Topic: FOOD POISONING.
TEST QUESTIONS
1. Definition of food poisoning. Common signs of food poisoning.
2. Classification of food poisoning.
3. Toxic infections. Etiology, clinic. Conditions necessary for the occurrence of toxicoinfections.
4. Prevention of toxic infections.
5. Staphylococcal toxicosis, clinic, etiology and prevention.
6. Botulism, clinic, epidemiology, prevention.
7. Mycotoxicosis. Etiology, clinic and prevention.
8. Mushroom poisoning. Clinic and prevention.
9. Poisoning by products of animal and vegetable origin. Their features and prevention.
10. Investigation of food poisoning.
1. Introduction
food poisoning- these are acute (less often chronic) non-contagious (non-contagious) diseases resulting from the consumption of food contaminated with microorganisms or containing toxic substances of a microbial or non-microbial nature.
Food poisoning is a group of diseases of different etiology (causative factor) and clinical picture.
In a single group they are united by a number of common features. Common signs of food poisoning include:
acute, sudden onset of the disease;
simultaneity of the onset of the disease in a group of individuals;
connection of diseases with the consumption of any food product;
territorial limitation of diseases by the place of consumption or the place of purchase of the food product;
cessation of the occurrence of new cases of diseases after the destruction or withdrawal of the guilty product;
lack of transmission causative factor food poisoning from a sick person to a healthy one. This feature distinguishes food poisoning from infectious diseases.
2. Classification of food poisoning
According to the etiological (causal) principle, food poisoning is divided into three groups:
microbial;
non-microbial;
unknown etiology.
food poisoning microbial origin according to the pathogenetic principle are divided into three groups:
toxic infections;
toxicosis (bacterial and mycotoxicosis);
poisoning of mixed etiology.
food poisoning non-microbial origin include three groups of diseases:
poisoning by poisonous plants and animal tissues;
poisoning by plants and animal tissues, poisonous under certain conditions;
chemical poisoning.
For food poisoning unknown etiology Gaff's (Yukst's) disease, which occurs when eating lake fish in certain parts of the world in certain years, is one of them. It is assumed that the toxic substance is contained in fish fat and is not inactivated (not neutralized) during heat treatment.
3. Toxic infections
Etiological factors are potentially pathogenic microorganisms.
This is a whole group of microorganisms, including several species: Echerichie coli, Proteus, Clostridium Perfringens, Bacillus cereus, Klebsiella, Aeromonas, etc.
source toxicoinfection is a person or animals.
transfer factor is a food product that plays an important role in the occurrence of the disease, as it is a substrate (environment) for the reproduction of microorganisms.
Incubation period lasts several hours.
Clinical course disease is determined by the type and type of microorganism.
Most common symptoms toxicoinfections are the phenomena of gastroenteritis and fever.
Diagnostics carried out according to clinical symptoms and confirmed by laboratory tests. Excrements, vomit, washings, blood, urine, food residues are subjected to laboratory research.
For retrospective diagnosis of food poisoning, the results of serological reactions are used.
Basic principles prevention toxic infections are reduced to:
prevention of contamination of food with potentially pathogenic microbes;
prevention of microbial growth in food products;
destruction of microbes during heat treatment of products.
The main activity aimed at source Potentially pathogenic microorganisms should be considered control over the observance of the rules of personal and industrial hygiene by employees of food enterprises. An important role is played by automation and mechanization of food production processes, veterinary supervision at slaughterhouses and meat processing plants.
To interrupt the routes of contamination of food products, sanitary requirements have been established for the factors of transmission of pathogens of food poisoning:
Delivery of food products by special transport.
Labeling of equipment and its use strictly for its intended purpose.
Compliance with the flow of production.
Control over the sanitary condition of industrial premises.
The prevention of microbial growth is achieved by observing the technology of food processing, using cold at all stages of the technological process, observing the temperature regime of cooking, pasteurization, sterilization of products, observing the deadlines for implementation finished products.
Poisoning- This is a pathological condition in which bacteria, any toxins or other toxic substances enter the human body. These substances can enter the body in various ways ( with food, inhaled air or through the skin), however, all of them certainly cause damage to various organs and disruption of their functions, which is accompanied by corresponding clinical manifestations and creates a danger to human health and life.Classification of poisoning
In clinical practice, it is customary to classify poisoning according to several criteria. This helps doctors determine the cause of the disease, as well as make a diagnosis and prescribe the correct treatment.Depending on the route of entry into the body, there are:
- Food poisoning- when toxins or poisons enter the human body along with the food taken ( through the gastrointestinal tract).
- Poisoning through the respiratory tract- when the toxin enters the body with the inhaled air ( in the form of steam or gas).
- Percutaneous poisoning- when toxins enter the skin or mucous membranes of a person, and through them are absorbed into the systemic circulation.
- Poisoning, in which the toxin is administered directly intravenously or intramuscularly.
- food intoxication ( food poisoning) - in this case, the disease is caused by eating foods that have been contaminated with any dangerous bacteria or their toxins.
- Gas poisoning- develops when inhaling any toxic gases.
- Chemical poisoning- chemicals include various toxins and poisons, which under normal conditions should not enter the human body.
- Poisoning with caustic substances ( acids or alkalis) - allocated to a separate group, due to the peculiarities of their clinical manifestations.
- Medicine poisoning- develops with misuse medicines.
- Ethanol poisoning ( alcohol, which is part of all alcoholic beverages) - also allocated to a separate group, which is explained by the specific effect of alcohol on the human body.
- Acute poisoning - develops with a single intake of a large dose of a toxic substance into the body and is accompanied by the rapid appearance and rapid development of clinical symptoms.
- chronic poisoning- occurs with prolonged intake of small doses of toxin in the body and may be asymptomatic for some time, but ultimately also leads to dysfunction of vital organs and systems.
Causes, types and pathogenesis ( development mechanism) food poisoning, infections and toxicoinfections
 As follows from the above, poisoning can develop when various substances enter the body. pathogenic bacteria, as well as toxic substances produced by them ( in the latter case we are talking about toxic infection). Each of these substances can affect the tissues and organs of the body in its own way, causing corresponding changes in them, which is accompanied by characteristic clinical manifestations and requires specific treatment. That is why it is extremely important to determine the type of poisonous substance in a timely manner and begin treatment. This will prevent the development of complications and save the life of the patient.
As follows from the above, poisoning can develop when various substances enter the body. pathogenic bacteria, as well as toxic substances produced by them ( in the latter case we are talking about toxic infection). Each of these substances can affect the tissues and organs of the body in its own way, causing corresponding changes in them, which is accompanied by characteristic clinical manifestations and requires specific treatment. That is why it is extremely important to determine the type of poisonous substance in a timely manner and begin treatment. This will prevent the development of complications and save the life of the patient. spicy food ( intestinal) poisoning in an adult ( expired food, meat, fish, eggs, milk, cottage cheese)
Acute food poisoning food intoxication) is a group of diseases in which, along with food, a person swallows any microorganisms ( bacteria, pathogenic fungi) or toxins released pathogenic microorganisms. If such bacteria or their toxins enter the gastrointestinal tract ( gastrointestinal tract), they affect the mucous membrane of the stomach and intestines, leading to the appearance of classic signs of poisoning ( abdominal pain, nausea, diarrhea and so on). Moreover, these toxins can be absorbed through the gastrointestinal mucosa and enter the systemic circulation, affecting distant organs and leading to complications.Food poisoning can be caused by:
- Spoiled meat. Meat is an ideal breeding ground for the growth and reproduction of pathogenic bacteria ( staphylococci, salmonella, E. coli and others). These bacteria may be present in meat products initially ( for example, if the slaughtered animal was infected with some kind of infection). In this case, infectious agents or their toxins ( bacteria released into the environment during growth) can enter the human body through the consumption of insufficiently processed food ( that is, undercooked or undercooked meat). At the same time, bacteria can develop in already cooked but improperly stored meat. If it is kept out of the refrigerator for several hours or days, the number of pathogens in it may become sufficient to cause a foodborne infection.
- Fish. Fish poisoning can occur for the same reasons as meat poisoning ( i.e. improper processing and improper storage of fish products). In addition, some exotic varieties of fish may contain toxic substances ( e.g. pufferfish, groupers, barracudas). In this case, the clinical manifestations of poisoning will depend on the type of poison that has entered the body. So, for example, the poison contained in puffer fish can cause paralysis of all muscles and respiratory arrest, which without medical care will inevitably lead to death. In other cases, the symptoms of poisoning may be similar to common foodborne infections.
- eggs. The risk of egg poisoning is increased if waterfowl eggs are eaten ( ducks, geese). The fact is that salmonella bacteria may be present in some polluted water bodies. It can get into the meat and eggs of waterfowl, and with them ( with improper heat treatment, that is, with the use of raw eggs or soft-boiled eggs) can enter the human body. Having penetrated the intestines, salmonella releases a special toxin that affects the mucous membrane intestinal wall, causing clinical manifestations of intestinal infection ( diarrhea, abdominal pain, etc.).
- Milk. Poisoning from fresh domestic milk can occur if the animals that produce it ( goats, cows) are kept in unsanitary conditions. At the same time, various pathogenic bacteria may be present in the udder area of animals ( staphylococci, E. coli and so on) that will enter the milk during milking. If you drink such milk in its raw form, there is a high probability of developing food poisoning. Moreover, it is worth noting that some animals can be carriers of pathogens especially dangerous infections. So, for example, when drinking cow's milk, you can become infected with brucellosis, an infection caused by pathogenic microorganisms ( brucella) and accompanied by damage to many body systems.
- Cottage cheese. Cottage cheese, like any lactic acid product, is an ideal breeding ground for various pathogenic bacteria. If the product is left out of the refrigerator for a long time, the number of bacteria in it increases significantly ( contributes to this heat environment in which the rate of bacterial growth increases). If you eat such cottage cheese, signs of an intestinal infection may appear.
Poisoning by poisonous plants ( bleached, hemlock), mushrooms ( pale grebe, fly agaric), berries ( belladonna, wolfberry)
Many plants contain substances that are toxic to the human body. The use of such plants or their fruits ( in particular, wolf berries - belladonna, wolfberry) in food may be accompanied by symptoms of food poisoning, as well as other specific manifestations (depending on what toxin was contained in the eaten plant).Poisoning can be caused by eating:
- Beleny. The toxicity of this plant is due to its constituent substances, in particular atropine and scopolamine. When ingested, they cause general weakness, dry mouth, intense thirst, emotional and motor agitation, and dizziness. In severe cases, vision and breathing problems, loss of consciousness, convulsions, and death may occur.
- Hemlock. The toxicity of this plant is due to its constituent substance - koniin. This is a strong poison, which, when it enters the gastrointestinal tract, is quickly absorbed through the mucous membrane and enters the bloodstream, affecting the central nervous system. This is manifested by progressive paralysis, in which a person loses all types of sensitivity, and also cannot move his arms or legs. The cause of death is usually paralysis of the respiratory muscles, causing the patient to stop breathing.
- Pale grebe ( fly agaric). A toxin found in some fly agarics ( in particular in pale grebe) has the ability to hit ( destroy) cells of the liver and other tissues of the body, which is accompanied by a violation of the functions of vital organs and systems. Without timely assistance, a person may die from cardiovascular or liver failure.
- Belladonna berries. Belladonna berries also contain atropine and scopolamine. Their poisoning has the same symptoms as henbane poisoning.
- Wolfberry berries. Toxic substances of the wolfberry ( meserine and daphne) are found in all parts of the plant ( in fruits, root, leaves). When eating fruits, these toxins cause a burning sensation in the mouth. Then there is severe pain in the upper abdomen, nausea and vomiting, in severe cases, convulsions occur.
Botulinum toxin poisoning
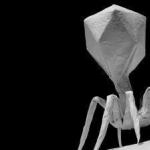
The cause of the disease is a toxin produced by the microorganism Clostridium. Disputes ( inactive forms) of this pathogen can persist for a long time in soil, silt, animal carcasses, and so on. Once in the human body, clostridium itself does not cause the development of infection, since they can only multiply under anaerobic conditions ( that is, when total absence oxygen). Botulinum toxin infection can occur when eating poorly processed canned food ( vegetable, meat) prepared at home. In this case, in a hermetically sealed jar, clostridia begin to actively multiply, releasing botulinum toxin into the environment, which is one of the most powerful poisons known to mankind.After entering the human gastrointestinal tract, botulinum toxin is not destroyed by acidic gastric juice, as a result of which it is easily absorbed through the mucous membrane. Entering the systemic circulation, this toxin reaches the tissues of the central nervous system and affects them, as a result of which characteristic clinical manifestations of the disease occur.
