normally non-toxic substances are toxic to people with a certain genotype (set of genes).
The dose of a substance that causes symptoms of poisoning also depends greatly on age. For example, ingesting more paracetamol in a small child is more likely to cause symptoms of poisoning than the same dose in an adult. For an elderly person, a sedative from the group of benzodiazepines (seduxen, Relanium, phenazepam) can be toxic in doses that do not cause any problems in a middle-aged person.
Symptoms of poisoning can be minor but unpleasant, such as itching, dry mouth, blurred vision, pain, or they can be life-threatening, such as confusion, coma, abnormal heart rhythm, difficulty breathing and severe agitation. Some poisons take effect within seconds, while others take several hours or even days to take effect.
There are poisons that do not cause obvious symptoms until there is irreversible damage to the function of vital organs, in particular the liver or kidneys. Thus, the symptoms of poisoning are as countless as the number of poisons.
Optimal management of patients with poisoning requires a correct diagnosis. Although the toxic effects of some chemicals are very characteristic, most of the syndromes observed during poisoning can be caused by other diseases.
Poisoning is commonly included in the differential diagnosis of coma, seizures, acute psychosis, acute liver or kidney failure, and bone marrow suppression. Although this should be done, the possibility of poisoning can be discounted when the patient's main symptoms are mild mental or neurological impairment, abdominal pain, bleeding, fever, hypotension, pulmonary congestion, or skin rash. In addition, the patient may not be aware of the effects of the poison on him, as is the case with chronic, latent poisoning, or after an attempt at suicide or abortion, the patient will also be reluctant to agree with such a diagnosis. Physicians should always be aware of the various manifestations of poisoning and maintain a high degree of vigilance in relation to them.
In all cases of poisoning, an attempt should be made to identify the toxic agent. It is obvious that without such identification it is impossible to carry out specific therapy with antidotes. In cases of murder, suicide or criminal abortion, the determination of poison may have legal significance. In cases where poisoning is the result of industrial exposures or therapeutic error, accurate knowledge of the active agents is necessary to prevent similar occurrences in the future.
In case of acute accidental poisoning, the active substance may be known to the patient. In many other cases, information can be obtained from relatives or friends, by examining containers located at the site of poisoning, or by interviewing the patient’s attending physician or his pharmacist. Often, such actions only allow us to establish the trade name of the product, which does not allow us to find out its chemical composition. The bibliography at the end of this chapter lists a number of books that list the active constituents of substances used in household, agricultural, patent medicines and poisonous plants. Every doctor should carry a small reference book of this type in his briefcase. The latest information of this kind can also be obtained from Poison Treatment Centers and from representatives of manufacturers of these substances. In case of chronic poisoning, it is often impossible to quickly determine the toxic agent based on medical history. The lower urgency of treatment in these cases usually allows for the necessary thorough examination of the patient’s habits and the state of the environment.
Some poisons can cause the development of characteristic clinical signs that are sufficient to strongly suggest an accurate diagnosis. Upon careful examination of the patient, a characteristic odor of cyanide can be detected; cherry staining of the skin and mucous membranes, revealing the presence of carboxyhemoglobin; constriction of the pupil, drooling and gastrointestinal hyperactivity caused by insecticides containing cholinesterase inhibitors; lead rim and extensor muscle paralysis characteristic of chronic lead poisoning. Unfortunately, these typical signs are not always present and in case of chemical poisoning their presence is rather an exception.
Chemical analysis of body fluids provides the most correct determination of the substance that caused the poisoning. Some common poisons, such as acetylsalicylic acid (aspirin) and barbiturates, can be identified and even quantified using relatively simple laboratory tests. Detection of other poisons requires more complex toxicological tests, such as high-performance gas or liquid chromatography, which are carried out only in specialized laboratories. In addition, the results of toxicological studies are rarely available in a timely manner to determine the initial treatment of acute poisoning. However, samples of vomit, gastric aspirate, blood, urine, and stool should be reserved for toxicology testing if diagnostic or legal questions arise. Chemical analysis of body fluids or tissues is especially important in diagnosing and assessing the severity of chronic poisoning. Ultimately, the results of such analyzes are useful for assessing the long-term results of certain types of therapy.
