The human urinary system is a combination of organs that synthesize urine from waste products and excrete it from the body. In this system, organs are divided into urinary (kidneys) and urinary (renal pelvis, ureters, together with the bladder and urethra).
Normally, the kidneys are a paired organ, but in the case of genetic abnormalities, the kidneys can be doubled. In certain cases, one kidney can be removed surgically from a person.
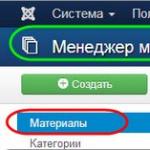
The structure of the human kidney, ureter and bladder
The kidneys are a paired organ, as mentioned earlier, have an original shape resembling beans. The size of each kidney ranges from 10 to 12 cm in length, up to 4 cm in thickness.
The mass of each kidney is about 200 grams. The kidneys are organs located in the retroperitoneal space, that is, the peritoneum covers them only in front.
Located in the lumbar region on both sides of the spine, the kidneys, getting sick, can disguise themselves as pain that occurs during lumbar osteochondrosis. In the vast majority of cases, the left kidney is slightly higher than the right.

Organs of the urinary system
Each kidney has in its arsenal a thin protective capsule with a good fat layer, which allows it to be kept at a certain level relative to the spine. When a person takes a breath, the kidneys normally move 3 cm.
In the case of a larger amplitude, one can speak of pathological mobility of the organ. The hilum of the kidney faces the spine.
Here is the renal pelvis and the main neurovascular bundle that connects the organ with the surrounding inner world. The pelvis of the kidney gradually narrows and passes into the ureter.
The kidney has two main layers: cortical and medulla. The medulla has Brown color with a red tint due to the abundance of blood vessels.
The cortical layer has a less rich blood supply, therefore it has a more friendly yellowish tint. The cortical layer contains glomeruli of nephrons, the main functional unit of the kidney.
But we will talk about nephrons a little later. The medulla consists of numerous pyramids, on the tops of which are micropapillae.
These papillae pass urine formed in the parenchyma into small calyxes, which unite into large calyxes and these, in turn, into the renal pelvis. The renal pelvis can be ampullar or branched in structure, and intra- or extra-renal in location.
Features of the location and structure of the renal pelvis are often the causes of the development of a particular kidney disease. The blood supply to the kidney is provided by the renal artery, which originates from the abdominal aorta, and by the renal vein, which flows into the system of the inferior vena cava.
Human urinary system: kidneys

Kidneys - urinary organ
The kidneys are real heroes and indispensable workers for the body. Normally, in three minutes, the renal system pumps all the blood circulating in the body.
About 100 ml of urine is filtered per minute in the nephrons of the kidney. Thanks to this, a healthy person is able to excrete from one and a half to two liters of urine every day, depending on the amount of liquid drunk.
The volume of daily urine excreted is always less by about 300-500 ml of the volume of liquid drunk per day. Blood through the renal system does not just pass through, along the way it gets rid of many unnecessary metabolites and is cleansed. This is facilitated by millions of nephrons located in the kidneys.
Nephron- is the main functional unit of the kidneys, thanks to which the metabolism in the blood is carried out. The nephron consists of a glomerulus of vessels and tubules.
In the vascular network of nephrons, blood is processed and the formation of primary urine, rid of unnecessary metabolic products. Primary urine has a low specific gravity and contains much-needed sugars and other nutrients.
Primary urine enters the tubules, where it is reprocessed and essential nutrients are absorbed from the primary urine back into the bloodstream. The resulting urine has a higher specific gravity, contains metabolic products. It is she who is excreted from the body every day.
Human urinary system: ureter
The ureter is a hollow muscular organ (tube) about 30 cm long that goes from the renal pelvis to the bladder. Urine produced in the renal system enters the bladder through muscle contractions of the ureter.
Bladder It is a hollow muscular organ, which in an empty state looks like a bag, and a small ball filled with urine. The bladder is located retroperitoneally in the area behind the pubic joint.
When the bladder does not contain urine, it does not cause any sensations in a person. However, when the amount of urine received exceeds 300 ml or more, a person has an urge to urinate.
The capacity of the bladder is different for each individual, but the mechanism of the bladder is the same. The number of urination depends not only on the characteristics of the body, but also on the diet, ambient temperature, and human diseases.
Normally, the number of urination of a person ranges from 4 to 8 times a day. Urine is expelled from the bladder through the urethra.

Bladder - urinary organ
The task of the urinary system is to remove human body many slags, toxins and other unnecessary metabolic products.
The first stage of blood filtration occurs at the level of the glomeruli of the nephron. Here, large protein molecules are selected, which are returned back to the bloodstream.
The liquid left without protein enters the tubules of the nephron. It should be noted that out of 1200 liters of liquid passed through the filter, about 180 liters of broth containing molecules of substances dissolved in blood plasma enter the tubules.
And only a maximum of two liters of fluid are excreted by the urinary system to the outside. The rest of the lion's share of the liquid, rich in nutrients, is sent back to the bloodstream.
If we imagine for a moment that this a complex system stop working, then the person will lose all their fluid in a matter of minutes. This is a condition incompatible with life.
In the cells of the kidneys, a strict selection of nutrients occurs, where the cells quickly and accurately determine which substance to remain in the blood, and which one needs to be eliminated.
So, what are the main functions of the human urinary system?
Firstly, the kidneys provide a constant composition of the necessary substances and the necessary volume of fluid in the body. This is also called maintaining homeostasis.
Secondly, the kidneys provide the blood with the necessary electrolytes, organic and inorganic salts in the body. Those. The kidneys provide acid-base balance, which is vital for the body.
In addition, the kidneys are involved in protein, fat and carbohydrate metabolism organism, and also ensure the maintenance of normal blood pressure.
Thirdly, the kidneys are involved in the production of biologically active substances and enzymes in the body that control blood pressure, the exchange of magnesium, calcium, potassium and sodium in the blood, as well as the formation of red blood cells.
Fourth, the kidneys are able to create substances that change the sensitivity of nephrons to certain hormones. This is important point in creating a normal hormonal background in the body.
In addition, if necessary, the kidney cells themselves are able to destroy hormones and deprive them of their activity, neutralizing them in a timely manner. The constant destruction of hormones contributes to the regular renewal of the hormonal background of the blood, which to some extent contributes to the rejuvenation of the blood.