Botulinum toxin poisoning can manifest itself:
- occasional vomiting and abdominal pain in the first hours after eating the contaminated product);
- respiratory failure;
- visual impairment;
- increased blood pressure;
- muscle weakness;
- urination disorders and so on.
mold poisoning
Molds are fungal microorganisms that can grow on or inside various foods. When eating moldy foods, fungi can enter the gastrointestinal tract and lead to symptoms of poisoning ( nausea, vomiting, diarrhea). This is due to the fact that many fungi secrete so-called mycotoxins, which have a negative effect on various systems organism.In addition, some molds have antibacterial activity, that is, they destroy various bacteria. Under normal conditions, the intestines of a healthy person contain many bacteria that take part in the process of digestion. If mold is poisoned, these bacteria can be destroyed, resulting in disruption or slowing down the process of digestion of food. It can also lead to bloating, diarrhea or constipation, abdominal pain, and other symptoms.
It is also worth noting that mold can be poisoned through the respiratory tract ( by inhaling particles of pathogenic fungi - for example, in pulmonary aspergillosis). At the same time, pathogenic fungi affect the lung tissue, as a result of which frequent coughing with the release of red bloody sputum ( hemoptysis), shortness of breath ( feeling short of breath), fever, chest pain, and so on.
Vitamin poisoning
Vitamin poisoning can be observed with their frequent use in large doses. However, the clinical manifestations of the disease may vary ( depending on what vitamin the person was poisoned with).Poisoning can occur with an overdose:
- Vitamin A. Since this vitamin affects the organ of vision, one of the first signs of poisoning will be double vision. Also, there may be nausea and vomiting due to the action of the vitamin on the nervous system. Patients may complain of increased drowsiness, headache, fever. Sometimes a skin rash may occur. After stopping the use of the vitamin, all the described symptoms disappear within 2 to 3 days. With chronic use of vitamin A in large doses, skin itching, hair loss, dryness and flaking of the skin can be noted.
- Vitamin D Vitamin D poisoning can also be acute ( when taking a very large dose) or chronic ( when used in high doses for a long time). In acute poisoning, patients complain of general weakness, nausea and vomiting, headaches and dizziness. In severe cases, there may be an increased heartbeat, fever, convulsions. With chronic intoxication with vitamin D, there is a decrease in appetite, increased irritability, and indigestion ( nausea, vomiting, diarrhea, or constipation). If left untreated, irreversible damage to the cardiovascular, bone and other body systems can occur.
- Vitamin C. Long-term use this vitamin in large doses, it can cause damage to the central nervous system, which will be manifested by insomnia, fever and a feeling of heat, headaches, dizziness, nausea. There may also be dryness of the skin and mucous membranes throughout the body.
- Vitamin B1. Poisoning with this vitamin can provoke a feeling of weakness or fatigue, insomnia, headaches, loss of appetite. In severe cases, there may be damage to internal organs ( kidneys, liver).
- Vitamin B6. Chronic poisoning with this vitamin can be accompanied by damage to the peripheral nervous system, impaired sensitivity in the limbs, a tendency to develop seizures and weight loss.
- Vitamin B12. The use of this vitamin in large doses can disrupt the functioning of the thyroid gland ( an organ that produces hormones that regulate the body's metabolism). It has also been noted that prolonged chronic overdose may contribute to the development of malignant tumors.
- folic acid. An overdose of this vitamin is manifested by nausea and vomiting, increased nervous irritability and insomnia, and headaches. In severe cases, there may be damage to the cardiovascular system and kidneys.
- Vitamin E. Chronic poisoning with this vitamin is manifested by headaches, general weakness and increased fatigue, nausea, and is also accompanied by a decrease in the body's defenses ( increased risk of microbial infections).
protein poisoning
Eating a large amount of protein foods ( predominantly meat) may be accompanied by an increase in the concentration of proteins in the blood. This can lead to disruption of the functioning of various organs and systems.Protein poisoning can manifest itself:
- Nausea or vomiting – protein food inhibits peristalsis motor activity) of the gastrointestinal tract, in connection with which the digestion process is disturbed.
- Bloating- due to impaired intestinal motility and the development of gas-forming microflora.
- insomnia- protein food stimulates the central nervous system, in connection with which there may be a violation of the process of falling asleep, as well as increased nervous excitability or irritability.
- An increase in body temperature– it is also associated with the excitation of the central nervous system.
- Darkening of the urine- this is due to the release of by-products of protein metabolism through the kidneys.
water poisoning ( water poisoning)
water poisoning ( hyperhydration), in fact, is not a poisoning. This is a pathological condition of the body, in which there is a violation of water-electrolyte metabolism. The reason for this may be severe vomiting, accompanied by loss of electrolytes ( if at the same time a person replenishes the loss of fluid with water that does not contain electrolytes), impaired renal function ( in this case, the fluid is not excreted from the body), excessive intravenous fluids, and so on. In addition, water poisoning can be observed when it is taken in excess for a short period of time. So, for example, drinking 2.5 - 3 liters of pure water for an hour can lead to overhydration, disruption of water and electrolyte balance, and even death.salt poisoning ( sodium)
From a chemical point of view, table salt is sodium chloride, that is, it contains the trace elements sodium and chlorine. When a large amount of salt is consumed in a short period of time, a person may develop hypernatremia - a pathological condition accompanied by an increase in the concentration of sodium in the blood ( norm - 135 - 145 mmol / liter). This can lead to disruption of the functioning of vital organs, as well as provoke the development of formidable complications from the central nervous system.One of the first symptoms of salt poisoning is thirst ( desire to drink water). This is explained by the fact that an increased concentration of sodium in the blood is recorded by special sensitive cells at the level of the brain. In order to "dilute" the blood and reduce the sodium concentration in it, the body needs to get a large amount of fluid from the outside, as a result of which a strong ( irresistible) thirst.
Other signs of salt poisoning are:
- general weakness;
- disorientation in time and space;
- loss of consciousness;
- increased neuromuscular excitability;
- wrinkling and dryness of the skin ( due to the release of fluid from the cells into the vascular bed).
Poisoning with mineral fertilizers ( nitrates)
Nitrates are chemical substances (salts of nitric acid), which are used as fertilizers. Nitrates can be found in large quantities in foods that have been processed by them during the growing process. When entering the human gastrointestinal tract, nitrates turn into so-called nitrites - toxic substances that affect red blood cells, making it impossible for them to transport oxygen. At the same time, a person begins to suffer from oxygen starvation ( fatigue, headaches, dizziness). In severe cases, death is possible.Poisoning with rat poison
In order to combat rats and other small rodents, special poisonous substances are used. After entering the body along with the bait ( food) these poisons disrupt the functioning of the vital organs of rodents, which leads to their death. It is worth noting that all these poisons are to some extent toxic to humans if they get into his gastrointestinal tract.A person can get poisoned:
- Naphthylthiocarbamide. If a person eats this poison, after a few minutes or hours he will have severe vomiting, as a result of which part of the toxin will be removed from the gastrointestinal tract. If the toxin enters the systemic circulation in high concentration, it can cause damage to the circulatory system, as well as the liver and lungs, which can lead to death of a person.
- Ratindan. When ingested, the active substance of this poison can be absorbed into the systemic circulation, where it disrupts the activity of the blood coagulation system ( which normally regulates hemorrhage control). Immediately after poisoning, the patient may experience nausea or vomiting once. After a few days, there may be frequent nosebleeds, bleeding gums, prolonged bleeding after injuries, and so on. In more severe cases, hemoptysis may occur ( coughing up blood from the lungs), as well as the appearance of blood in the stool and urine. If you do not start specific treatment, after a few days you may experience a feeling of general fatigue and lethargy, which is associated with chronic blood loss. Death can occur from a pronounced decrease in the concentration of red cells in the blood and oxygen starvation brain, as well as damage to other vital organs ( liver, kidney, central nervous system, respiratory system and so on).
- Brodifacoum. This drug also disrupts the activity of the blood coagulation system. Signs of poisoning them are similar to those of ratindan poisoning.
alcohol poisoning ( ethyl alcohol, vodka, wine, beer, surrogates)
Poisoning alcoholic drinks can be observed when using them in large quantities, as well as when drinking low-quality alcoholic beverages. It should be noted that active "intoxicating") the substance of all alcoholic beverages is ethyl alcohol ( ethanol). The rate of development of intoxication, as well as the severity of symptoms of poisoning, depends on its concentration. So, for example, the concentration of ethanol in vodka is 40%, while in beer it is up to 8-10%. It follows that the symptoms of ethanol intoxication will occur more quickly when drinking large amounts of vodka than beer or other ( less strong) alcoholic beverages.Ethyl alcohol poisoning can manifest itself:
- Nausea and vomiting. These are natural protective reflexes, the purpose of which is to remove excess toxic substances from the body, as well as to prevent its further intake.
- Dizziness and confusion. This symptom is due to the effect of alcohol on brain cells.
- Nervous excitement or drowsiness. In the initial stages of intoxication, alcohol stimulates the central nervous system ( CNS), in connection with which the patient may behave excitedly or aggressively, see hallucinations ( something that doesn't really exist) and so on. With an increase in the concentration of ethanol in the blood, the activity of the central nervous system is inhibited, and therefore drowsiness and lethargy appear. In severe cases, a person can fall into a coma - a life-threatening condition in which the patient does not respond to external stimuli.
- Redness of the skin ( especially faces). Ethyl alcohol causes the expansion of superficial blood vessels, causing blood to flow to the skin, changing its color.
- The presence of a specific alcoholic smell. Alcohol is partially excreted through the lungs ( in the form of vapor). The higher its concentration in the blood, the more pronounced will be the alcoholic smell from the patient's mouth. This symptom will distinguish alcoholic coma ( extreme depression of consciousness) from other diseases in which a person can also lose consciousness.
- Breathing disorder. This may be due to damage to the central nervous system, as well as blockage of the respiratory tract by vomit ( if vomiting occurred while the person was unconscious).
Methyl alcohol poisoning
Methyl alcohol ( methanol) is used in chemical industry as a solvent and for other purposes. It also has a moderate intoxicating effect, but much less pronounced than ethyl alcohol. It is strictly forbidden to eat methanol, since the products of its metabolism ( in particular formaldehyde and formic acid) are extremely toxic to the body. Accumulating in tissues and organs, they can cause damage to the central nervous system, the organ of vision, the liver and the cardiovascular system, and in severe cases lead to the death of the patient. The lethal dose of methanol is 25 - 100 ml ( depending on the age and weight of the person).Methyl alcohol poisoning manifests itself:
- Nausea, vomiting, headaches and dizziness- the mechanism of occurrence of these symptoms is the same as with ethyl alcohol poisoning.
- Paroxysmal abdominal pain- they are caused by the accumulation of by-products of methanol metabolism in the tissues of the gastrointestinal tract and a violation of the contractile activity of the stomach and intestines.
- visual impairment ( up to its complete loss.) - the development of this symptom is also due to the toxic effect of formaldehyde and formic acid at the level of the optic nerve ( innervates the retina of the eye, which perceives light).
- Loss of consciousness, convulsions and coma- develop as a result of severe intoxication of the body with formic acid, which can lead to the death of the patient within a day.
Symptoms and signs of food poisoning and toxic infections
 At the initial stages of the development of the disease, the symptoms and signs of all food poisoning are similar to each other. The entry of a toxic substance into the body triggers a series of protective reactions aimed at removing it from the body. In the later stages of development, specific signs of poisoning may appear, depending on which toxin the patient has eaten ( violations of the functions of the cardiovascular and respiratory systems, damage to the liver, kidneys, and so on).
At the initial stages of the development of the disease, the symptoms and signs of all food poisoning are similar to each other. The entry of a toxic substance into the body triggers a series of protective reactions aimed at removing it from the body. In the later stages of development, specific signs of poisoning may appear, depending on which toxin the patient has eaten ( violations of the functions of the cardiovascular and respiratory systems, damage to the liver, kidneys, and so on).Food poisoning can manifest itself:
- nausea and vomiting;
- diarrhea ( loose stools, diarrhea);
- pain in the abdomen;
- an increase in body temperature;
- headaches;
- dizziness;
- body intoxication.