To properly treat a patient with poisoning, it is necessary to know both the basic principles of managing such patients and the details of therapy for specific poisonings. The treatment process includes:
- prevention of further absorption of poison;
- removal of absorbed poison from the body;
- symptomatic maintenance therapy or symptomatic treatment for circulatory, respiratory disorders, neurological disorders and renal dysfunction;
- introduction of systemic antidotes.
The first three steps apply to most types of poisoning. The fourth stage is most often used only when the toxic agent is known and a specific antidote is available. However, sometimes, if there is a high degree of suspicion that the patient is overdosing on opiates, he is given naloxone. It should be realized that for most poisons there are no specific antidotes, and to carry out the necessary maintenance therapy it is not necessary to know which toxic agent caused the poisoning. Thus, although the physician should always attempt to identify the active poison, these attempts should not delay life-saving therapeutic measures. .
Prevention of absorption of ingested poisons. If a significant amount of poison has been ingested, an attempt should be made to minimize its absorption from the gastrointestinal tract. The success of such attempts depends on the time elapsed after ingestion of the poison and on the site and speed of absorption.
- Evacuation of stomach contents
Always, unless there are specific contraindications, you should try to empty the stomach. These attempts can be very successful if done soon after the poison is ingested. Significant amounts of poison may still be cleared from the stomach several hours after ingestion because emptying may be delayed by gastric atony or pylorospasm. This occurs in poisoning with phenothiazines, antihistamines and tricyclic antidepressants.
After swallowing many poisons, vomiting occurs spontaneously. In a minority of cases, it can be induced at home by mechanical irritation of the back of the throat. The emetic effect of ipecac syrup (the concentration should not exceed 14 times the concentration of the liquid extract), given in a dose of 15 - 30 ml, is more effective and safe even at home. Its action begins on average 20 minutes after administration and depends partly on absorption in the gastrointestinal tract, so simultaneous administration of activated carbon, which is an adsorbent, should be avoided. A second dose of ipecac syrup should be given to the patient if he does not vomit 20 minutes after taking the first dose (after taking two doses, vomiting will develop in 90-95% of patients). If ipecac syrup is not available, every effort should be made to find it, even if this means taking the patient to the hospital. Apomorphine, administered intramuscularly at a dose of 0.06 mg/kg, acts within 5 minutes, but can cause prolonged vomiting. When administered intravenously at a dose of 0.01 mg/kg, apomorphine causes vomiting almost immediately, with no subsequent effect on the central nervous system. Sometimes it may not be possible to induce vomiting and valuable time should not be wasted waiting. Attempting to induce vomiting should not be attempted in victims who are convulsive, in patients with severe central nervous system depression, or (due to the risk of gastric or esophageal perforation or because of aspiration of vomit into the trachea) in those who have ingested a potent, caustic chemical. or small quantities (less than 100 ml) of liquid hydrocarbons that are strong lung irritants (eg, kerosene, polish).
Compared to vomiting, gastric lavage is preferable and has an immediate effect, but it usually does not remove poison from the stomach more effectively than vomiting. It can be performed in unconscious patients; evacuation of the stomach contents reduces the risk of aspiration of vomit. Its implementation, however, is contraindicated after ingestion of strong corrosive substances, due to the risk of perforation of damaged tissue. When performed correctly, gastric lavage carries a small risk of aspiration of stomach contents into the lungs. The patient should lie on his stomach with his head and shoulders bowed. Using a mouth dilator, a gastric tube is inserted into the stomach, the diameter of which is sufficient to pass solid particles (30 gauge). If the functions of the central nervous system are depressed, if the insertion of the tube causes vomiting, or if a substance that is a lung irritant has been swallowed, then before performing gastric lavage it is reasonable to insert an endotracheal tube with a cuff into the trachea. The contents of the stomach are aspirated with a large syringe, and with it most of the poison is removed from the body. After this, 200 ml (less in children) of warm water or a liquid solution is injected into the stomach and sucked out until the aspirated liquid becomes clear.