In addition, due to the uniform excretion of fluid, a constant osmotic pressure of fluids throughout the body is ensured. Through the development of the active form of vitamin D, participation in bone formation is ensured. Thanks to the renin-angiotensin system, a constant blood pressure is maintained.
The main signs of damage to the urinary system can be: frequent and painful urination, acute delay urine, bloody urine, colorless urine with infrequent urination, high blood pressure that does not decrease after taking antihypertensive drugs pain in the lower abdomen. In all cases involving a violation of the urinary system, it is necessary to contact a specialist. Kidney damage can often be life-threatening.
The structure and functions of the urinary system
Isolation is the process of removing waste products from the body. harmful products metabolism. The excretion of end products of metabolism involves the kidneys, lungs, sweat glands and intestines. CO 2 and water vapor are excreted through the lungs. A small amount of water and urea and mineral salts dissolved in it are excreted through the sweat glands. Most of the metabolic products are excreted through the urinary system.
The main organ of excretion is the kidneys. They have a complex structure, which reflects the complexity of their functions. In addition to the kidneys, the excretory organs include the ureter, bladder, and urethra. The kidneys are a paired organ that has a bean-like shape and weighs up to 100 g. The kidneys are located in abdominal cavity adjacent to its posterior wall at the level of the lumbar vertebrae. The kidney is covered on the outside with a very dense connective tissue capsule, which is surrounded by a fatty capsule. Kidney tissue consists of two layers: outer - cortical and inner - cerebral. The medulla forms 15-20 pyramids. In the middle of the pyramids, thin tubes pass, ending in holes in the papillae, which protrude into a small cavity - the renal pelvis. The kidney has a complex microscopic structure and contains about 1 million structural and functional units - nephrons. The nephron consists of a capsule (in the form of a two-layer bowl), which contains a tangle of capillaries, and a system of tubules. The walls of the tubules are formed by a single layer of epithelial cells. The capsule is located in the cortical layer, a tortuous tubule of the first order departs from it, which goes to the medulla and, straightening, forms a loop. The loop returns to the cortical layer and there forms a convoluted tubule of the second order, flows into the collecting duct. The collecting ducts, merging, open into the cavity of the renal pelvis, from which the ureters depart.
Urine is formed from blood plasma. The process of urine formation begins in the capsules of the outer layer of the kidneys. When the blood passes through the capillaries of the glomeruli, water and substances dissolved in it are displaced (filtered) from its plasma. Filtration is carried out because the vessel that brings blood to the glomerulus, wider than the vessel, takes blood out of it. A high pressure is created in the glomerulus, two or more times higher than the blood pressure in other capillaries. The filtered liquid is called primary urine. Up to 150-180 liters of primary urine can be formed in the body per day. Primary urine does not differ from blood plasma in terms of the concentration of dissolved substances. In addition to dissimilation products, it contains amino acids, glucose, ions of inorganic substances, etc. In primary urine, unlike blood plasma, there are no proteins, since they are not filtered. Thus, primary urine is a blood plasma filtrate, and the main filtering force is blood pressure in the capillary glomerulus.
From the capsules, the primary urine passes into the primary tubule, then into the secondary tubule, densely entwined with a network of capillaries. In this part of the nephron, most of the water and some substances are absorbed into the blood: glucose, amino acids, proteins, vitamins, and inorganic ions. The primary urine that enters the collection tube is called secondary. It contains urea, uric acid, ammonia, etc. Up to 1.5 liters of secondary urine can form per day. If the kidneys are functioning normally, then there is no protein and glucose in the secondary urine. From the tubules, secondary urine is collected in the renal pelvis, and then through the ureters enters the bladder. Filling the bladder leads to stretching of its wall. The nerve endings that are in the wall are irritated, signals are sent to the central nervous system, and the person is attracted to urination. It is carried through the urethra and is under control nervous system.
Kidney functions excretory; regulation of the volume of blood, lymph and tissue fluid, ensuring the constancy of the osmotic pressure and ionic composition of the fluids of the internal environment of the body; regulation of blood pressure and hematopoiesis.
Violation of the kidneys. Prevention of diseases of the excretory organs
Violations or cessation of kidney function is caused by infection in the renal parenchyma. Contribute to this hypothermia of the body, kidneys, colds. Kidney diseases also develop in case of poisoning with salts of heavy metals, drugs, acids, etc. Bad influence the kidneys are affected by the consumption of too spicy food. Alcohol affects the cells of the epithelium of the kidneys, disrupts or stops the formation of urine. Often, kidney stones form in diseased kidneys.
To prevent kidney disease, you should adhere to certain hygiene requirements: eat right, treat teeth, sore throat in a timely manner, harden your body, be careful with various poisons, take medicines only as prescribed by a doctor, and observe personal hygiene.
The human urinary system performs the function of removing toxins, unnecessary, harmful compounds, while remaining in the body required amount mineral salts and water. This task is realized through the formation of urine in the kidneys in a certain volume and with a certain concentration.
The structure of the urinary system.
Its structure includes organs that produce urine (kidneys), accumulate and excrete urine from the body (bladder, ureters).
The kidneys, located in the space behind the peritoneum on both sides of the spine, are bean-shaped. The left kidney is slightly higher than the right. The upper edges of this paired organ are close to the spine, the lower ones are distant.
In the kidney, the lower and upper poles, the inner and outer edges are determined. In the center of the inner edge there is a gate (recess). Through them, nerves and arteries enter the organ, the ureter and vein exit. The combination of these elements forms the renal stalk.
A fatty capsule, its own membrane and connective tissue fascia surround each kidney. The substance of the kidney includes two layers - cerebral and cortical. The first is represented by twelve to fifteen cone-shaped formations. They are called pyramids. The cortex seeps between the nearby pyramids. The cortical layer has a thickness of four to thirteen millimeters.
The urinary system has several regulatory mechanisms.
The amount of water contained in the body affects the concentration of urine. An excessive volume of water contributes to the inhibition of secretion in the pituitary gland, which controls the absorption of salts and water. With a lack of water, sensitive special formations (osmoreceptors) are excited. In this case, ADH is released into the blood, which contributes to the reabsorption (reabsorption) of water.