Nausea and vomiting
As mentioned earlier, nausea and vomiting are protective mechanisms that should slow down the entry of toxic substances into the systemic circulation. Once the toxin or poison enters the gastrointestinal tract ( gastrointestinal tract), it almost immediately begins to be absorbed through the gastric mucosa ( a little later through the intestinal mucosa). This leads to certain changes in the patient's blood, triggering nervous and hormonal defense reactions.Under normal conditions, after eating, peristalsis is activated ( motor activity) gastrointestinal tract. This promotes mixing of food with digestive juices and absorption of nutrients. As soon as the body "understands" that poisoning has occurred, the motility of the gastrointestinal tract immediately stops. At the same time, food ceases to be absorbed, stagnates in the stomach and stretches it, which creates an unpleasant feeling of nausea. After that, the so-called anti-peristaltic waves appear, that is, such muscle contractions of the gastrointestinal tract that push its contents in the opposite direction ( that is, from the small intestine to the stomach, and from the stomach through the esophagus to the oral cavity). This is how vomiting occurs, the purpose of which is to remove potentially hazardous products from the gastrointestinal tract, which will prevent further absorption of toxins.
diarrhea ( loose stools, diarrhea)
Diarrhea can occur due to the activity of pathogenic microorganisms that have entered the gastrointestinal tract ( gastrointestinal tract) along with any products. So, for example, when consuming salmonella-infected ( pathogenic microorganisms) food, the toxins produced by them stimulate the release of salts and water into the intestinal lumen, which is manifested by massive watery diarrhea, which can be repeated several dozen times a day. In this case, the body loses a large amount of fluid and electrolytes, which can endanger the life of the patient.In other cases, the development of diarrhea may not be associated with the pathogen itself, but is a consequence of the development of a pathological process in the gastrointestinal tract. The fact is that after the onset of poisoning, the motility of the stomach and intestines slows down, as a result of which the digestion process is disturbed. Food from the small intestine and stomach can be removed from the GI tract by vomiting, while the contents of the large intestine remain in it. Under normal conditions, a certain part of the water is absorbed precisely through the mucous membrane of the final sections of the gastrointestinal tract ( that is, through the mucosa of the large intestine). However, due to the slowdown in peristalsis, the absorption process is also disturbed, as a result of which water and intestinal contents are excreted through the anus in the form of loose stools or diarrhea. Such diarrhea usually recurs 1-2 times and does not pose a danger to the patient's life, since the loss of fluid and electrolytes is not as pronounced as in the first case.
Stomach ache ( stomach, intestines)
Pain in case of poisoning may be associated with damage to the mucous membrane of the stomach or intestines. The fact is that under normal conditions it is covered with a thin layer of mucus, which protects it from the traumatic effects of food products, as well as from sour gastric juice. In case of poisoning, the secretion of this mucus is disrupted, which leads to damage to the gastric mucosa and its inflammation ( gastritis). As a result, the patient may feel acute, paroxysmal pain in the upper abdomen, which occurs with a frequency of 1 to 2 times per minute and lasts from 5 to 20 seconds. The mechanism of pain in this case is due to peristaltic ( contractile) waves of the muscles of the gastrointestinal tract ( gastrointestinal tract). When these muscles contract, the nerve endings of the stomach wall are irritated, which is felt by the patient as a cutting, poorly localized pain ( the patient cannot pinpoint exactly where it hurts).Drawing pains in the lower abdomen may be due to the transition of the infectious process to the large intestine, which will be accompanied by the appearance of diarrhea. Under normal conditions, the peristaltic wave is accompanied by a short-term ( for 3 - 5 seconds) muscle contraction, which helps to push the intestinal contents. With the development of poisoning, this function is impaired, as a result of which the muscular contractions of the intestine become too long ( that is, the muscles remain in a contracted state for 10 to 20 seconds or more). In this case, the metabolism in them is disturbed, which is accompanied by the appearance of characteristic pains.
Increase in body temperature
An increase in body temperature during poisoning is also a protective reaction of the body. The fact is that many pathogenic microorganisms and their toxins can only exist at a certain temperature, and when the ambient temperature rises, they die or are destroyed. That is why, in the process of evolution, the body developed this defensive reaction- as soon as any foreign substance enters the systemic circulation, a number of biochemical processes are launched, the final result of which is an increase in body temperature.With any food poisoning, body temperature will rise to at least 37 to 38 degrees during the first 6 to 12 hours after eating bad or contaminated food. If the body's defenses cope with the infection, body temperature returns to normal within a day. At the same time, it is worth noting that infection with some pathogenic microorganisms or toxins can be accompanied by an extremely pronounced increase in temperature ( up to 39 - 40 and more degrees).
Headache
Headache can accompany poisoning if toxic substances from the gastrointestinal tract enter the bloodstream in large quantities. This activates the body's immune system, the purpose of which is to find and destroy all foreign agents that have entered the systemic circulation. During the operation of this system, so-called biologically active substances are produced that fight foreign microorganisms and their toxins. However, these substances also have negative effects, in particular a vasodilating effect. When toxic substances enter the systemic circulation, as well as when exposed to biologically active substances, an expansion of the blood vessels of the brain is noted, as a result of which part of the fluid from the bloodstream passes into the surrounding tissues. At the same time, the meningeal membrane of the brain, rich in sensitive nerve endings, is also stretched. All this leads to the occurrence of severe headaches, which can appear within the first day after the onset of poisoning and subside only after the patient's condition is normalized ( that is, after removal of foreign toxins and subsidence of immune responses).It should be noted that alcohol poisoning headache also occurs due to the expansion of blood vessels and swelling of brain tissue. However, in this case, ethyl alcohol itself has a vasodilating effect ( contained in alcoholic beverages), and the body's immune system is not involved in the pathological process.
Dehydration
Dehydration is a pathological condition characterized by the loss of large amounts of fluid from the body. The cause of dehydration in case of poisoning can be frequent vomiting or diarrhea, during which a large amount of fluid is removed from the body. Moreover, an increase in body temperature can contribute to the development of dehydration, since in this case a person begins to sweat, and along with sweat, loses fluid.Since it is not always possible to recover losses ( for example, if the patient vomits again when taking fluids), already 4-6 hours after the onset of the disease, the patient may show the first signs of dehydration. If treatment is not started on time, the body will continue to lose fluid and vital electrolytes ( chlorine, sodium and others), which over time can lead to dysfunction of vital organs or even death.
Dehydration manifests itself:
- Decreased elasticity and dryness of the skin. Due to the fact that the liquid leaves the skin, it becomes dry and less elastic, loses its usual luster.
- Dryness of mucous membranes. This symptom is clearly visible in the oral cavity, tongue and lips ( mucous membranes become dry, and then covered with characteristic crusts).
- Pale skin. Due to the decrease in the volume of circulating blood, there is a "closure" of peripheral blood vessels ( especially in the skin), which allows you to maintain blood circulation in vital organs ( brain, heart, liver) at normal levels. The pallor of the skin in this case occurs due to the fact that the amount of blood in its vessels decreases.
- Retraction of the eyeballs. Under normal conditions, a layer of adipose tissue is located between the eyeball and the back wall of the orbit. It supports and fixes the eye, preventing its damage in case of injury. During dehydration, fluid from adipose tissue is also removed, as a result of which it ( adipose tissue) becomes thinner, and the eyeballs are displaced deep into the orbits.
- Rapid heartbeat. With moderate or severe dehydration, the volume of circulating blood decreases. To compensate for the losses and maintain the blood supply to the organs at a normal level, the heart has to pump blood at a faster rate.
- Decreased amount of urine. As the amount of fluid in the body decreases, protective mechanisms are launched, the purpose of which is to prevent further loss of water. One of these mechanisms is a decrease in the rate of urine formation in the kidneys.
Dizziness
Dizziness can be one of the first symptoms of poisoning by certain plants and fungi, as well as poisoning with alcoholic beverages or surrogates. The reason for the development of this symptom in this case is the direct toxic effect exerted by toxic substances on the brain. At the same time, it is worth noting that dizziness can also occur with other poisonings, indicating their severe course. So, for example, with severe intoxication of the body, accompanied by dehydration ( fluid loss) and a decrease in blood pressure, there may be a violation of the blood supply to the brain cells, which will be manifested by dizziness, darkening of the eyes, or even loss of consciousness.Body intoxication
General intoxication syndrome is a complex of symptoms that develop in the body with any food poisoning ( whatever its cause). The occurrence of this syndrome is due to the activation of the immune system and its fight against foreign agents. After removal of all toxic substances from the body, signs of general intoxication disappear ( along with the normalization of body temperature).Intoxication of the body can manifest itself:
- general weakness;
- decrease in working capacity;
- retardation of thinking;
- drowsiness;
- chills ( feeling of coldness in the extremities);
- increased heartbeat;
- rapid breathing.
Symptoms of food poisoning in children
Mechanisms for the development of food poisoning in children do not differ from those in adults. At the same time, it is worth remembering that in early childhood poisoning can develop faster and be more severe than in an adult. This is due to the imperfection of the protective forces and the immune system of the child's body, as well as its low compensatory capabilities. So, for example, after 2 - 4 bouts of vomiting or diarrhea, a child may develop dehydration, while in an adult this will not cause any serious disorders. That is why it is extremely important to timely identify the first signs and symptoms of poisoning and begin therapeutic measures without waiting for the baby's condition to worsen and complications develop.Poisoning in a child can manifest itself:
- Tearfulness- this is especially pronounced in young children who do not yet know how to express their feelings in words ( if the child is hurt or ill, he cries).
- Increased motor activity- the child may be restless, agitated.
- Defensive position in bed- in case of poisoning, children also experience abdominal pain, and therefore take characteristic posture"embryo" ( knees and elbows are pressed to the stomach, and when you try to unbend or raise them, they begin to cry).
- Nausea, vomiting and diarrhea- the causes of these symptoms are the same as in case of poisoning in adults.
- An increase in body temperature- the temperature reaction in children may be more pronounced, as a result of which from the first day the temperature can rise to 38 - 39 degrees.
- Drowsiness and impaired consciousness- these signs occur with severe intoxication of the body and require immediate hospitalization.
- convulsions ( seizures) - they can occur when the child's body temperature rises above 40 degrees and is associated with impaired functioning of the nervous system.
Does blood pressure rise with poisoning?
Under normal conditions arterial pressure (HELL) of a person is 120/80 millimeters of mercury. By itself, food poisoning does not cause an increase in blood pressure. At the initial stage of the development of the disease, when the patient develops severe vomiting, diarrhea and abdominal pain, his blood pressure may slightly exceed the norm. This is due to an increase in pressure in the abdominal cavity ( during vomiting), as well as the activation of the body's defense systems, one of the manifestations of which is the narrowing of blood vessels and an increase in blood pressure. After the vomiting subsides, the pressure usually returns to normal within an hour.At the same time, it should be noted that when severe course poisoning ( that is, with the development of dehydration and other complications) may experience a drop in blood pressure below normal. This is an extremely dangerous symptom, indicating the depletion of the body's compensatory capabilities. This can disrupt the blood supply to vital organs ( first of all, the brain), as a result of which a person may experience dizziness, lose consciousness, or even fall into a coma.
Can poisoning occur without fever?
Most poisonings are characterized by an increase in body temperature, however this symptom does not always occur. As mentioned earlier, an increase in temperature is a protective reaction of the body that develops when foreign microorganisms or their toxins enter the systemic circulation. However, in some poisonings, the toxic agent does not enter the systemic circulation, but exerts its pathogenic effect only at the level of the intestinal mucosa. In this case, the patient may experience some characteristics poisoning ( nausea, vomiting, abdominal pain), but body temperature may remain normal or rise slightly ( up to 37 - 37.5 degrees).The severity of poisoning ( mild, moderate, severe, fatal)
The severity of poisoning depends on the severity of damage to vital organs and systems that develops after the ingestion of a toxic substance into the body.Depending on the severity, there are:
- Light poisoning. The disease does not cause dysfunction of vital organs. Therapeutic measures can be done at home.
- Moderate poisoning. The general condition of the patient is disturbed, which is manifested by moderate disorders of the functions of vital organs ( increased breathing and heart rate, fluctuations in blood pressure, increased body temperature, and so on). Although the patient's life is not in danger, the treatment of such poisoning is recommended to be carried out in a hospital, since otherwise the patient's general condition may worsen and complications may develop.