Interference with absorption in the gastrointestinal tract.
Since neither vomiting nor gastric lavage completely empties the stomach, an attempt should be made to reduce absorption by introducing substances that bind toxins that have entered the body. Many poisons are adsorbed by powdered activated carbon. High quality activated carbon can adsorb 50% of the mass of many common poisons. Liquid activated carbon (20-50 g in 100 * 200 ml) should be administered after gastric emptying.
Adsorption by activated carbon is a reversible process and the adsorption efficiency of many poisons varies depending on the pH value. Acidic substances are better absorbed by acid solutions and can therefore be released in the small intestine. It is desirable that the activated charcoal with the adsorbed poison pass through the intestine as quickly as possible. This will also reduce the intestinal absorption of any unabsorbed poison that passes through the pylorus. In patients with good renal and cardiac function, this is best achieved by oral or intramuscular administration of osmotic laxatives agents such as magnesia or sodium sulfate (10 - 30 g in a solution with a concentration of 10% or less).
Prevention of absorption of poison from other organs and systems. Most topically applied poisons can be removed from the body by abundant rinsing with water. In certain cases, weak acids or alkalis or alcohol in combination with soap are more effective, but rapid and copious rinsing with water must be carried out until these solutions are available to doctors. Chemical antidotes are dangerous because the heat generated by the chemical reaction can cause tissue damage.
The systemic distribution of injected venoms can be slowed by applying a cold compress or ice to the injection site or by applying a tourniquet proximal to the injection site.
After inhalation of toxic gases, vapors or dust, remove the victim to clean air and maintain adequate ventilation. The patient cannot move and must wear a protective mask.
Removing absorbed poison from the body. In contrast to preventing or slowing absorption, measures that accelerate the elimination of the toxic agent and the body rarely have a major effect on the peak concentration of the poison in the body. However, they can significantly reduce the time during which the concentration of many poisons remains above a certain level, and thereby reduce the risk of complications and the death of the patient. When assessing the need to carry out such measures, it is necessary to take into account the clinical condition of the patient, the properties and pathways of metabolism of the poison and the amount of absorbed poison based on medical history and the results of determining its concentration in the blood. The administration of some poisons can be accelerated by various methods; The choice of method depends on the condition of the patient, the amount of poison in the body and the availability of experienced personnel and equipment.
Certain organic acids and active drugs are secreted into bile in a direction opposite to the large concentration gradient. This process takes some time and cannot be accelerated. However, the absorption in the intestine of substances already secreted into bile, such as glutethimide, can be reduced by introducing activated carbon every 6 hours. The organochlorine pesticide - chlordenone - is slowly eliminated from the body (half-life from the blood is 165 days). Cholestyramine (16 g per day) significantly accelerates its elimination (half-life from the blood is 80 days).
Acceleration of renal excretion is justified in cases of poisoning with a much larger number of poisons. Renal excretion of toxic substances depends on glomerular filtration, active tubular secretion and passive tubular resorption. The first two of these processes can be protected by maintaining adequate circulation and kidney function, but as a practical matter they cannot be accelerated. On the other hand, passive tubular resorption of many poisons plays an important role in prolonging their period of action and can often be reduced by readily available methods. In case of poisoning with drugs such as salicylic acid preparations and long-acting barbiturates, increased diuresis induced by the administration of large volumes of electrolyte solutions in combination with intravenous furosemide has been demonstrated to enhance renal excretion.
A change in urine pH can also inhibit the passive reversible diffusion of some poisons and increase their renal clearance. The renal tubular epithelium is more permeable to uncharged particles than to ionized solutions. Weak organic acids and bases diffuse easily from the tubular fluid in their non-ionized form, but are retained in the tubules if they are ionized. Acidic poisons are ionized only at a pH higher than their pK. Alkalinization of urine sharply increases the ionization of organic acids such as phenobarbital and salicylate in the tubular fluid. In contrast, the pK values of pentobarbital (8.1) and secobarbital (8.0) are so high that renal clearance does not increase appreciably as urine pH increases within the physiological alkaline range. Alkalinization of urine is achieved by infusion of sodium bicarbonate at a rate determined by the pH value of urine and blood. The development of severe systemic alkalosis or electrolyte imbalance should be avoided. The combination of controlled diuresis with urine alkalinization can increase the renal clearance of some acid poisons by 10-fold or more, and these measures have been found to be very effective in poisoning with salicylates, phenobarbital, and 2,4-dichlorophenoxyacetic acid. Conversely, lowering the pH value below its normal values has been shown to increase the clearance of amphetamines, phencyclidines, fenfluramine and quinine.