The urinary system carries out, together with urine, the excretion of water, salt, and urea. These components are also excreted through the lungs, skin, intestines, salivary glands, however, they are not able to replace the kidneys.
Including the stage of filtering fluid from the blood, secretion and reabsorption, is carried out in the nephrons ( constituent parts renal tissue). Each nephron contains the renal (Malpighian) bodies, which provide the filtration process, and the urinary tubules. The body is represented by a hemispherical double-walled bowl. The gap between its walls covers the capillary glomerulus. A tubule also emerges from the gap.
Intravascular pressure (70-90 mm Hg) contributes to the seepage of the liquid part of the blood into the nephron capsule. This process is called filtration, the leaked liquid, respectively, is called "filtrate" (primary urine).
The urinary system forms a filtrate, consisting mainly of water. The concentration of low molecular weight substances in the primary urine is approximately the same as in the blood plasma. As the filtrate moves through the tubules, its composition is constantly changing, eventually becoming the final urine. The average volume of urine is about one and a half liters per day.
The urinary system also includes the bladder in its structure. This organ performs the function of storing urine. A powerful shell of muscles is located in the wall of the organ. With its reduction, the volume of the bladder cavity decreases. In the area of the openings of the ureters, the internal opening of the urethra are sphincters (compressors). They regulate the flow of urine.
Tubes (ureters) fit to the bottom of the bladder.
The excretion of urine to the outside is carried out through the urethra, which exits the bladder.
The human urinary system is an organ where blood is filtered, waste is removed from the body, and certain hormones and enzymes are produced. What is the structure, scheme, features of the urinary system is studied at school in anatomy lessons, in more detail - in a medical school.
The urinary system includes such organs of the urinary system as:
- ureters;
- urethra.
The structure of the human urinary system is the organs that produce, accumulate and excrete urine. The kidneys and ureters are the components of the upper urinary tract(VMP), and the bladder and urethra - lower parts urinary system.
Each of these bodies has its own tasks. The kidneys filter the blood, clearing it of harmful substances and producing urine. The urinary system, which includes the ureters, bladder, and urethra, forms the urinary tract, which acts as a sewage system. The urinary tract carries out the removal of urine from the kidneys, accumulating it and then removing it during urination.
The structure and functions of the urinary system are aimed at efficient filtration of blood and removal of waste products from it. In addition, the urinary system and skin, as well as the lungs and internal organs maintain homeostasis of water, ions, alkali and acid, blood pressure, calcium, red blood cells. Maintaining homeostasis is importance urinary system.
The development of the urinary system in terms of anatomy is inextricably linked with the reproductive system. That is why the human urinary system is often referred to as the genitourinary system.
Anatomy of the urinary system
The structure of the urinary tract begins with the kidneys. This is the name of a paired bean-shaped organ located in the back of the abdominal cavity. The task of the kidneys is to filter waste, excess ions and chemicals in the process of making urine.
The left kidney is slightly higher than the right one because the liver on the right side takes up more space. The kidneys are located behind the peritoneum and touch the muscles of the back. They are surrounded by a layer of adipose tissue that holds them in place and protects them from injury.
The ureters are two tubes 25-30 cm long, through which urine flows from the kidneys to the bladder. They go on the right and left side along the ridge. Under the influence of gravity and peristalsis of the smooth muscles of the walls of the ureters, urine moves towards the bladder. At the end, the ureters deviate from the vertical line and turn forward towards the bladder. At the point of entry into it, they are sealed with valves that prevent urine from flowing back into the kidneys.

The bladder is a hollow organ that serves as a temporary reservoir for urine. It is located along the midline of the body at the lower end of the pelvic cavity. In the process of urination, urine slowly flows into the bladder through the ureters. As the bladder fills, its walls stretch (they are able to accommodate from 600 to 800 mm of urine).
The urethra is the tube through which urine exits the bladder. This process is controlled internally and external sphincters urethra. At this stage, the female urinary system is different. The internal sphincter in males is made up of smooth muscle, while the female urinary system does not. Therefore, it opens involuntarily when the bladder reaches a certain degree of distension.
The opening of the internal sphincter of the urethra feels like a desire to empty the bladder. The external urethral sphincter consists of skeletal muscles and has the same structure in both men and women, and is controlled arbitrarily. A person opens it with an effort of will, and at the same time, the process of urination takes place. If desired, during this process, a person can voluntarily close this sphincter. Then the urination will stop.
How filtering works
One of the main tasks performed urinary system is blood filtration. Each kidney contains a million nephrons. This is the name of the functional unit where blood is filtered and urine is produced. Arterioles in the kidneys deliver blood to structures made up of capillaries that are surrounded by capsules. They are called renal glomeruli.
When blood flows through the glomeruli, most of the plasma passes through the capillaries into the capsule. After filtration, the liquid part of the blood from the capsule flows through a number of tubes that are located near the filter cells and are surrounded by capillaries. These cells selectively absorb water and substances from the filtered fluid and return them back to the capillaries.

Simultaneously with this process, the waste products of metabolism present in the blood are excreted into the filtered part of the blood, which at the end of this process turns into urine, which contains only water, waste products of metabolism and excess ions. At the same time, the blood that leaves the capillaries is absorbed back into the circulatory system along with nutrients, water, ions, which are necessary for the functioning of the body.
Accumulation and excretion of waste products of metabolism
The krina produced by the kidneys travels through the ureters to the bladder, where it collects until the body is ready to empty. When the volume of the fluid filling the bladder reaches 150-400 mm, its walls begin to stretch, and the receptors that respond to this stretch send signals to the brain and spinal cord.
From there comes a signal aimed at relaxing the internal urethral sphincter, as well as a feeling of the need to empty the bladder. The process of urination can be delayed by willpower until the bladder is inflated to its maximum size. In this case, as it stretches, the number of nerve signals will increase, which will lead to more discomfort and strong desire empty.
The process of urination is the release of urine from the bladder through the urethra. In this case, urine is excreted outside the body.
Urination begins when the muscles of the urethral sphincters relax and urine flows out through the opening. Simultaneously with the relaxation of the sphincters, the smooth muscles of the bladder walls begin to contract to force urine out.
Features of homeostasis
Physiology urinary system manifested in the fact that the kidneys maintain homeostasis through several mechanisms. In doing so, they control the release of various chemicals in the body.