- Severe poisoning. In this case, intoxication of the body leads to severe dysfunction of vital organs, which can be manifested by a drop in blood pressure, impaired consciousness, lack of urine ( due to dehydration and impaired urinary function of the kidneys) and so on. Treatment of such patients should be carried out exclusively in the hospital, as otherwise the risk of complications and death is high.
- Extremely severe poisoning. In this case, the violation of the functions of vital organs is so pronounced that in order to save a person's life, he must be immediately hospitalized in the intensive care unit and begin specific treatment. Otherwise, death is inevitable.
- Fatal poisoning. In this case, poisoning with any substances leads to the death of the patient, despite the best efforts of doctors ( if any, that is, if the patient managed to be hospitalized
CLASSIFICATION OF FOOD POISONING
Food poisoning refers to diseases of various nature that occur when eating food containing pathogens or their toxins or other non-microbial substances that are toxic to the body.
Unlike intestinal infections food poisoning is not contagious, not transmitted from a sick person to a healthy one.
These diseases can occur in the form of mass outbreaks, covering a significant number of people, as well as group and individual cases. Food poisoning is characterized by sudden onset, short current. The occurrence of poisoning is often associated with the consumption of a single food product containing a harmful principle. In cases of prolonged consumption of food products containing harmful substances (pesticides, lead), food poisoning can also occur in the form of chronic diseases.
Clinical manifestations of poisoning are more often in the nature of disorders of the gastrointestinal tract. However, in some cases these symptoms are absent (with botulism, poisoning with lead compounds, etc.). The most sensitive to food poisoning are children, the elderly and patients with gastrointestinal diseases. Their poisoning often occurs in a more severe form.
According to the new classification approved by the Ministry of Health of the Russian Federation (compiled by a “group of specialists in food hygiene - I. A. Karplyuk, I. B. Kuvaeva, K. S. Petrovsky, Yu. I. Pivovarov), food poisoning is divided into three groups according to etiological signs:
microbial poisoning;
non-microbial poisoning;
poisoning of unknown etiology.
1. Clinic. Clinical manifestations of food poisoning are very similar to each other. The clinic of salmonellosis, which in one form or another is observed in PTI of a different etiology, has been studied and described in the most detail, therefore it is advisable to use the classification proposed for salmonellosis. In general, this group of diseases is characterized by a short incubation period, acute onset and rapid development of the disease, a combination of signs of damage to the gastrointestinal tract and severe intoxication. There are some features of the clinical picture, depending on the type of pathogen. So, with staphylococcal etiology, the disease develops most acutely after a very short incubation period (30-60 minutes) with the onset of nausea, vomiting, which in some patients becomes indomitable for several hours. There is a strong cutting pain in the abdomen, resembling stomach colic; it is localized most often in the epigastrium, less often in the navel. With the gastric form of staphylococcal PTI, the nature of the stool does not change. Significantly more common, and most importantly, more rapidly developing symptoms such as weakness, dizziness, collapse, cyanosis, convulsions, loss of consciousness.
A rapidly developed food poisoning infection, which began with the appearance of intense stabbing pains in the abdomen, accompanied by nausea, vomiting and loose bloody stools at normal body temperature, makes one think about the clostridial nature of the disease (Cl. perfringens type C or F). For PTI proteus etiology of the disease is characterized by a sharp fetid odor, feces.
Pathogenesis. PTI pathogens are capable of producing toxins both in food products and in the human body. With the destruction of pathogens in the gastrointestinal tract, additional portions of various kinds of toxic substances are formed. The body responds to a massive ingestion of pathogens and toxic products into the human gastrointestinal tract with the stereotyped reaction described below.
The action of the complex of toxins causes local changes in the gastrointestinal tract (inflammatory process, changes in the synthesis of various biological substances, perversion of the motility of the gastrointestinal tract), general toxic syndrome (headache, hyperthermia of the body, disruption of the cardiovascular and nervous systems, etc.) . In addition, there is a perversion of the synthesis of biologically active substances [cyclic adenosine-3,5-monophosphate (cAMP) and cyclic guanosine monophosphate (cGMP), prostaglandins, histamine, intestinal hormones, etc.], which in turn contribute to the development of a complex complex of functionally -morphological disorders characterized by toxic damage to the gastrointestinal tract, cardiovascular and, in some cases, the nervous system.
Immunity with PTI (except for salmonella and dysentery etiology) is practically not studied.
Etiology. As already stated, food poisoning- polyetiological disease. Most often they are caused by salmonella, which for various reasons cannot be isolated bacteriologically, and opportunistic pathogens [Pokrovsky VI et al., 1981; Litinsky Yu. I. et al., 1982, etc.]. Opportunistic bacteria are quite widespread in the environment, and most of them live in the intestines. healthy people as saprophytes. For the development of the disease, a number of contributing factors are required both from the side of the microorganism (sufficient dose, appropriate virulence and toxigenicity, etc.) and the macroorganism (reduced body resistance, the presence of concomitant diseases, etc.). Under the influence of various external factors, opportunistic bacteria quickly change such biological properties as virulence, pathogenicity, sensitivity to antibacterial drugs and others, which must be taken into account when interpreting the issues of the etiopathogenesis of these diseases.
FOOD BACTERIAL TOXICOSIS OF STAPHYLOCOCCAL AND STREPTOCOCCAL
ETIOLOGIES
General characteristics and pathogenicity of these microorganisms. Staphylococci and streptococci are two separate genera of microorganisms widely distributed in nature. They are found in the air and in water, on the skin and in the respiratory tract, as well as in the intestines of humans and animals. From the ability to form pigment on nutrient media, golden, white and lemon yellow staphylococci (S. aureus, S. album, S. citreus) are distinguished. Of the various serological groups of streptococci (A, B, D, H), S. haemoliticus, S. viridans, S. faecalis are important in the pathology of animals and humans.
Staphylococci and streptococci - aerobes or facultative anaerobes, have a spherical shape and are arranged in the form of single cocci, clusters of diplococci or in other combinations, do not have capsules and flagella, do not form spores, grow well on ordinary nutrient media, are gram-positive. All of them are relatively resistant to drying, salt, do not die at low temperatures. Unfavorable conditions for the growth and reproduction of these microorganisms are an acidic environment (pH 6.0 and below), high temperature (75 ° C and above) is detrimental.
Staphylococcus aureus and other types, as well as some streptococci, have pathogenic properties and produce toxins. Such streptococci can cause diseases of the upper respiratory tract, pustular lesions of the mucous membranes and skin, and staphylococci are an etiological factor in the development of various septicopyemic processes in humans and animals, including generalized diseases - septicopyemia and septicemia.
The toxic substances produced by pathogenic staphylococci and streptococci are referred to as exotoxins. These exotoxins have an enteric effect, and therefore, food toxicosis in humans can be caused by a toxin without the presence of the microorganisms themselves. The accumulation of enterotoxins in products is facilitated by their massive contamination and storage time, environmental temperature, pH value, as well as the association of the development of staphylococci and streptococci with certain types of aerobic bacteria (Proteus, etc.) and mold fungi. The optimal conditions for the accumulation of enterotoxins in products are the presence of carbohydrates and proteins in their composition, temperature
25-35°C and pH 6.9-7.2. At temperatures below 20 °C and pH 6.5, the production of enterotoxins slows down, and at temperatures below 15 °C and pH 6.0 it stops. A factor contributing to the accumulation of enterotoxins in milk is its storage at a temperature above 10 °C. Staphylococcal and streptococcal enterotoxins are thermostable and are destroyed only during prolonged boiling of products. To typify pathogenic and enterotoxigenic cocci from saprophytic cocci, various methods. So, to indicate pathogenic and enterotoxigenic staphylococci, a hemolysis reaction, a plasma coagulation reaction, a phage typing method and a biological test on laboratory animals are used. All these methods are studied in detail in laboratory and practical classes on veterinary sanitary examination, as well as microbiologists.
Epidemiology of staphylococcal and streptococcal toxicoses. Over the past 2-3 decades, in many countries of the world, there has been an increase in the proportion of staphylococcal toxicosis from the total number of foodborne diseases of a bacterial nature in humans. Most often, cases of staphylococcal toxicosis are observed from eating confectionery cream products, cakes, pastries, milk and dairy products (cottage cheese, sour cream, cheese). Dairy products are also a source of food streptococcal intoxication. In the occurrence of staphylococcal and streptococcal toxicoses, the role of meat, fish, salted and smoked meat and fish products is not excluded.
Sources of infection of food products with staphylococci and streptococci are very diverse. One of the main places is occupied by animals
(cows, sheep) suffering from mastitis and giving milk known to be infected with these microorganisms. Often, enterotoxigenic strains of staphylococci, as well as streptococci, are isolated from the carcasses and organs of animals that were forcedly killed during septicopyemic processes, enteritis, and pneumonia. Currently great importance.gives exogenous and aerogenic contamination of food products by these microorganisms. Exogenous contamination is possible during the primary processing of food products by persons suffering from pustular diseases of the skin, and especially the hands. Aerogenic contamination of products is possible by persons with rhinitis and nosopharyngitis.
When coughing and sneezing, staphylococci massively infect the environment, including food.
A distinctive feature of the development of toxicosis of staphylococcal and streptococcal etiology in humans is an exceptionally short incubation period of 2-6 hours. Clinically, toxicosis occurs in the form of acute gastroenteritis with the following symptoms: soon after ingestion of infected food, abdominal pain, headache, weakness, nausea and vomiting, frequent loose stools appear. With staphylococcal toxicosis, it is also possible to raise the temperature to 38.5 ° C, a decline in cardiac activity, convulsions, cyanosis of the lips, nose and extremities, weakening of vision, and even loss of consciousness with a drop in blood pressure.
Recovery usually occurs in 1–3 days (no deaths have been reported in the literature).
Sanitary assessment of products in the isolation of toxigenic coccal microorganisms. When isolated from meat samples and lymph nodes carcasses of toxigenic coccal microbes, internal organs are subject to technical disposal, and the meat is disinfected by boiling or sent for the manufacture of sausage bread. Finished products from which toxigenic staphylococci and streptococci are isolated are disposed of.
Botulism.
It belongs to the most severe food poisoning. Botulism occurs when eating food containing botulinum bacillus toxins. Currently, the causes of botulism are well studied, and measures have been developed and are being implemented to combat this disease. As a result of widely held preventive measures the incidence of botulism has dropped sharply.
The causative agent of botulism is widespread in nature; it lives in the intestines of warm-blooded animals, fish, humans, rodents, birds, cats, in the soil, in the mud of reservoirs, etc. Cl. botulum is a spore-bearing bacillus that is a strict anaerobe. There are six types of botulinum bacillus (A, B, C, D, E, F). In the USSR, the most common options are A, B, E. The most toxic is type A. Toxins of each type are neutralized only by the corresponding antitoxic serum. Botulinum bacillus spores are extremely resistant to various environmental factors. Complete destruction of spores was noted at a temperature of 100°C for 5-6 hours, at a temperature of 105°C - for 2 hours, at a temperature of 120°C spores die in 10-20 minutes. Botulinum bacillus spores are highly resistant to low temperatures and various chemical agents. They remain viable for more than a year in refrigerators at a temperature of -16 ° C, tolerate drying well, remaining viable for about a year.
Spore germination is delayed by high concentrations of sodium chloride (8%) and sugar (55%). The causative agent of botulism is sensitive to an acidic environment; its development is delayed at pH 4.5 and below. This property of the stick is widely used in the production of canned food, since under conditions acid environment Botulinum bacterium does not produce a toxin.
Optimal conditions for the development and toxin formation of botulinum bacillus are created at a temperature of 25-30°C. However, the formation of toxin quite intensively occurs at a temperature of 37°C. At lower temperatures (15-20°C), microbial reproduction and toxin formation proceed more slowly and the complete reproduction of the microbe and toxin formation proceed more slowly and completely stop at a temperature of 4°C (the exception is botulinum type B, which releases the toxin). Toxin - the causative agent of botulism in terms of toxic effect on the body is the most powerful of all known bacterial toxins; a lethal dose for humans is hundredths of a milligram per 1 kg of body weight. In an acidic environment, the toxin is stable, and in a slightly alkaline (pH 8.0) it loses activity by 90%. Long-term storage of the toxin in a frozen state does not reduce its activity. At a temperature of -79°C, it remains active for 2 months. Table salt, even at high concentrations, does not inactivate the toxin. Toxin formation is delayed only when the content of NaCl in the food product is 11% (F. M. Belousskaya).