In conclusion, it should be noted that the renal excretion of certain poisons can be increased by highly specific methods. An example of this is the removal of bromide from the body through the administration of chloride and chloruretics. These methods are discussed when considering individual poisons.
Dialysis has been found to be effective in removing many substances from the body, including barbiturates, borate, chlorate, ethanol, glycols, methanol, salicylates, sulfonamides, theophylline, and thiocyanate. Theoretically, it should accelerate the elimination from the body of any dialyzable toxin that is not irreversibly bound to tissues. Its effectiveness does not apply to large molecules, non-dialyzable poisons and is reduced to a large extent by the binding of the toxic substance to proteins or its solubility in fats.
Peritoneal dialysis can be easily performed in any hospital and can be done over a long period of time. However, performing it for the purpose of removing poisons from the body is justified only if the patient has impaired renal function, hemodialysis or hemosorption is impossible, or forced diuresis cannot be used.
Hemodialysis is undoubtedly more effective in removing large quantities of dialyzed poisons from the body. For barbiturates, dialysis rates of 50 - 100 ml/min have been achieved, while the rate of their elimination from the body is 2 - 10 times higher than with peritoneal dialysis or forced diuresis. When blood is perfused through activated carbon or ion exchange resin, even greater rates of clearance of most poisons are achieved than with hemodialysis. It is clear that extracorporeal dialysis and hemosorption may be considered the procedures of choice for the rapid removal of poisons from the body of patients who have absorbed quantities of poison that make it unlikely that they will survive even with the best supportive care provided. Since the equipment and experienced personnel necessary for hemodialysis and hemosorption are not available in every hospital, the possibility of transferring such patients to a facility that has such capabilities should be considered.
Complexation and chemical bonding. The elimination of some poisons from the body is accelerated by chemical interaction. actions with other substances followed by excretion through the kidneys. These substances are considered systemic antidotes and are discussed when considering individual poisons.
Maintenance therapy. Most chemical poisonings are reversible, self-limiting disease states. Skillful supportive care can keep many severely poisoned patients alive and keep their detoxifying and excretory mechanisms functioning until the concentration of the poison has decreased to safe levels. Symptomatic measures are especially important when the active poison belongs to the category of substances for which a specific antidote is unknown. Even when an antidote is available, the possibility of impairment of vital functions should be prevented or controlled with appropriate supportive care.
A patient with poisoning may suffer from various physiological disorders. Most of them are not specific to chemical poisoning and the management of such patients is discussed in other sections. This section briefly discusses only those aspects of supportive care that are specifically relevant to the treatment of poisoning.
Depression of the central nervous system. Specific therapy aimed at combating the inhibitory effect of poisons on the central nervous system is usually not necessary and difficult. Most patients with poisoning emerge from a coma, as if from a long-term anesthesia. During the unconscious period, careful nursing care and close monitoring of the patient are necessary. If inhibition of centers located in the medulla oblongata occurs as a result of circulatory or respiratory disorders, then measures to maintain these vital functions must immediately and vigorously be started using chemicals and mechanical procedures. The use of analeptics in the treatment of patients with venom-induced central nervous system depression has been largely abandoned. It is certain that these substances should never be used to awaken consciousness, and it is doubtful that their use to hasten the restoration of spontaneous breathing and active reflexes has ever been justified. In contrast, the drug antagonist naloxone, administered intravenously in adequate doses, usually reverses the central nervous system depression associated with drug overdose.