The kidneys can control the excretion of potassium, sodium, calcium, magnesium, phosphate, and chloride ions into the urine. If the level of these ions exceeds the normal concentration, the kidneys can increase their excretion from the body in order to maintain normal level electrolytes in the blood. Conversely, the kidneys can store these ions if their blood levels are below normal. At the same time, during blood filtration, these ions are reabsorbed into the plasma.
The kidneys also make sure that the levels of hydrogen ions (H+) and bicarbonate ions (HCO3-) are in balance. Hydrogen ions (H+) are produced as a natural by-product of the metabolism of dietary proteins that accumulate in the blood over time. The kidneys send excess hydrogen ions into the urine to be removed from the body. In addition, the kidneys reserve bicarbonate (HCO3-) ions in case they are needed to compensate for the positive hydrogen ions.

Isotonic fluids are essential for the growth and development of body cells to maintain electrolyte balance. The kidneys maintain osmotic balance by controlling the amount of water that is filtered and eliminated from the body in the urine. If a person consumes a large amount of water, the kidneys stop the process of water reabsorption. In this case, excess water is excreted in the urine.
If the tissues of the body are dehydrated, the kidneys try to return as much as possible to the blood during filtration. Because of this, the urine is very concentrated, with a large amount of ions and waste products of metabolism. Changes in water excretion are controlled by antidiuretic hormone, which is produced in the hypothalamus and anterior pituitary gland to retain water in the body when it is deficient.
The kidneys also monitor the level of blood pressure, which is necessary to maintain homeostasis. When it rises, the kidneys reduce it, reducing the amount of blood in the circulatory system. They can also reduce blood volume by reducing the reabsorption of water into the bloodstream and producing watery, dilute urine. If the blood pressure becomes too low, the kidneys produce the enzyme renin, which constricts the blood vessels and produces concentrated urine. Wherein more water remains in the blood.
Hormone production
The kidneys produce and interact with several hormones that control various systems organism. One of them is calcitriol. it active form vitamin D in the human body. It is produced by the kidneys from precursor molecules that occur in the skin after exposure to ultraviolet radiation from solar radiation.
Calcitriol works in conjunction with parathyroid hormone to increase the amount of calcium ions in the blood. When their level falls below the threshold level, the parathyroid glands begin to produce parathyroid hormone, which stimulates the kidneys to produce calcitriol. The action of calcitriol is manifested in the fact that small intestine absorbs calcium from food and transfers it to the circulatory system. In addition, this hormone stimulates osteoclasts in the bone tissues of the skeletal system to break down the bone matrix, which releases calcium ions into the blood.
Another hormone produced by the kidneys is erythropoietin. It is needed by the body to stimulate the production of red blood cells, which are responsible for transporting oxygen to tissues. At the same time, the kidneys monitor the state of the blood flowing through their capillaries, including the ability of red blood cells to carry oxygen.

If hypoxia develops, that is, the oxygen content in the blood falls below normal, the epithelial layer of capillaries begins to produce erythropoietin and throws it into the blood. Through the circulatory system, this hormone reaches the red bone marrow, where it stimulates the rate of production of red blood cells. Thanks to this, the hypoxic state ends.
Another substance, renin, is not a hormone in the strict sense of the word. This is an enzyme that the kidneys produce to increase blood volume and pressure. This usually occurs as a reaction to a drop in blood pressure below a certain level, loss of blood, or dehydration of the body, for example, with increased skin sweating.
Importance of Diagnosis
Thus, it is obvious that any malfunction of the urinary system can lead to serious problems in the body. Pathologies of the urinary tract are very different. Some may be asymptomatic, others may be accompanied by various symptoms including abdominal pain when urinating and various secretions in urine.
Most common causes pathologies are infections of the urinary system. The urinary system in children is especially vulnerable in this regard. The anatomy and physiology of the urinary system in children proves its susceptibility to diseases, which is aggravated by the insufficient development of immunity. At the same time, even the kidneys healthy child work much worse than an adult.
To prevent the development of serious consequences, doctors recommend taking a general urine test every six months. This will allow timely detection of pathologies in the urinary system and treatment.
1. The meaning and structure of the urinary system.
The value of the excretion of waste products of the body, In the process of metabolism in the cells, end products are formed. Among them, there may be substances that are toxic to cells. So, during the breakdown of amino acids, nucleic acids and other nitrogen-containing compounds, toxic substances are formed - ammonia, urea and uric acid, which, as they accumulate, are subject to excretion from the body. In addition, excess water, carbon dioxide, poisons that come with inhaled air, absorbed food and water, excess vitamins, hormones, drugs, etc. must be removed. With the accumulation of these substances in the body, there is a danger of violation of the constancy of the composition and the volume of the internal environment of the body, which can affect human health.
Organs of excretion and their functions. The excretory function is performed by many organs. So, the lungs remove carbon dioxide, water vapor, and some volatile substances from the body, such as ether vapor, chloroform vapor during anesthesia, and alcohol vapor during intoxication. Sweat glands remove water and salts, small amounts of urea, uric acid, and with intense muscular work - lactic acid. The salivary and gastric glands secrete some heavy metals, a number of medicinal substances, and foreign organic compounds. An important excretory function is performed by the liver, removing hormones (thyroxine, folliculin), hemoglobin breakdown products, nitrogenous metabolism and many other substances from the blood. The pancreas and intestinal glands remove salts of heavy metals, medicinal substances. However, the main role in the excretion processes belongs to specialized organs - the kidneys. To essential functions kidneys include participation in the regulation of: 1) the volume of blood and other fluids of the internal environment, 2) the constancy of the osmotic pressure of blood and other body fluids, 3) the ionic composition of fluids of the internal environment and the ionic balance of the body, 4) acid-base balance, 5) excretion of the end products of nitrogen metabolism and foreign substances from the body. Thus, the kidneys are an organ that provides homeostasis of the internal environment of the body.
The structure of the urinary system The organs that make up the urinary system are responsible for filtering the blood and removing waste fluid from the body. The urinary system consists of the following formations: two kidneys, which are located on back wall the abdominal cavity directly above the lower back on either side of the spine; two ureters that connect the kidneys to the bladder; bladder and urethra (urethra) which connects the bladder to the outside.