Therefore, if the toxin has already accumulated in the food product, then canning the product - salting, freezing, pickling - does not inactivate it.
The resistance of the toxin to high temperatures is relatively low: when boiled, it is destroyed within 15 minutes, when heated to 80 ° C - after 30 minutes and up to 58 ° C - within 3 hours. Therefore, high temperature is one of the most important ways to combat botulism. Usually the toxin is inactivated by boiling pieces of meat, fish and other products for 50-60 minutes.
The causative agent of botulism is capable, under favorable conditions, of reproduction and toxin formation in any products of both animal and vegetable origin. It was found that the most common cause of botulism are canned foods. Usually, with the development of microbes, the organoleptic properties of the product do not noticeably change, sometimes only a faint smell of rancid fat is felt, much less often the product softens and its color changes. In canned food, as a result of the development of microbes and hydrolysis of protein and other substances, gases can accumulate, causing persistent swelling of the bottom of the can (bombing).
In recent years, cases of botulism caused by the use of canned food home made. Mushrooms and vegetables with low acidity in rolled up jars are the most dangerous. There are cases of the disease as a result of the use of canned meat, ham, ham, as well as salted, dried home-made fish. This is due to the fact that the mode of processing canned food at home does not ensure the death of botulinum bacillus spores.
Botulism is an extremely serious disease, characterized by high mortality (60-70%). The incubation period is 12-24 hours, less often a few days, and in some cases it can be reduced to 2 hours.
The first signs of the disease are malaise, weakness, headache, dizziness and often vomiting. Then symptoms of visual impairment appear (weakening of vision, double vision, trembling of the eyeballs, drooping of the eyelids). The voice becomes weak, swallowing and chewing are difficult. The duration of the disease is different, on average - from 4 to 8 days, sometimes up to a month or more.
Anti-botulinum serum is a highly effective therapeutic agent, the timely administration of which prevents death.
Mycotoxicoses
Food mycotoxicoses are diseases arising from the use of grain processing products contaminated with toxic substances of microscopic fungi. Mycotoxicoses include ergotism, fusariotoxicosis and aflotoxicosis. Currently, mycotoxicoses are recorded extremely rarely.
Ergotism occurs when using products made from grain containing an admixture of ergot. For the prevention of ergotism importance has a thorough cleaning of seed and food grains from ergot. The content of ergot in flour and cereals is allowed no more than 0.05%.
Fusariotoxicoses include alimentary-toxic aleukia and poisoning with "drunken bread".
Alimentary-toxic aleukia, or septic tonsillitis, develops as a result of the consumption of products from grain overwintered in the field, contaminated with toxins of fungi from the genus Fusarium. The toxic substance of these fungi is heat-resistant and does not lose activity during heat treatment of grain products.
Poisoning with "drunken bread" also occurs when eating grain products affected by the toxic fungus Fusarium graminearum. The signs of this disease resemble a state of intoxication and are characterized by a state of excitement, euphoria (laughter, singing, etc.), impaired coordination of movements ( wobbly gait). Often there are disorders of the gastrointestinal tract - diarrhea, nausea, vomiting.
The main measure for the prevention of fusariotoxicoses is the prohibition of the use of food products from grain that has overwintered in the field.
Measures to prevent this food poisoning also include compliance with the necessary humidity and temperature conditions for storing grain, excluding its moisture and mold.
Aflotoxicosis is a disease that occurs with prolonged use of products from cereals affected by fungi of the genus Penicillium and Aspergillus.
The main measure for the prevention of mycotoxicoses is the creation of the correct conditions for storing products (especially grains), excluding their moisture and mold.
NON-MICROBIAL FOOD POISONINGS
Characteristic features of non-bacterial foodborne diseases are their predominant occurrence in everyday life and a small number of victims. Among foodborne diseases, non-bacterial poisonings account for 7-15%. These diseases are characterized by high mortality, mainly when using poisonous mushrooms idiopathic plants.
This group includes poisoning by inedible poisonous products (mushrooms and wild plants), food products that have temporarily become poisonous or partially acquired toxic properties (potato solanine, beans, bitter kernels of stone fruits, animal organs), poisoning caused by toxic impurities in food products (salts heavy metals, weeds and pesticides).
Poisoning by inedible products of plant and animal origin
Mushroom poisoning. Among the poisonings of plant origin, the most common are diseases caused by fungi. On average, about 15% of cases of mushroom poisoning are fatal.
Distinguish between edible and non-edible mushrooms. Edible mushrooms are unconditionally edible and conditionally edible. Unconditionally edible mushrooms are usually eaten without preliminary and additional processing ( porcini, boletus, boletus, butterdish, flywheel and some agaric champignons, real honey agaric, chanterelle, etc.).
Conditionally edible mushrooms - lines, morels, russula, pigs, etc. - if cooked incorrectly, can cause food poisoning. Before culinary processing, these mushrooms are subjected to long-term cooking by removing the broth (lines, morels, russula, pigs, etc.) or soaking in running or changing water (milky mushrooms - mushrooms, podgruzdi, volushki, nigella, etc.).
Pale grebe, pestilence fly, false honey agaric, etc. are poisonous mushrooms. Poisoning with pale grebe and conditionally edible mushrooms is the most dangerous. Poisoning from the use of poisonous mushrooms often occurs at the end of summer, during the period of their greatest collection, and is usually of an individual or family nature.
Poisoning by certain edible foodstuffs that have partially acquired toxic properties.
This group includes food poisoning caused by potato solanine, kidney beans, bitter stone fruit kernels, beech nuts, and the organs of some fish and animals.
Solanine is part of the potato in an amount of about 11 mg, most of all in the peel - 30-64 mg%. The content of solanine may increase during germination and greening (420-730 mg%) of potatoes. Solanin is similar in properties to glycosides and belongs to hemolytic poisons, that is, it destroys red blood cells. For humans, the toxic dose of solanine that can cause poisoning is 200-400 mg%. Potatoes containing an increased amount of solanine have a bitter taste, and when consumed, a scratching sensation occurs in the throat. Poisoning is accompanied by a slight upset of the gastrointestinal tract. To prevent the accumulation of solanine, potatoes are stored in dark rooms at a temperature of 1-2°C. Green potatoes are not eaten.
Fasin is a toxic substance found in raw beans. Food poisoning occurs when bean flour and food concentrates are used in food. Poisoning is manifested by mild symptoms of intestinal upset. The main measure for the prevention of phasin poisoning is the observance of the technology for the preparation of bean concentrate, which reliably ensures the inactivation of phasin.
Amygdalin. Some plants, their fruits and seeds contain substances that have poisonous properties. Thus, bitter almonds and kernels of stone fruits contain the glycoside amygdalin, the destruction of which releases hydrocyanic acid. Amygdalin is found in bitter almonds in an amount of 2-8%, in the kernels of apricot kernels - 8, peaches - 2-3, plums - 0.96%; when it is split, 5.6% of hydrocyanic acid is formed.
Poisoning in mild form is accompanied by headache, nausea; in severe form of poisoning, cyanosis, convulsions, loss of consciousness, and death are possible.
Fagin. Possible poisoning caused by raw beech nuts, which contain fagin. Poisoning manifests itself in the form of poor health, headache, nausea and intestinal upset. Nuts are neutralized by heat treatment at a temperature of 120-130 ° C for 30 minutes.
Weed poisoning. Flour from poorly cleaned grain may contain poisonous impurities of cockle, sophora (gorchak), heliotrope pubescent, trichodesma gray, etc.
Cases of poisoning with these toxic impurities are very rare. The content of some impurities in flour is standardized: cockle - no more than 0.1%, sophora - 0.04%.
Measures for the prevention of poisoning by weed impurities are reduced to an increase in the agrotechnical culture of agriculture and a thorough cleaning of grain from impurities.
Poisoning by impurity salts of heavy metals
Toxic amounts of salts of heavy metals accumulate in cases where the material of utensils, apparatus, equipment contains elevated "concentrations of these substances, that is, when it does not meet hygienic requirements, or when the utensils are not used for their intended purpose. Toxic metals can also enter food products from the soil into as a result of intensive pollution with industrial emissions, often containing a significant amount of lead, arsenic, copper, zinc, antimony, tin, fluorine, etc. These substances enter the environment with fuel combustion products, chemical fertilizers and pesticides used in agriculture. The degree of toxic effect of metal salts depends on their quantity and mechanism of action on the body.Poisoning often proceeds according to the type of acute forms, accompanied by pronounced local or general symptoms of a health disorder.Some metal salts have a cumulative ability, i.e., the ability to gradually accumulate in the body and cause a chronic form of poisoning.
Lead poisoning.
Lead poisoning occurs when lead is ingested from glazed earthenware, from tin-plated dishes or from equipment coated with tin with a high lead content, as well as from enameled dishes in violation of the enamel production recipe.
Preserving food with high acidity in such dishes (pickled vegetables, cabbage soup, borscht, compotes, marinades, dairy products etc.) the transition of lead into the product is possible. It has been established that prolonged daily administration of 1 mg of lead into the body leads to the development of chronic poisoning. At the same time, general malaise, loss of strength, nausea, and then a “lead border” along the edge of the gums, constipation, abdominal cramps, anemia, and pallor appear at first. Acute forms of food poisoning are extremely rare and can develop only with the simultaneous introduction of lead into the body up to 10 mg per day.
To prevent lead poisoning, its content in dishes is strictly limited by sanitary standards. So, in tin for tinning plate utensils and digestive boilers it can be contained - no more than 1%, in aluminum foil - no more than 0.1% together with zinc. The daily maximum allowable intake of lead with food should not exceed 0.2-0.25 mg.
Copper poisoning.
At present, poisoning with copper salts is extremely rare, since copper utensils and equipment have been replaced by more advanced ones made of stainless and corrosion-resistant materials. Untinned utensils, which were previously widely used, were a source of increased amounts of copper in food and food in the food industry and in catering establishments. When eating food containing copper salts, usually after 2-3 hours, colicky abdominal pain, diarrhea, and vomiting appear. The disease ends within the first day. According to sanitary standards, the amount of copper compounds in food products is strictly limited: in tomato paste- copper compounds in foodstuffs are strictly limited: in tomato paste - no more than 80 mg/kg; in tomato puree-15-20; in canned vegetables, jam, marmalade-10; in canned fish(in tomato sauce) - 8; in canned milk and fruit compotes - 5 mg/kg.
Zinc poisoning.
Zinc poisoning can occur during the manufacture and storage of acidic foods (jelly, compotes, cabbage soup, etc.) in zinc dishes. When moistened, zinc surfaces form a film of zinc carbonate in air, which, interacting with organic acids of the food product, forms its salts of organic acids. In case of zinc poisoning, headache, frequent vomiting, and abdominal pain are observed. Zinc does not dissolve in water, therefore, at catering establishments, it is allowed to store drinking water or bulk products in galvanized iron dishes.
Polymeric materials (plastics).
At present, polymeric materials are widely used in the food industry, public catering and trade (tare, packaging, pipelines, equipment, etc.).
The danger is represented by additives that are included in the polymer base (stabilizers and antioxidants, plasticizers, dyes) and non-polymerized monomers. For hygiene requirements, the residual amount of monomers should not exceed 0.03 - 0.07%.
Poisoning with pesticides
The use of pesticides (pesticides) in agriculture to protect cultivated plants from weeds and pests is expanding every year. The use of pesticides in agriculture gives a great economic effect. In all countries of the world, the industrial production of pesticides is growing and by now it has already reached several million tons per year. According to the nature of their chemical structure, pesticides are divided into organochlorine preparations - chlorinated hydrocarbons (DDT, hexachloran, DDT-2, 4-D, 1hetachlor, etc.), organophosphorus preparations (metafos, chlorophos, karbofos, thiophos, etc.), organomercury compounds (granosan , mercuran, etc.), carbamates - compounds of carbamic acid (sevin, tsiny, tsiram, etc.) and other organic and inorganic compounds.
According to their purpose, pesticides are divided into the following main groups: insecticides that are used in the fight against harmful insects; fungicides that act on pathogens of fungal diseases; herbicides used in weed control.