Cramps. Many poisons (for example, chlorinated hydrocarbons, insecticides, strychnine) cause the development of seizures due to their specific stimulating effect. In patients with poisoning, convulsions may also occur due to hypoxia, hypoglycemia, cerebral edema or metabolic disorders. In such cases, these violations should be corrected as far as possible. Regardless of the cause of seizures, the use of anticonvulsants is often necessary. Intravenous diazepam, phenobarbital, or phenytoin are usually effective.
Brain swelling. Increased intracranial pressure caused by cerebral edema is also a characteristic sign of the action of some poisons and a nonspecific consequence of other chemical poisonings. For example, cerebral edema occurs with lead, carbon monoxide, and methanol poisoning. Symptomatic treatment consists of the use of adrenocorticosteroids and, when necessary, intravenous administration of hypertonic solutions of mannitol or urea.
Hypotension. The causes of hypotension and shock in a patient with poisoning are numerous and often several causes occur simultaneously. Poisons can cause depression of vasomotor centers in the medulla, block autonomic ganglia or adrenergic receptors, directly inhibit the tone of smooth muscles of arteries or veins, reduce myocardial contractility or induce the appearance of cardiac arrhythmias. Less specific is the condition when the patient with poisoning is in shock due to tissue hypoxia, extensive tissue destruction by corrosive substances, loss of blood and fluid, or metabolic disorders. If possible, these violations must be corrected. If central venous pressure is low, then the first therapeutic action should be to replenish fluid volume in the body. Vasoactive drugs are often useful and sometimes necessary to treat a poisoned patient who has developed hypotension, especially in shock due to central nervous system depression. As with shock caused by other causes, choosing the most appropriate drug requires an analysis of hemodynamic disturbances, which is carried out after measuring blood pressure.
Cardiac arrhythmias. Disturbances in the generation of excitation waves or cardiac conduction in patients with poisoning arise as a result of the action of certain poisons on the electrical properties of cardiac fibers or as a result of myocardial hypoxia or metabolic disorders in the myocardium. The latter need to be corrected, and antiarrhythmic drugs are used according to indications, based on the nature of the arrhythmia.
Pulmonary edema. A patient with poisoning may develop pulmonary edema due to inhibition of myocardial contractility or damage to the alveoli by irritating gases or aspirated liquids. The latter type of edema is less treatable and may be accompanied by laryngeal edema. Therapeutic measures include suctioning of exudate, giving oxygen in high concentrations under positive pressure, administering aerosols of surfactants, bronchodilators and adrenocorticosteroids.
Hypoxia. Poisoning can cause the development of tissue hypoxia through various mechanisms, and several of these mechanisms can operate simultaneously in one patient. Inadequate ventilation may result from central respiratory depression, muscle paralysis or airway obstruction from accumulated secretions, laryngeal edema, or bronchospasm. Alveolar-capillary diffusion may be impaired during pulmonary edema. Anemia, methemoglobinemia, carboxyhemoglobinemia, or shock may impair oxygen transport. Inhibition of cellular oxidation (eg, cyanide, fluoroacetate) may occur. For treatment, it is necessary to maintain adequate airway patency. The clinical situation and location of the obstruction may indicate frequent suctioning, insertion of an oropharyngeal airway or endotracheal tube, or tracheotomy. If, despite a normal airway, ventilation remains inadequate, as evidenced by clinical status or cardiac output or blood gas measurements, mechanical ventilation by appropriate mechanical means is imperative. In case of tissue hypoxia, the introduction of high concentrations of oxygen is always indicated. In cases where severe depression of the central nervous system occurs, the administration of oxygen often leads to respiratory arrest and must be accompanied by artificial ventilation.
Acute renal failure. Renal failure with oliguria or anuria may develop in a patient with poisoning due to shock, dehydration, or electrolyte imbalance. In more specific cases, it may be due to the nephrotoxic action of certain poisons (eg, mercury, phosphorus, carbon tetrachloride, bromate), many of which are concentrated and excreted by the kidneys. Kidney damage caused by poisons is usually reversible.