How the urinary system works The outer part of the kidneys (the cortex) contains thin tubes that filter waste materials from the blood. The filtered liquid enters the central part of the kidneys - the medulla, in which some substances are reabsorbed from it. The resulting fluid (urine) is sent through the ureters to the bladder, which is in a closed state thanks to a ring of muscles (sphincter). The accumulated urine periodically exits the bladder through the urethra.
Rice. 1. The structure of the urinary system: 1 - kidney; 2 - kidney gate; 3 - ureter; 4 - bladder; 5 - urethra; 6 - adrenal glands.
Functions of water-electrolyte metabolism: water in the body plays a transport role, filling cells, interstitial (intermediate) and vascular spaces, is a solvent of salts, colloids and crystalloids and takes part in biochemical reactions. All biochemical fluids are electrolytes, since salts and colloids dissolved in water are in a dissociated state. It is impossible to list all the functions of electrolytes, but the main ones are: maintaining osmotic pressure, maintaining the reaction of the internal environment, participating in biochemical reactions. The main purpose of acid-base balance is to maintain a constant pH of body fluids as the basis for normal biochemical reactions and, therefore, vital activity. Metabolism occurs with the indispensable participation of enzymatic systems, the activity of which closely depends on chemical reaction electrolyte. Together with water-electrolyte exchange acid-base balance plays decisive role in ordering biochemical reactions. Buffer systems and many physiological systems of the body take part in the regulation of acid-base balance.
Regulation of osmotic blood pressure and extracellular water volume. The osmotic pressure of the blood is an important indicator of homeostasis. Osmoreceptors that respond to its changes are located in the nuclei of the hypothalamus, in the liver, heart, kidneys, and other organs. Water reabsorption is increased by the action of the antidiuretic hormone, ADH (vasopressin), which is secreted from the pituitary gland in response to a decrease in blood osmotic pressure. The content of vasopressin in the blood depends on the daily rhythm, i.e. during the day a person produces less of it than at night. With violations of the regulation of the formation of ADH, nocturia can be observed - the nighttime excretion of large amounts of urine. The formation of ADH significantly increases with painful stimuli in response to the action of a painful stimulus, pain anuria occurs, i.e. cessation of urine output. With inhibition of vasopressin release, diuresis sharply increases (more than 10-20 final urine), and polyuria develops. With a decrease in the level of sodium ions in the blood, the production of aldosterone hormones increases, which increases the activity of the sodium-potassium pump in the renal tubules and increases the reabsorption of sodium from the primary urine. When too high level sodium ions in the blood increases the production of natriuretic hormone in the hypothalamus and atria, which, on the contrary, reduces the reabsorption of sodium in the renal tubules and increases its excretion in the urine.
Hematopoiesis (hematopoiesis), the process of formation, development and maturation of blood cells - leukocytes, erythrocytes, platelets hematopoietic organs There are embryonic (intrauterine) hematopoiesis, which begins at a very early stages embryonic development and leads to the formation of blood as a tissue, and postembryonic hematopoiesis, which can be considered as a process of physiological blood renewal. In an adult organism, mass death continuously occurs shaped elements blood, but dead cells are replaced by new ones, so that total blood cells is preserved with great constancy.
The structure of the reticular (hematopoietic) tissue. In red bone marrow there are so-called stem cells - the precursors of all blood cells, which (normally) come from the bone marrow into the bloodstream already fully mature. No more than 20% of stem cells simultaneously take part in the process of hematopoiesis, while most of them are at rest. Hematopoietic stem cells are able to differentiate into different types of blood cells. The process of differentiation takes place in several stages. Thus, the process of erythropoiesis (erythrocyte formation) includes the following stages: proerythroblasts, erythroblasts, reticulocytes, and, finally, erythrocytes. The duration of erythropoiesis is 2 weeks.
Granulocytes are also formed in the bone marrow, with neutrophils, basophils and monocytes coming from one (pluripotent) cell - the precursor of neutrophils and basophils, and eosinophils - from another (unipotent) cell - the precursor of eosinophils. As granulocytes differentiate, the size of the cells decreases, the shape of the nucleus changes, and granules accumulate in the cytoplasm. The process of development of granulocytes is morphologically distinguished into 6 stages: myeloblast, promyelocyte, myelocyte, metamyelocyte, stab and segmented granulocytes. Granules specific for each type of granulocytes appear at the stage of myelocytes. Cell divisions stop at the stage of metamyelocytes.
Platelets give rise to the largest (30-100 microns) bone marrow cells - megakaryocytes, which have a lobed nucleus with a polyploid set of chromosomes.
Lymphocytes, unlike other blood cells, can be formed both in the bone marrow (B-lymphocytes) and in the tissues of the immune system: the thymus gland (thymus) (T-lymphocytes), in the lymph nodes, in other lymphoid organs. A mature lymphocyte is much smaller than its progenitor cell, the lymphoblast, but many lymphocytes can, when stimulated with an antigen, enlarge and reacquire the morphology of a lymphoblast.
Thus, the bone marrow plays a central role in immune system, since B-lymphocytes are formed in it, and there is also a large number of plasma cells synthesizing antibodies. In addition to hematopoiesis, in the bone marrow, as in the spleen and liver, old and defective blood cells are removed from the bloodstream.
2. The structure of the urinary organs.
The external structure of the kidneys
Rice. 2. Kidneys and ureters.
right kidney
left kidney
adrenal glands
abdominal aorta
inferior vena cava
renal artery
renal vein
ureter
ureter
The kidneys are excretory organs located behind the peritoneum in the lumbar region on the back wall of the abdominal cavity at the level from the XII thoracic to the I, II lumbar vertebrae on the sides of the spine. Right kidney lies 1.5 cm below the left. The kidney is bean-shaped. Its surface is smooth and dark red in color. The kidney has two poles - upper and lower, two edges - internal concave and external convex, two surfaces - anterior and posterior. On the inner edge of the kidney are the gates of the kidney, through which the renal artery, renal vein, lymphatic vessels, nerves and ureter pass. The mass of each kidney of an adult is about 150 g, the length is about 10 cm. The kidney is surrounded by its own dense connective tissue membrane in the form of a thin smooth film directly adjacent to the substance of the kidney. This shell can be easily separated. On top of this shell is a layer of loose adipose tissue that forms the fatty capsule of the kidney. The fatty capsule contributes to shock absorption, protection and more durable fixation of the kidney in a certain position. The importance of this function of the fat capsule is evident from the following: during prolonged fasting, fat, as a spare nutrient, from the fatty capsule of the kidneys is consumed last. Omission of the kidneys - a pathology that occurs due to a violation of their correct position, leads to difficulty in the blood supply to the kidneys and disruption of their work. Adjacent to the upper pole of each kidney endocrine gland- adrenal.