The toxicity of pesticides to humans is not the same and depends on many reasons. Of particular danger are pesticides, which are characterized by high stability in the external environment, pronounced cumulative properties and the ability to be excreted in the milk of lactating animals and in the milk of nursing mothers. This group of pesticides includes organochlorine pesticides (hexachloran, polychloropinene, ligdan, etc.). For example, hexachlorane can persist in soil for 11 years. The most acceptable pesticides are those that are relatively quickly decomposed into harmless components by the influence of environmental factors. At present, organophosphorus substances, which are less resistant to environmental factors, are widely used in agriculture. Most of them decompose in plants, soil, water within a month. Pesticides of this group are much less frequently found in food products, as they are destroyed during culinary processing.
Ways of contamination of food products with pesticides are varied. Pesticides can enter plant products directly during the processing of crops, food stocks, and also as a result of soil pollution; water, air.
The adverse effect of pesticides on the human body can manifest itself in the form of acute and chronic poisoning. Acute poisoning often occurs with gross violations of the rules for the use of pesticides and the rules for the use of food products treated with pesticides (the use of seed grains pickled with granosan). Chronic poisoning occur as a result of long-term use of food products containing pesticides in doses that slightly exceed the maximum permissible concentrations. The manifestation of chronic poisoning is most often accompanied by diseases of the digestive system (liver, stomach), cardiovascular system. The mechanism of toxic action of most organophosphorus compounds is based on the inhibition of cholinesterase, accompanied by the accumulation of acetylcholine in the blood and tissues.
Classification of food poisoning

Etiology of food poisoning, microbial etiology
1.1. Toxic infections- Potentially pathogenic microorganisms: Proteus mirabilis, Proteus vulgaris; enteropathogenic, enteroinvasive: E. coli, Clostridium perfringens, Streptococcus fecalis; other little-studied bacteria: citrobacter, hafnia, Klebsiella, etc.
Toxicosis
1.2.1.Bacterial- bacterial toxins produced Staphylococcus aureus and Clostridium botulinum
1.2.2. Mycotoxicoses – mycotoxins produced by microscopic fungi of the genera Aspergillus, Fusarium, ergot, etc.
1.3. Mixed etiology (mixed) – combinations: potentially pathogenic microorganisms or potentially pathogenic microorganisms + toxin.
Food poisoning investigation- a set of measures aimed at identifying the etiology of the disease and the factors contributing to its occurrence, in order to treat and prevent such diseases.
The sanitary doctor for food hygiene, as well as medical doctors (district doctor and polyclinic specialists, shop doctors of medical and sanitary units and doctors of other medical institutions) take part in the investigation of the poisoning.
Before the health officer arrives, the investigation of food poisoning is conducted local doctor or paramedical staff . They are obliged:
1. Remove the remains of suspicious food from consumption and take samples for analysis in the amount of 200-300 g.
2. Collect vomit and feces of the sick, gastric lavage and urine in the amount of 100-200 ml for bacteriological analysis, take 10 ml of blood from the cubital vein for blood culture.
All samples for analysis should be collected in a sterile container. In this regard, in medical institutions, primarily at ambulance stations, as well as in hospitals, clinics, there should be necessary stock sterile glassware. If sterile glassware is not available, cleanly washed glassware should be boiled in water before use.
3. Send the seized food, collected secretions and washings for examination to the sanitary-bacteriological laboratory or keep them in the cold until the arrival of the sanitary doctor.
4. Before clarification of all circumstances, prohibit the sale of suspicious products.
5. Immediately report food poisoning by telephone, telegraph and send an emergency notice by courier to the local center of hygiene and epidemiology.
Sanitary doctor when investigating food poisoning, should:
1. Conduct a survey of patients according to the following scheme:
FULL NAME. ________________________________________________________________________
Age ________________________________________________________________________
Place of work_________ _________________________________________________________
What and where did the victim eat during the last 2-3 days.____________________________
Are there diseases among family members, where and what do they eat __________________
Date and time of onset of illness
Clinical symptoms diseases: fever, diarrhea, chills, convulsions, cyanosis, headache, pain in the extremities, abdominal pain, nausea, vomiting _______________________
Which food or dish is suspected ______________________________________________
Place and time of ingestion of a suspicious product _________________________________
Incubation period __________________________________________________________________________
2. Thoroughly analyze with the participation of attending physicians the entire clinical picture of the disease, taking into account the primary symptoms, further course and outcomes. In this case, it is necessary to exclude diseases of a different etiology, resembling food poisoning in some respects.
3. Send, if this is not done, suspicious products and secretions collected from the sick to the laboratory for analysis.
4. Ensure that the blood of the diseased is taken and sent to the laboratory for culture and serological tests. Serological reactions are put on the 1-3rd day of the disease and on the 7-10th day. If the reactions are not made in a timely manner, then they are placed on the 7-10th day and repeated on the 15-20th day.
With a large number of victims, the blood of the most seriously ill patients is subjected to serological testing (it is recommended to take blood from at least 15-20 people), and with a small number of victims, preferably from all patients.
In the case of deaths, the results of a pathoanatomical autopsy are taken into account and a laboratory study of cadaveric material is performed: parenchymal organs, contents of the stomach and intestines (200-300 g), blood from the heart (10 ml).
5. To find out the ways of infection or contamination of a food product with poisonous substances that caused poisoning, it is necessary to check the sanitary conditions of transportation, food preparation technology, the shelf life and sale of raw materials, semi-finished products and finished products, the availability of veterinary and sanitary certificates, the possibility of infection of products with bacteria carriers, persons with pustular diseases, etc.
In the course of the investigation, the sanitary doctor takes the necessary measures:
1. Prohibits the use or in necessary cases establishes the procedure for the sale of food products that caused poisoning.
2. Immediately removes from work or transfers to work not related to the processing, storage or transportation of food, persons who could be a source of food contamination.
3. Suggests and controls the implementation of the necessary sanitary measures at the enterprise, sanitary violations in which caused the production of substandard products (temporary or permanent prohibition of operation, disinfection, repair of the food enterprise).
4. Attracts to administrative responsibility or transfers the materials of the investigation to the prosecutor's office to bring to justice those responsible for the production, production and sale of the product that caused food poisoning.
Food poisoning of non-microbial etiology, their prevention, methods of investigation. Examination of food products for the content of food additives.
I. food poisoning, II. Food poisoning caused by bacteria caused by bacteria,
exotoxins (intoxication): flowing by type
acute gastroenteritis
(toxic infections)
1) Clostridia botulism (neurotoxin); 1) salmonella;
2) clostridia perfringens 2) Escherichia coli;
(α – toxin and β – toxin); 3) proteus;
3) staphylococci (enterotoxins). 4) Klebsiella;
4) Clostridia difficile. 5) genus of citrobacterium;
6) the genus Bacillus cereus;
III. Food poisoning, 7) enterococci (Str. faecalis);
caused by toxins 8) Pseudomonas aeruginosa;
fungi (mycotoxicosis). 9) parahemolytic vibrio; 10) cerations.
Mark the biological features of the pathogen that determine their leading role in the etiology of food poisoning (for example: staphylococci produce enterotoxins, which, being absorbed in the stomach, cause activation of its and intestinal motility, lower blood pressure due to the effect on the parasympathetic nervous system: characterize botulinum toxin in Cl. botulinum and its effect on the central nervous system, Cl.difficile - enterotoxin acts on the adenylate cyclase system, accumulates cyclic AMP, disturbs the water and electrolyte balance (diarrhea, dehydration).
Epidemiology.
Source:- a person, animals (sick or carriers of the pathogen). The reproduction of microorganisms becomes possible if sanitary rules are violated during the preparation of food products, as well as in the process of preparing finished products from them, if they are improperly transported and stored.
Distribution path:- alimentary.
Poisonings are recorded throughout the year, but the vast majority of them occur during the warm season, which is explained by the possibility of bacterial growth in perishable products if there are no sources of artificial cold for their storage and transportation.
Emphasize that among the total number of food poisonings of various etiologies, bacterial ones occupy a leading place (60-95% of cases).
General clinical symptoms of poisoning.
Acute onset after a short incubation period (from 2-4 to 8 hours) in the form of general toxic effects: fever, weakness, headache, dysfunction of the cardiovascular and nervous systems. The presence of symptoms of gastroenteritis is also characteristic: nausea, vomiting, diarrhea, bloating and rumbling in the abdomen. Duration does not exceed 1-3 days. Food poisoning caused by serovars A and C Cl. perfringes are becoming increasingly important and represent an urgent problem for public health in most countries of the world.
Cl. perfringens type A causes mild and medium degree severity: the disease develops acutely, with abdominal pain, vomiting with blood, diarrhea (up to 20 times a day). Symptoms disappear in the next 12-24 hours.
Cl. perfringens type C causes necrotizing enteritis. At acute forms the disease can end in death within 12-24 hours (the action of β-toxin).
In recent years, the growth of diseases caused by Bacillus cereus (soil bacteremia - saprophyte) has been different. Contaminates food products, causing food poisoning. Bacteria secrete enterotoxin during the germination of spores that are resistant to certain thermal conditions of food processing (usually vegetables). B. cereus resembles anthrax bacillus, in smears it is located in the form of a picket fence, gram-positive, on agar it forms “flattened” colonies with uneven edges, on blood agar they give a hemolysis zone, over time the colonies become waxy (from Latin cera, wax, candle) ; in liquid media film + flocculent sediment + turbidity of the broth. Bacteria have high proteolytic activity, liquefy gelatin, form lecithinase, acetoin, break down glucose and maltose to acid.
See #29
31. O-antigen - lipopolysaccharide-protein complex, thermostable (withstands boiling for 2.5 hours, autoclaving at 1200 C - 30 minutes), sensitive to formaldehyde, but resistant to alcohol. This is a group antigen - according to the classification of Kaufman and White, the family is divided into 67 serogroups. They are designated capital letters Latin alphabet (A, B, C, D, etc.). Some groups share O antigens, but each group contains one main antigen. (For example, in group A - this is 2, in group B - 4, in group C - 6, D - 9, etc.)
32. Features of microbiological diagnostics.
The earliest possible diagnosis (5th -7th days of the disease) is necessary for the timely implementation of anti-epidemic measures. For the purpose of diagnosis, bacteriological and serological research methods are used. The choice of material for research is determined by the stage of the disease. In the incubation period, feces are examined; in the prodromal period - blood for culture; at the height of the disease (2-3 weeks) - urine, feces, bile, scraping from roseola, bone marrow, etc. The selected pure culture of the pathogen is identified by studying the biochemical activity; seroidentification is performed first using polyvalent group serum, then - group and typical diagnostic sera. For the purpose of serodiagnosis, the following reactions are performed: Vidal, RPHA with O-, H-, Vi- erythrocyte diagnosticums. A skin-allergic test with Ebertine, which reveals a state of delayed hypersensitivity, is of diagnostic value.
33. Dysentery is an acute anthroponotic infection with a fecal-oral transmission mechanism, characterized by a predominant lesion of the large intestine mucosa, loose stools mixed with mucus and blood
Taxonomy.
Family Enterobacteriaceae
Tribe Escherichia
Species Sh. Dysenteriae
Morphology.
Gram-negative rod, 0.5 x 3.0 µm; immobile, has a general type of pili and sexual. Does not form a dispute. They can form a microcapsule. The smears are arranged randomly.
cultural properties.
Facultative anaerobes, chemoorganoheterotrophs, grow well on simple nutrient media. The optimum growth temperature is 37 0 C, pH 6.7-7.4. On the broth grow in the form of diffuse turbidity. On agar, 2 types of colonies can form: S (small, colorless, smooth) and R (larger, dry, rough). On differential diagnostic media (Endo, Levin, Ploskirev), Shigella grow in the form of colorless colonies, since they do not break down lactose).
biochemical properties.
Saccharolytic activity: lactose and sucrose are not broken down (except for Sh. Sonnei, which slowly ferment lactose), other sugars decompose to acid without gas, slowly break down glucose into acid, fermenting mixed type(exception - Newcastle strains). In relation to mannitol, they are divided into mannitol-positive (group A) and mannitone-negative (all others).
Proteolytic Properties : shigella do not form hydrogen sulfide, indole form intermittently, do not liquefy gelatin, do not ferment urea, reduce nitrates to nitrites.
antigenic properties.
Shigella have 2 main antigens: O- and K-.
Somatic O-antigen - group, cell wall lipopolysaccharide, thermostable.
Surface K-antigen, typical, thermolabile.
According to the antigenic structure, Shigella are divided into groups, those - into serovars, and serovars - into subserovars. Serovars are indicated by Arabic numerals, and subserovars by Arabic numerals with the addition of lowercase Latin letters.