Electrolyte and water balance disorders. Electrolyte and fluid imbalances are common signs of chemical poisoning. They may be caused by vomiting, diarrhea, renal failure or therapeutic measures such as bowel cleansing with laxatives, forced diuresis or dialysis. These disorders can be corrected or prevented with appropriate therapy. Certain poisons have a more specific effect, causing the development of metabolic acidosis (eg, methanol, phenol, salicylate) or hypocalcemia (eg, fluoride, oxalate). These disorders and all specific treatments are described in the sections devoted to individual poisons.
Acute liver failure. The primary manifestation of some poisonings (eg, chlorinated hydrocarbons, phosphorus, hypophen, certain fungi) is acute liver failure.
Administration of systemic antidotes. Specific antidote therapy is possible only for poisoning with a small number of poisons. Some systemic antidotes are chemical substances that exert their therapeutic effect by reducing the concentration of a toxic substance. This is achieved by combining the antidote with a specific poison (eg, ethylenediaminetetraacetate with lead, dimercaprol with mercury, reagents having sulfhydryl groups with the toxic metabolite of acetaminophen) or by increasing the excretion of poisons (eg, choride or mercuric diuretics for bromide poisonings). Other systemic antidotes compete with the venom for receptors at the site of their action (for example, atropine with muscarine, naloxone with morphine, physostigmine eliminates some of the anticholinergic effects of tricyclic antidepressants as well as antihistamines, belladonna and other atropine-like substances). Specific antidotes are discussed in the sections on individual poisons.
www.eurolab.ua
Symptoms and principles of first aid for chemical poisoning
 Poisoning with chemicals can occur in hazardous industries, at home, and during combat. Toxic compounds enter the body through food, drink, and contaminated air. They can penetrate through the skin, mucous membranes, through the intestines, bronchi and lungs. When poisoned by chemicals, symptoms can be different, because toxins affect different systems and organs.
Poisoning with chemicals can occur in hazardous industries, at home, and during combat. Toxic compounds enter the body through food, drink, and contaminated air. They can penetrate through the skin, mucous membranes, through the intestines, bronchi and lungs. When poisoned by chemicals, symptoms can be different, because toxins affect different systems and organs.
Signs of chemical poisoning
Signs of poisoning by hazardous chemical substances depend on the class of substances and the route of entry into the body. The main symptoms of chemical poisoning:
- Nausea and vomiting.
- Hallucinations.
- Stomach ache.
- Increased heart rate or cardiac arrest.
- Constriction or dilation of the pupils (miosis and mydriasis).
- Paleness of the skin, its cyanosis or yellowness.
- Bleeding.
- Breathing disorders: shortness of breath, suffocation.
What is dangerous about detergent poisoning: symptoms, consequences.
What to do in case of hydrochloric acid poisoning: signs and treatment.
Inhalation of toxic substances may result in coughing, mucus discharge from the nose, sputum discharge, bronchospasm and inability to exhale. Toxic pulmonary edema is also possible. If the poison enters the gastrointestinal tract, then in case of chemical poisoning, symptoms may include abdominal pain, heartburn, and vomiting. Each class of substances is characterized by effects on certain organs and systems, so the signs of poisoning by chemicals are specific.
There are many classes of chemical compounds that are toxic to the body. The most common of them:
- Pesticides, herbicides, substances used in agriculture (see Nitrate poisoning).
- Chemical warfare agents, gaseous compounds.
- Medicines (atropine, physostigmine, antidepressants, barbiturates, opioid analgesics).
- Alcohol and ethyl alcohol substitutes.
- Poisonous mushrooms, plants, animals.
- Acids and alkalis.
Pesticides and chemical warfare agents contain organophosphorus compounds that have a toxic effect on the respiratory system. This chemical class connections causes activation parasympathetic system by blocking the destruction of acetylcholine in the body. The accumulation of acetylcholine in nerve endings leads to spasm of the bronchi, gastrointestinal tract, lacrimation and salivation, and diarrhea. Cardiac arrest is also possible.
Poisoning with certain drugs (Neostigmine, Physostigmine), as well as fly agaric mushrooms (see Fly agaric poisoning) also causes activation of the cholinergic system, which can lead to pulmonary edema. One of the signs of poisoning is constriction of the pupils (miosis).