Internal macroscopic structure of the kidneys
Rice. 3. Internal structure of the kidney (longitudinal section).
1 - a large cup; 2 - small cups; 3 - renal pelvis; 4 - ureter; 5 - medulla (renal pyramids); 6 - papillae of the pyramids; 7 - cortex.
On a longitudinal section through the kidney, it can be seen that the kidney consists of a cavity and the proper renal substance. The renal substance consists of two layers: cortical and medulla. The cortical substance occupies a peripheral position, has a thickness of about 4 mm. The medulla occupies an internal position and consists of conical formations called renal pyramids. The bases of the pyramid are directed to the periphery of the kidney, and the tops - to the cavity of the kidney. The cortical substance enters the medulla, forming the renal columns separating the pyramids. The cavity of the kidney is occupied by small and large calyces and the renal pelvis. Small cups 8 - 9. Each small cup covers the top of the pyramid. Combining several, they form large cups (there are usually two of them - upper and lower). The large calyces merge into one renal pelvis, which partially protrudes from the hilum of the kidney.
Microscopic structure of the kidneys The kidney is a complex tubular gland. The structural and functional unit of the kidney is the nephron. The nephron looks like a thin tube of microscopic diameter, about 30-50 mm long. Each kidney has about a million nephrons. The nephron begins with an enlarged area called the nephron capsule, or the Shumlyansky-Bowman capsule. The capsule is a double-walled cup or glass. The walls of the capsule are formed by a single-layer epithelium, and its inner layer is squamous epithelium. The capsule tightly covers the capillary glomerulus. This glomerulus begins at the afferent arteriole and ends at the efferent arteriole. The diameter of the afferent arteriole is larger than the efferent arteriole, therefore, increased pressure is created in the capillary glomerulus. The capillary glomerulus, together with the capsule covering it, forms the renal (Malpighian) body. Renal corpuscles lie in the cortical layer of the kidneys and are visible to the naked eye in the form of small red dots. From the capsule of the renal corpuscle, the convoluted tubule of the first order (proximal tubule) begins, which continues into the loop of Henle. The loop is followed by a convoluted tubule of the second order (distal tubule), passing into the intercalary section. The loop of Henle lies in the medulla of the kidney. The walls of the nephron are formed by a single-layer epithelium, the shape of the cells of which is different in its different parts (for example, the wall of the convoluted tubule of the first order is formed by ciliated epithelium).
Blood vessels of the kidneys
Blood enters the kidney through the renal artery, which originates from the abdominal aorta. About 25% of the blood expelled by the left ventricle enters the kidneys, which is approximately 1.5 thousand liters per day. renal artery in the kidneys, it breaks up into a system of small arteries up to the level of the arterioles of the renal corpuscles, giving rise to the capillary glomerulus. The efferent arteriole of each renal corpuscle splits into a system of capillaries that form a network around the nephron. From this network, venules and veins are formed, eventually merging into the renal vein. Thus, in the kidneys there are two systems of capillaries:
capillaries of the renal corpuscles, in which there is no change of blood from arterial to venous
capillaries covering the tubules of nephrons, in which there is a change of blood from arterial to venous.
The first network provides blood filtration, the second - metabolic processes in the kidneys.
Rice. 4. Scheme of the structure of the nephron (A), Malpighian body (B) and the epithelium of various parts of the tubule of the nephron (C).
A: 1 - malpighian body; 2 - convoluted tubule of the first order (proximal); 3 - descending section of the loop of Henle; 4 - ascending section of the loop of Henle; 5 - convoluted tubule of the second order (distal); 6 - insertion section of the nephron; 7 - common collecting tube.
B: 1,2 - outer and inner walls of the Shumlyansky-Bowman capsule; 3 - cavity inside the capsule; 4 - bringing arteriole; 5 - capillary glomerulus; 6 - efferent arteriole; 7 - cubic epithelium of the proximal tubule; 8 - microcilia of epithelial cells; 9 - flat epithelium of the loop of Henle; 10 - epithelium of the distal tubule.
The work of cells leads to the formation of harmful substances that the body needs to remove. This problem is solved by the absorption of some substances for their reuse and the removal of others. Excretion of harmful products is carried out in four ways: during breathing, with sweat, with feces and with the help of the urinary system. The latter is actually excretory system, consisting of a complex organ - the kidneys, as well as the ureters, bladder and urethra.
The urinary, or excretory, system filters the blood and removes the products of metabolism (metabolism), that is, the products resulting from the transformations that the food eaten undergoes before it is converted into digestible substances. Thus, the cells receive the necessary energy to perform their functions, and harmful substances pass through the blood to the kidneys.
Removal of harmful substances from the body
Organs of the urinary system
The kidneys filter the blood and form urine from water and harmful substances, which is excreted from the body through the urinary system.
The ureters are the channels that connect the kidneys to the bladder.
The urethra is the channel through which urine accumulated in the bladder is excreted from the body. These organs are different for men and women.
The bladder is an elastic muscular organ that collects urine from the kidneys.