In accordance with the structure of the O-antigen and with some biochemical features of the known 39 Shigella serotypes, according to the International Classification, they are divided into 4 groups (A, B, C, D). Further differentiation into types and subtypes is based on the features of the antigenic structure.
Enzymes of pathogenicity.
1. Toxins:
Endotoxin is a lipopolysaccharidoprotein complex that acts on the nervous and vascular system the human body;
Exotoxin (Shiga toxin) is cytotoxic (impairs protein synthesis on ribosomes); enterotoxic; neurotoxic action.
2. Enzymes of aggression: hyaluronidase; fibrinolysin; mucinase; plasmacoagulase; neuraminidase.
3. Structural and biochemical components of cells: microcapsule; drank; outer membrane proteins capable of binding to epithelial cell receptors and inducing them to "induced endocytosis".
The genes encoding virulence are located in chromosomes and in plasmids: genes encoding the ability to attach to epithelial cells; genes that damage cell membranes. In the case when the genes that determine the ability to penetrate into cells are on plasmids, they can be easily transmitted by EPC.
resistance.
In soil, water, food, shigella survive up to 2-3 months, actively multiply in milk at room temperature. The terms of survival of microorganisms in milk and dairy products are longer than the terms of their implementation (hence the outbreaks associated with infection with dysentery through milk, sour cream). On fabric, paper shigella persist up to 1 month. They live on vegetables and fruits for more than 2 weeks. When heated to 60 0 C, death occurs in 15-20 minutes, when boiled - immediately. very sensitive to disinfectants. Important feature Shigella Zone - their resistance to environmental factors and pronounced resistance to antibiotics.
Epidemiology.
Reservoir and source of infection- a person (sick or bacterial carrier). The greatest danger for the spread of infection is posed by patients with erased forms of dysentery, especially persons of certain professions (for example, those working in the food industry).
Transfer mechanism- fecal-oral. Transmission routes- water, food, contact household. The factor of dirty hands and the "fly" factor are of great importance.
34. Pathogenesis and clinical features.
The natural susceptibility of people to the disease is high. Shigella, having overcome the non-specific oral defense factors and the gastric acid barrier, attach to colonic enterocytes and secrete toxins. Specific proteins of the outer membrane of Shigella interact with plasma membrane receptors and provide adhesion. With the help of the enzyme mucinase, they penetrate into the cells of the mucosal epithelium. In the affected cells, pathogens actively multiply; the toxin they secrete ensures the development of an inflammatory process in the submucosal layer. Inflammation is maintained by the cytotoxin secreted by Shigella. Edema and destruction of the colon mucosa develops. Catarrhal or fibro-necrotic inflammation leads to the death of epithelial cells and contributes to the formation of erosion and ulcers. At the same time, when pathogens die, endotoxin is released, causing intoxication of the body.
Dysentery constantly proceeds with symptoms of dysbiosis, preceding or accompanying the development of the disease. All this determines the development of exudative diarrhea and hypermotor dyskinesia of the colon.
Thus, the pathogenesis of the disease is determined by the adhesive properties of the pathogen, its penetration into cells, reproduction there and the production of toxins. Intoxication is exacerbated by the action of endotoxin, which is released during the mass death of pathogens. Clinical manifestations depend on the type of pathogens. The incubation period lasts from 1 to 7 days. The onset of the disease may be accompanied by fever up to 38-39 0 C, headache, weakness. There are cutting pains in the abdomen. At the same time, liquid stools are noted; later the stool becomes scanty, with large quantity mucus and mixed with blood ("rectal spit"). Characterized by the appearance of tenez - painful pulling pains in the region of the rectum. After the transfer of dysentery, a chronic process or the formation of a bacteriocarrier is possible.
35. For the study, the patient's stools are taken on the Endo-Levin-Ploskirev medium or a smear from the rectum on the green broth. . The reaction is taken into account after 24 hours; with a positive result, hyperemia and an infiltrate of at least 1 * 1 cm in size appear. The reaction is detected in the first days of the disease, its frequency increases from the 4th to the 5th day of the disease; it has significant sensitivity (80 - 85% of positive results), but is not strictly specific. Most children under the age of 1 year have a negative reaction.
36. E. coli is a sanitary indicative microorganism, its detection indicates fresh fecal contamination of environmental objects.
37. Escherichiosis is an acute intestinal disease caused by pathogenic E. coli and proceeding as enteritis and enterocolitis.
The causative agents are diarrheagenic serovars of Escherichia coli; they are divided into 5 groups. Morphologically representatives different groups are indistinguishable from each other; they are differentiated according to antigenic structure and pathogenicity factors. Currently, ~170 antigenic variants of E. coli are known, more than 80 of them cause coli infection.
The diarrheagenic serovars of Escherichia coli are divided into the following 5 groups (Table 1):
Enteropathogenic (EPKD) include 15 serogroups and 29 serovars.
Enteroinvasive (EICP) - about 9 serogroups and 13 serovars.
Enterotoxigenic (ETEC) - 17 serogroups and 16 serovars.
Enterohemorrhagic (EHEC) - 4 serogroups.
Enteroadhesive (EACP) not definitively differentiated
38. ETEC - ETEC cause cholera-like disease. With the help of pili, they attach to the epithelium of the lower parts of the small intestine and produce 2 types of toxins: heat-labile and heat-stable. The latter is a low molecular weight protein; it increases the content of cyclic guanine monophosphate in epithelial cells, which leads to a disruption in the transport of molecular iron and an increased release of water from cells. The high molecular weight temolabile toxin resembles vibrio cholerae exotoxin in its mechanism of action. The course of the disease resembles light form cholera. In the literature, it is often called travelers' diarrhea or tourists' diarrhea. Route of infection: water. Number of bowel movements 5-10.
39. EIEC cause a dysentery-like illness in children and adults. Adsorbed on the cells of the epithelium of the lower parts of the colon. Penetrate inside the cells; multiplying and destroying them. Spreading through the intercellular spaces, they affect neighboring cells, forming ulcers. They produce Shigella-like toxin. Clinical symptoms: first - watery diarrhea, then an admixture of mucus and blood appears in the stool. Mechanism of infection: food, water.
40 .EPEC- cause escherichiosis in children under 1 year old (from mother to child, through milk formula). Pathogens affect the epithelium of the small intestine, are adsorbed on the surface of enterocytes due to proteins of the outer membrane and multiply here, damaging the microvilli and causing their rejection. The inflammatory reaction that develops in this case is due to the action of endotoskin, which is released during the destruction of Escherichia coli. The course of the disease is severe, it can last for weeks. The main clinical manifestations: diarrhea, vomiting, regurgitation of food, signs of dehydration and demineralization of the body. Hypotrophy may develop. Pathogenicity factors: adhesion, colonization, invasion, endotoxin, thermolabile enterotoskin.
41. EHEC - causative agents of hemorrhagic diarrhea and hemolytic syndrome. Pathogens secrete a Shigel-like cytotoxin, which causes destruction of the vascular endothelium, intestinal cells, kidney cells, and, accordingly, differentiation of blood in stools. The appearance of urohemorrhagic syndrome (blood in the urine), but the microorganism penetrates into the blood, is destroyed with the release of endotoxin, which acts on the mast cell, causing its degranulation, which leads to the release of serotonin and histamine, patients develop severe headache, bleeding, development of toxic shock and peritonitis (if the patient lived to see it).
42 . Features of laboratory diagnostics.
Diagnosis of escherichiosis caused by diarrheagenic E. coli is based on the isolation of a pure culture of the pathogen and its identification using sets of polyvalent OK-sera containing antibodies to certain O-antigens. In Russia, sets of diagnostic OK-sera are produced: OKA, OKV, OKS, OKE. The main polyvalent serum OKA contains antibodies to O- and K-antigens of more than 20 main serological groups, the remaining OK-sera contain antibodies to O- and K-antigens of the same serogroups, but in a smaller combination. The agglutination reaction with the isolated culture is placed on the glass. In this case, all sets of OK-sera are used sequentially. First, the OK-serogroup is determined with a live culture (at the same time, its biochemical properties are also studied), and finally, the O-serogroup is identified using adsorbed O-sera and heated at 100 0 C for an hour (to destroy the K-antigen) culture. You can use the reaction of coagglutination, IFM.
To identify EICG, a keratoconjunctival test, a test with dysenteric phage, ELISA (to detect outer membrane proteins encoded by the plasmid) can be used. RIF can be used to detect specific antigens in the feces of patients. The fastest and most specific method for diagnosing diseases caused by diarrheagenic E. coli is the use of DNA probes. They make it possible to directly detect the genes of plasmids responsible for the pathogenicity of E. coli or the synthesis of their cytotoxins.
43. Cholera.
Taxonomy:
Family Vibrionaceae
Species V. cholerae
Biovars; V. cholerae asiaticae (classicae)
Morphology:
slightly curved stick, dimensions 1.5-4.0 x 0.2-0.4 microns, polymorphic (from granular forms to rod-shaped, depending on the age of the culture and the material under study), monotrichous (flagellum 2-3 times longer than the body, increased mobility, resembles an undulating membrane). With antibiotic treatment, motility decreases and can be converted to L-forms. Does not form spores or capsules.
Tinctorial properties:
easily dyed with aniline dyes, gr. "negative", in native preparations in the form of "shoals of fish".
Cultural properties:
grows well on conventional nutrient media, but demanding on pH (halophile), optimal pH = 8.0-9.0. In 1% alkaline peptone water, after 6-8 hours growth is noted in the form of a delicate, thin, bluish film, in 0.5 -1% Na Cl - slight turbidity; on a dense medium, smooth, transparent, bluish colonies with a smooth edge (S-shaped) grow in 10-12 hours; with prolonged cultivation, the colonies increase in size; atypical colonies are possible: cloudy, with a dense center, pigmented (brown or yellow), small , rough (R-forms), bacteria from them are not sensitive to bacteriophages, antibiotics and are not agglutinated by O-antiserum. On the alkaline-blood agora, V. cholerae asiatica does not give hemolysis zones, V. eltor - gives a hemolysis zone; on agar with thiosulfate, citrate, bile salts and sucrose (TC BS agar) forms yellow colonies
strict aerobe;
optimal growth temperature 37 °С;
cultivation time (6-8-10-12-24 hours).
Biochemical properties:
active, break down glucose, maltose, lactose, glycogen, mannitol with the formation of acid without gas, liquefy gelatin in the form of a funnel, form indole, reduce nitrates to nitrites (nitrosoindole test), decompose urea, starch. According to the ability to ferment sucrose, arabinose and mannose, all vibrios are divided into 6 groups according to Heiberg's classification. Vibrio cholerae belong to group 1 (Heiberg's triad) - they break down sucrose and mannose and do not break down arabinose.
Distribution ecology:
Anthroponosis, deltas of the rivers Ganges, Brahmaputra.
Infection mechanism:
Fecal-oral (10¹² class infectious dose).
Route of infection: water
Resistance: in fresh water up to 1 year
In salt water up to 1 year
In frozen water up to 2 years
Boiling for 1 min
Sensitive to UV disinfectants.
Clinic: the incubation period is from several hours to 2-6 days, more often 2-3 days. There are 3 periods:
cholera enteritis: against the background of normal temperature, a rare liquid stool, after 1-2 days vomiting joins;
Acute gastroenteritis: frequent vomiting, rumbling in the abdomen, bowel movements take the form of "rice water" - a cloudy liquid with floating mucus residues and epithelial cells; acts of defecation become more frequent, the tongue becomes covered with plaque, the amount of urine decreases, severe thirst, dehydration;
cholera algid - t 35°C, gray, bluish, wrinkled skin, Hippocrates' face "facies hippocratica": pointed nose, sunken eyes, protruding cheekbones; aphonia, hypotension. Death occurs from cardiovascular and renal failure as a result of dehydration and intoxication.
Immunity: post-infectious, persistent, long-lasting, antimicrobial and antitoxic; post-vaccination non-durable for 3-5 months.
44. Pathogenic factors:
A) endotoxin (cell wall LPS, thermostable, causes inflammation and induces the synthesis of vibriocidal antibodies)
B) exotoxin = enterotoxin = cholerogen (the main role in pathogenesis, thermolabile protein, its formation is encoded by chromosomal and plasmid genes, consists of two components: A and B. Component A consists of subunit A1 (active center) and subunit A2, binding A and B The A1 subunit activates adenylate cyclase, leading to an increase in the intracellular content of cAMP and the release of fluid and electrolytes from the cells of the Lieberkühn glands into the intestinal lumen.