Medicines from the group of anticholinergic drugs and belladonna alkaloids, on the contrary, cause dilation of the pupils. In this case, disruptions in the functioning of the heart are observed - tachycardia.
Important! Alcohol and surrogates cause liver damage - toxic hepatitis. Methyl alcohol has a detrimental effect on the central and peripheral nervous system; in case of poisoning, blindness and deafness occur.
Hydrocarbons and alcohols are toxic to the liver. Poisoning by them occurs due to unconventional methods of treatment (kerosene poisoning), working at gas stations. Inhalation poisoning through the respiratory tract leads to damage to the central nervous system and hallucinations.
Aflatoxins from molds that grow on bread can cause liver cell cancer. Toadstool poisons are the cause of toxic hepatitis (see Poisoning by toadstool).
Signs of chemical poisoning from heavy metals include nervous system disorders, hearing loss, and double vision. Possible mental disorders– with mercury poisoning, pathological shyness appears. Intoxication with lead compounds causes porphyria, renal failure, and spasmodic pain in the intestines.
Poisoning with caustic compounds such as acids and alkalis can lead to ulcerative lesions of the gastrointestinal tract. When toxic substances (acetic acid) penetrate into the blood through ulcerative defects in the mucous membrane, blood cells are destroyed. In this case, pale skin and jaundice are possible, associated with the death of red blood cells and the release of bilirubin.
Treatment of chemical poisoning
What to do in case of chemical poisoning? First of all, it is necessary to stop the flow toxic substances into the body. Principles of providing assistance in case of chemical poisoning:
- If poisoning occurs when chemical compounds enter the gastrointestinal tract, then you need to ask the victim or witnesses what poisoned the person.
- In case of poisoning with caustic compounds such as acids or alkalis, rinsing the stomach is prohibited in order to avoid damage to the esophagus and bleeding.
- To dilute the concentration of the substance, it is recommended to drink a glass of water - this is first aid for poisoning with chemicals through the stomach. Then you need to wait for medical help.
- If gastrointestinal poisoning is caused by hydrocarbon compounds, such as kerosene, turpentine, it is necessary to give a laxative (magnesia solution) to quickly remove toxic substances from the digestive tract.
- First aid for chemical poisoning by asphyxiating compounds - it is necessary to stop their access to the body by removing the victim from the contaminated area into fresh air or into a well-ventilated area. To return to a conscious state, ammonia is used by bringing it to the nose.
 For any chemical poisoning, first aid is to stop the access of the poison. It is necessary to take the victim to the hospital as quickly as possible. In a medical institution, in case of poisoning with acids and alkalis, the stomach is lavaged using a nasogastric tube and a Janet syringe connected to it. Acids are neutralized with a solution of soda, alkalis with a solution of various weak acids. Care must be taken in neutralization, as soda causes distension of the stomach walls.
For any chemical poisoning, first aid is to stop the access of the poison. It is necessary to take the victim to the hospital as quickly as possible. In a medical institution, in case of poisoning with acids and alkalis, the stomach is lavaged using a nasogastric tube and a Janet syringe connected to it. Acids are neutralized with a solution of soda, alkalis with a solution of various weak acids. Care must be taken in neutralization, as soda causes distension of the stomach walls.
In case of poisoning with organophosphorus compounds contained in pesticides, cholinesterase reactivators - Dipiroxime, Alloxime - or atropine-like drugs - belladonna alkaloids - are administered. Glutamic acid is also used in complex therapy.
If heavy metal poisoning occurs, Dimercaprol and Thioctic (lipoic acid) are used to remove them from the body. For intoxication with morphine-like compounds, the antidotes are Naltrexone and Naloxone.
In case of intoxication, detoxification therapy is carried out in the hospital using forced diuresis. Crystalloid solutions and glucose solution with the addition of diuretics (Lasix) are infused.
Peritoneal dialysis is also carried out: toxic compounds absorbed by the body are released into the abdominal cavity, which are washed off with saline.
Hemodialysis is a procedure for purifying blood through carbon filters or semi-permeable polyethylene membranes. It is used for poisoning by chemical compounds that lead to kidney failure, for example, lead poisoning.
Salmonella poisoning symptoms