3. Formation of urine.
The kidneys produce urine from the plasma of the blood flowing to them. The process of urination is divided into two stages: the formation of primary urine and the formation of secondary urine. Blood plasma under high pressure is filtered through the walls of the capillaries into the renal capsule. The walls of the capillaries and the renal capsule do not allow blood cells and large protein molecules to pass through, but some substances dissolved in the blood plasma pass through. Primary urine is a liquid formed in the cavity of the renal capsule. From the renal capsule, primary urine enters the renal tubule, the thin walls of which absorb water and some substances dissolved in it, needed by the body and release harmful substances into it. Needed by the body substances return to the blood through a network of capillaries that encircle the renal tubule, and the products of the final breakdown of substances or unnecessary compounds form secondary urine. The resulting urine flows into the renal pelvis, and from it periodically enters the bladder through the ureters. . When the bladder is filled to a certain limit, the receptors of the bladder wall are irritated, which causes a reflex contraction of its muscles and relaxation of the muscle thickenings, leading to the emptying of the bladder, i.e., to urination. The urinary reaction center is located in spinal cord and is under the control of the brain.
kidney cortex
medulla
calyces
pelvis
ureter
bladder
urethra
Nervous and humoral regulation of kidney activity
The human body is a system of highly differentiated cells, tissues, organs, the coordinated work of which is a sine qua non normal functioning of the body. On the other hand, for the normal functioning of the body, a state of homeostasis is necessary, i.e. maintenance of constancy chemical composition and physico-chemical properties of cells, tissues and the internal environment of the human body. Finally, the human body exists in conditions constant change internal and external environment to which it is necessary to constantly adapt. Integration (coordination) of the processes and functions of the body and adequate adaptive reactions of the body is carried out due to the continuous flow of regulatory processes. There are two main types of regulation of functions in the human body: nervous and humoral regulation. The first is carried out as a result of the activity of the nervous system, the second - due to the activity of the endocrine glands and other organs with secretory activity. Physiological processes in all cells, tissues, organs are under continuous regulatory influence from the nervous and endocrine systems. Thanks to this, the state of homeostasis of the body and the adaptation of the body to a specific state of the internal and external environment are most subtly and accurately maintained.
Both types of regulation have their own characteristics:
Nervous regulation
Humoral regulation
Communication with the organs to which the regulatory influence is directed is carried out along the nerve pathways.
The regulatory effect is carried out by the distribution of biologically active substances by liquid media of the body.
There is an exact "addressee" (an organ, a tissue, a group of cells) to which the regulatory action is directed.
There is no precise targeting, so a large number of organs are included in the response.
Very high speed control action, because speed of nerve impulse conduction reaches 120 - 140 m/s
The rate of regulatory action is hundreds of times lower than that of nervous regulation.
Rapid interruption of control action possible
The termination of the regulatory action is extended in time
Both types of regulation, having their own characteristics, complement each other, are interconnected, therefore it is more correct to speak of a single regulatory mechanism - neurohumoral regulation owing to which the organism exists as a whole. The main centers of coordination and coordination of the nervous and endocrine regulatory systems are the hypothalamus (the hypothalamic part of the diencephalon) and the pituitary gland. The hypothalamus and pituitary together form the hypothalamic-pituitary system. The hypothalamus produces neurohormones that enter the pituitary gland and regulate its activity. Neurohormones liberins enhance, and statins slow down the production of pituitary hormones.
4. Age features of the structure of the kidneys.
The intensity of kidney growth is not the same in different age periods. The most intensive growth takes place in the first 3 years of life, during puberty and in 20-30 years. The kidneys of newborns have a lobular structure, which is somewhat smoothed out by one year due to the growth in width and length of the urinary tubules. An increase in the volume and number of these tubules contributes to smoothing the boundaries between the lobules of the kidneys. At 5 years of age, lobulation of the kidneys in most children disappears. However, in rare cases lobulation persists throughout life. The ratio of the cortical and medulla of the kidney changes quite sharply with age. While in an adult the thickness of the cortical layer is 8 mm, and the medulla - 16 mm, in a newborn it is, respectively, 2 mm and 8 mm. Consequently, the ratio of the thickness of the cortical and medulla in adults is 1: 2, and in children - 1: 4. The growth of the cortical layer of the kidneys occurs especially intensively in the first year of life, when its thickness doubles. In the cortical substance of the kidneys of newborns, there are many small Malpighian bodies, which are quite tightly adjacent to each other. There are 50 glomeruli per unit volume of an almost newborn (in adults - 4-6, and in 8-10-month-old children - 18-20). With age, the urinary tubules, which grow in size, increase the distance between adjacent bodies more and more and at the same time move them away from the kidney capsule. The latter leads at the age of 1-2 years to the formation of a glomerular-free layer under the kidney capsule, the width of which increases up to 14 years. In the first 20 days of a child's life, the formation of new Malpighian bodies is possible. At the same time, throughout the first year in the kidney of children there are nephrons that have undergone reverse development (sclerosed). With age, their number steadily decreases. From 7 to 50 years, the reverse development of nephrons is observed quite rarely. Thus, not all nephrons that are laid down in the embryonic period develop to full maturation: some of them undergo reverse development and die. The reason for this phenomenon is that the nerve fibers grow into the kidney after the laying of nephrons, and some of them do not reach the nerve branches. These nephrons, deprived of innervation, undergo reverse development, being replaced by connective tissue, i.e. sclerosing. Nephrons of the kidneys of newborns are characterized by immaturity, which is expressed in the features of the cellular structure of the capsule. The epithelial cells of the inner leaf of the capsule are very high (cylindrical and cubic epithelium). The leaf itself covers the vascular glomerulus only from the outside, without penetrating between the individual vascular loops. With age, the height of the cells decreases: the cylindrical epithelium turns first into a cubic, and then into a flat one. Moreover, the inner leaf of the capsule begins to penetrate between the vascular loops, evenly covering them. The diameter of the glomerulus in newborns is very small, so that the total filtration surface per unit mass of the organ is much smaller than in an adult. The urinary tubules in newborns are very narrow and thin. The loop of Henle is short, its apex enters the cortical layer. The diameter of the urinary tubules, as well as the renal corpuscles, increases up to 30 years. Transverse section the convoluted tubules of the kidneys of children are 2 times narrower than those of adults. In newborns, the diameter of the tubule is 18-23 microns, in an adult - 40-60 microns. The renal pelvis in newborns and infants is most often located in the kidney parenchyma itself. The older the age, the more cases where the pelvis is located outside the renal parenchyma. At the age of 3-5, a fatty capsule of the kidney is formed, which provides a loose connection between the kidneys and the adrenal glands. With age, the vascular network of the kidneys changes. Age changes arterial system kidneys are expressed in a thickening of the outer and inner walls of the arteries and a decrease in the thickness of the middle wall. At the same time, smooth muscle cells appear in large numbers in both the inner and outer layers. Only by the age of 14, the thickness of the arterial wall of the vessels of the bumps turns out to be the same as in adults. In the venous plexus of the kidneys of newborns, it is impossible to distinguish individual trunks. The latter appear only at 6 months of age. At 2-4 years old, the structure of the kidney veins is the same as in adults. The lymphatic system of the renal pelvis in children is more closely connected with the lymphatic system of the intestine than in adults. As a result, children may develop intestinal bacteria from the intestines to the renal pelvis, which leads to the occurrence of an inflammatory process in them. In newborns, they are almost slightly higher than in adults. The upper pole of the kidneys corresponds to the lower edge of the 11th thoracic vertebra; only by 2 years the level of location of the kidneys is the same as in adults.