Component B is non-toxic, has the ability to bind to the receptors of the epithelial cells of the small intestine, facilitating the penetration of component A into the cell.
Serovar 0139 bacteria also synthesize an exotoxin with similar properties, but in smaller quantities.
C) exotoxins LT, ST, SLT
D) permeability factor - increases the permeability of capillaries.
2. enzymes: neuraminidase = sialidase (cleaves sialic acid from epithelial glycoproteins, creating a “landing” platform for vibrios, increasing the number of cholerogen receptors by modifying tri- and disialoglycosides into monosialoglycosides
Gm1); hyaluronidase; mucinase (promotes the destruction of mucin on epithelial cells, which facilitates the absorption of toxic products), proteases, lecithinase, hemolysin V. eltor.
Structural and chemical components of the cell:
Flagella causing chemotaxis to overcome the mucous layer and interaction with epithelial cells. In Che– - mutants (that have lost the ability to chemotaxis), virulence is reduced, and in Mot- mutants (that have lost mobility), virulence disappears or decreases by 100-1000 times.
45 . Antigenic structure:
O-antigen - specific, heterogeneous: species and type antigens. There are 139 serovars for the O antigen in the genus Vibrio. The species is determined in a reaction with 01 serum, and the type with Inaba and Ogawa sera, since three serotypes are distinguished: A, B, C; A - general, AB - Ogawa, AC - Inaba, ABC - Gikoshima. They are epidemiological markers.
Vibrios agglutinating with serum 0139 were called biovar Bengal.
R-forms, mucous M-forms with altered O-antigen structure are not agglutinated by 01 antiserum, therefore, OR-antisera are used to identify OR and R dissociants.
H-antigen thermolabile, general, non-specific, protein nature. H- antigens are common for a large group of bacteria, they are divided into A and B groups: A - cholera vibrio, B - cholera-like, 6 groups.
Vibrios that are not agglutinated by sera of groups 01 are called non-agglutinated - NAG vibrios, cause cholera-like diseases.
Also, 2 more antigens were isolated from Vibrio cholerae, which stimulate the formation of vibriocidal and antitoxic antibodies.
46. To differentiate the biotypes of cholera vibrios, the ability of the El Tor vibrio to grow on a medium with the antibiotic polymyxin and cause hemagglutination of chicken erythrocytes is used.
47. For the VII cholera pandemic, two features of distribution are characteristic. The first is that "the initial introduction of infection into many countries did not end with the formation of complete epidemic prosperity, cholera took root in the territory of these countries, creating, as it were, a springboard for the further advancement of epidemics."
The second feature of the spread of El Tor cholera was that it appeared in those countries where the disease had not been recorded for many years (Cambodia, Burma, Nepal, Turkey, the USSR, countries of East Africa, etc.) or had never been detected before (South Africa, Morocco, Tunisia, Angola, New Zealand etc.), i.e. the area of this infection has expanded significantly. The possibility of spreading and rooting of cholera when it enters a previously non-endemic territory depends on the local sanitary and hygienic conditions of the population, its sanitary culture, socio-economic and natural-geographical factors that contribute to the formation of foci. The formation of secondary foci of cholera and its rooting is facilitated by the long-term preservation of El Tor vibrios in environmental objects. Long-term (observation period 14 months) existence of cholera vibrios outside the human body - in the water of a surface natural stagnant reservoir.
48. Microbiological diagnostics.
The main research method is bacteriological. The objects of study are feces, vomit, bile, sectional material, flies, water, silt, hydrobionts, wastewater. Transport medium: 1% peptone water, pH 8.2-8.6, transportation rules correspond to especially dangerous infections.
Serological method
a) seroidentification: ELISA, RIF, RPHA with antibody erythrocyte diagnosticum (RTPHA to confirm RPHA), RA with O, OR, 0139 antisera
b) serodiagnosis: RA, RPHA with erythrocyte cholera diagnosticum RHAg, lysis reaction, ELISA (for retrospective diagnosis, detection of vibrio carriers, assessment of post-vaccination and post-infection immunity).
Accelerated methods: RIF, DNA probes, PCR, immobilization of vibrios with O-cholera serum and bacteriophage.
It is necessary to identify and differentiate from V. parahaemolyticus, V. vulnificus, V. alginoluticus, V. mimicus, V. damsela, V. metschnigovii, V. proteus (finglepriori), V. albensis.
A preliminary positive response in the diagnosis of cholera is issued after 5-6 hours based on the detection in crops of cultures agglutinating on glass with cholera O-serum at a dilution of 1:100 and typical Ogawa or Inaba serum (1:50), and with a positive result of accelerated methods studies (ELISA, RIF, microagglutination, RPGA, immobilization reactions).
The final positive response is issued after 18-48 hours on the basis of isolated cultures that have typical morphological features, taking into account the data of an extended agglutination reaction with cholera sera O, OR, Ogawa, Inaba, samples with cholera diagnostic phages; belonging to Heiberg group 1.
49. treatment of acute intestinal infections is aimed at maintaining the activity of a number of functional systems, incl. providing the level of blood pressure, the mass of circulating blood, maintaining optimal values of respiratory parameters, the level of osmotic pressure and the excretion system. Using modern approaches in the treatment of acute intestinal infections, it is possible to avoid the development of such terrible complications as infectious-toxic and hypovolemic shocks, acute renal failure. Accuracy and rationality in the use of antibiotic therapy can save patients from dysbacteriosis, adequately performed oral rehydration copes with the main symptoms of acute intestinal infections in a short time.
50. Syphilis.
Department: graculecutes
Group: gr- Spirochetta
Family: Spirochactaceae
Genus: Treponema
Species: Treponema pallidum
Morphology - a microorganism of a spiral shape, d=0.12, length 15 microns, number of curls from 8-12. Under email under a microscope, it looks like a snake or an earthworm, blepharoplasts are located at the ends, in unfavorable conditions they form cysts, in the body it can form a capsule-like sheath.
Physiology: poorly stained with aniline dyes, therefore it was called pale spirochete, when stained according to Morozov - brown, when stained according to Romanovsky-Giemsa - pale pink.
Chemoorganoheterotroph, obligate anaerobe. Not cultivated on simple nutrient media.
Biochemical: poorly studied due to culture problems (infection of the rabbit in the testicle.)
Antigenic properties: Treponema antigens are poorly understood. It has been established that treponema contains protein, polysaccharide and lipid complexes. The antigenic composition of cultural and tissue treponemas is so close that it can be used for CSC in the diagnosis of syphilis. Does not form exotoxins.
Ecology is a severe anthroponotic disease, a sick person is contagious for 3-5 years, in the later stages it is not contagious.
Way of infection: sexual, contact-household, transplacental.
Resistance - when dried, heated at 55 ̊С for 15 minutes in HCl, it loses mobility, arsenic, mercury remain viable in the blood for 24 hours.
Pathogenesis and clinic: the incubation period for acquired syphilis is 2-10 weeks. (20-28 days).
The entrance gate is the mucous membranes of the genital organs, less often the oral cavity, as well as damaged skin. At the site of introduction, the pathogen multiplies and primary syphiloma is formed - a hard chancre-erosion or an ulcer with a dense base. Further, the pathogen penetrates into the lymphatic system and forms lymphangenitis, regional lymphadenitis. This is a typical clinic of primary syphilis (1.5-2 months). Then these signs disappear. The secondary period of syphilis is associated with a generalization of the process, when many lymph nodes increase, and rashes appear on the skin and mucous membranes, and damage to internal organs and the nervous system can be observed. With each subsequent relapse, the intensity of the rash is less and less pronounced, and the periods between relapses increase. The elements of the rash contain a large number of live treponema, during this period the patient is most contagious. This period lasts from 4 or more years. Further, the disease enters a long asymptomatic period, after which tertiary syphilis occurs. At the same time, gross violations and lesions of the internal organs of the CCC, SNS, bones are observed, with the formation of gum, accompanied by tissue decay and its degeneration. A characteristic clinical feature of syphilis is the absence of any complaints from the patient.
51. Immunity: neither natural nor artificial immunity arises, there is only infectious, and while it exists, a person is practically not susceptible to a new infection. Infectious immunity develops 10-11 days after the appearance of a hard chancre.
52. Laboratory diagnostics: an integrated approach is optimal, involving the simultaneous use of several methods: direct and indirect. Direct - infection of animals, different kinds microscopy. Indirect - serological tests to detect antibodies.
Specific prophylaxis and treatment: No specific prophylaxis has been developed. Non-specific prevention involves abstinence from casual sex, early detection of patients, timely and effective treatment.
53. Sexually transmitted infections include:
bacterial infections : inguinal granuloma (donovanosis), soft chancre, syphilis, venereal lymphogranuloma, chlamydia, gonorrhea, mycoplasmosis, ureaplasmosis
viral infections: HIV, genital herpes, genital warts caused by human papillomavirus, hepatitis B, cytomegalovirus (human herpesvirus type 5), molluscum contagiosum, Kaposi's sarcoma (herpes type 8);
protozoal infections: trichomoniasis fungal infection: candidiasis (thrush);
A chronic systemic venereal infectious disease affecting the skin, mucous membranes, internal organs, bones, nervous system with a successive change in the stages of the disease, caused by bacteria of the species Treponema pallidum (pallid treponema), subspecies pallidum, belonging to the genus Treponema (Treponema). It is characterized by a specific lesion of the inguinal, femoral, iliac and deep pelvic lymph nodes - a sexually transmitted infectious disease caused by chlamydia (Chlamydia trachomatis). It is one of the most common sexually transmitted infections. According to statistics, 100 million people in the world fall ill with chlamydia every year, and the number of people infected with chlamydia worldwide the globe by the most conservative estimates reaches one billion. According to WHO and numerous domestic and foreign researchers, urogenital chlamydia is one of the most common sexually transmitted diseases, therefore serious problem for modern venereology is the search for the most effective means of treating the so-called non-gonococcal inflammatory diseases organs of the genitourinary system. (from other Greek γόνος " seminal fluid"and ῥέω" flow ") - an infectious disease caused by a gram-negative diplococcus - gonococcus. Neisseria gonorrhoeae, sexually transmitted and characterized by lesions of the mucous membranes of the urinary organs. Refers to venereal diseases. With gonorrhea, the mucous membranes are most often affected by the genital tract, but the rectal mucosa, conjunctiva can be affected (in this case, the disease is called blennorrhea - a disease caused by a specific microorganism Ureaplasma urealyticum (ureaplasma urealyticum), belonging to Gram-negative microbes devoid of a cell wall.
54. Ureaplasmosis
Department: Mollicutes
Group: gr- obligate cocci
Family: Mycoplasmatacaea
Genus: Ureplasma
Species: Ureplasma Urealiticum.
Morphology:
Small coccoid forms, pronounced polymorphism. Restricted to a three-layer membrane. Under unfavorable conditions, it forms an L-shape, it is reversible.
Physiology:
Tolerant of nutrient media. Mandatory presence of urea, glucose, cholesterol and selective antibiotic-lincomycin, pH indicator (bromothymol blue).
Biochemical properties:
t optimum 35-37 ̊С (mesophylls), pH = 6.0-6.5, when urease is cleaved, the pH shifts to the right (alkali) Yu, if manganese sulfate is added, they turn golden brown.
Antigenic properties:
Antigenic polymorphism. 16 U.urealiticum serotypes, divided into serogroups A and B. Antigens include adhesin proteins, phospho and glycolipids.
Ecology:
Pathogenicity factors: adhesins
Endotoxins
Hemolysins
Exotoxins
Enzymes (phospholipase A, aminopeptidase, protease)
Way of infection: sexual,
Transplacental,
Contact household.
Pathogenesis:
It can occur both in acute and in chronic form. It can cause inflammation of any organs of the genitourinary apparatus. Men: urethra, prostate, bladder, testicles and their appendages. Women: Vagina, uterus and appendages. In men, it causes inflammation of the prostate gland, disrupts the motor activity of spermatozoa, and kills sperm. In women, untreated ureaplasmosis causes inflammation and adhesions in the fallopian tubes, leading to infertility and increasing the risk of ectopic pregnancy. In pregnant women, it can cause pathology of pregnancy and the fetus.
Laboratory diagnostics:
ELISA, PCR (polymerase chain reaction). Bacteriological (cultural method).
Similar information.