5.Enuresis, its causes and prevention.
Currently, enuresis is understood as involuntary urination during the night and daytime sleep in a child with unsteady control of urination, not appropriate for his age. The term "nocturnal enuresis" is not entirely accurate, because. Involuntary urination can also occur during daytime sleep. It would be correct to call this disease "sleep enuresis". However, it was decided to leave the usual name of the disease. Doctors who use this term put the right content into it.
Nocturnal enuresis should be distinguished from persistent urinary incontinence (day and night) as a consequence of congenital anatomical disorders of the urinary tract. Persistent urinary incontinence is urological disease, which after surgical intervention in most cases it is curable.
At first glance, nocturnal enuresis is a harmless disease that does not deserve special attention. However, changes that are imperceptible at first, which occur in the character of a child, are often not taken into account - isolation, secrecy, sometimes aggressiveness, etc., which can leave an imprint on a person's entire subsequent life. It is known how difficult and sometimes impossible it is to “correct” the character that has developed in an adult. In addition, we should not forget about the inconvenience in the everyday life of families where there are children with this disease. The mother has to constantly wash clothes and bedding. In the room where the child sleeps, there is a smell of urine.
In the very early age The main factor of urinary incontinence in children is most often conditioned reflex. A child, accustomed to being put on the potty at a certain time, subconsciously expects the same during sleep. Accustomed to the presence of his mother, he can wet himself at night if the mother does not respond to his call. This type of enuresis, developing at an early age, can be observed in children up to five years of age.
Another cause of enuresis in children can be uneven psychomotor development, or the so-called dysontogenetic factor. Such children are distinguished by a slower level of motor and mental development, they later begin to sit, walk, talk, etc. In some cases, excessive speed of movements or, conversely, their stiffness, may serve as evidence of uneven psychomotor development.
The cause of enuresis can be an elementary lack of attention and love from parents. This is the so-called factor of pedagogical neglect. Parents may pay too little attention to their child different reasons: someone is simply not capable of showing feelings for a child, someone is too busy at work, and someone simply thinks that one should not "spoil" a child, especially a boy, caress him too much. Children suffering from a lack of manifestations of parental feelings, as a rule, are either extremely overexcited or, on the contrary, inhibited. In this case, enuresis can be stable and very long-term.
Often, childhood enuresis can be due to the so-called minimal brain dysfunction. A similar disorder is most often observed when the parents of the child suffer from alcoholism. It is alcohol that has a traumatic effect on the child's brain system, which manifests itself, in particular, in pathological disorders of the sleep process. Enuresis in this case is a relaxation reflex acquired from parents in the form of an act of involuntary nocturnal or daytime (during sleep) urination, which is often observed in alcoholics in a state of intoxication. Children suffering from minimal brain dysfunction have a general reduced background of emotionality. The experiences and feelings of such children are shallow, superficial, self-criticism is practically absent.
Enuresis resulting from cerebral organ failure (or cerebro-organic factor) is another type of bedwetting in children. The most obvious signs in this case are increased physical activity child, excitability, frequent mood swings, conflict, pugnacity, inability to live in a team, almost complete lack of criticism of one's own shortcomings. In this case, enuresis is caused birth trauma, resulting in increased and painful excitability of the brain.
A less common cause of enuresis in children may be the so-called neurotic factor. In this case, urinary incontinence in a child is not stable - sometimes for a short or even quite a long period of time, he can remain dry in bed. Urinary incontinence is observed against the general background of an increase in the emotional state, feelings of fear or anxiety, when the child is frightened or simply overexcited by something, that is, in this case, the cause of urinary incontinence should be sought in stressful situation. Stress is a push; if this is a short-term stress, then enuresis eventually stops and resumes only with the repeated influence of another stress. If the child lives in constant stress (for example, he is haunted by nightmares, he is afraid of the dark, etc.), then, accordingly, enuresis is more stable and permanent. As a rule, such children are very worried about their deficiency and do their best to hide enuresis from their parents and other family members.
Often, enuresis affects those flyers who are not similar in temperament to their parents, especially to the mother (or to that of the family members who are raising the child).
If enuresis occurs at any age, you should consult a doctor as soon as possible, because. sometimes simple tips regarding hygienic content can give a good effect. In the absence of treatment, enuresis can continue for a long time, leading to disturbances in mental sphere child. Currently, there are a number of effective treatments for enuresis. Treatment is prescribed strictly individually, because the means that are effective in treating one child may be useless for another.
Psychotherapeutic treatment is carried out as in outpatient settings as well as in the hospital. Hypnotic sessions are most often group.
Another method of treating nocturnal urinary incontinence is the use of conditioned reflex therapy using the Laskov apparatus. The principle of its action is that during involuntary urination, the first drop of urine closes an electrical circuit, resulting in electrocutaneous irritation that contributes to the awakening of the child, which coincides with the contraction of the external sphincter. Urination is interrupted, the child wakes up and goes to the toilet. After a series of repetitions, a conditioned reflex awakening at the onset of involuntary urination.
One of the ancient methods of treating various diseases in both children and adults is acupuncture. It is also used for nighttime urinary incontinence. This method of treatment is not always effective, and only a doctor can determine the indications for the treatment of children with enuresis.
From medications in our country and abroad, melipramine is most widely used, which can only be prescribed by a doctor. The drug is used both in hospital conditions and in outpatient practice. Due to the fact that the drug has some side effects, it is important that parents carefully monitor the child and immediately inform the attending physician about the observed deviations.
A child suffering from nocturnal urinary incontinence should be engaged in hardening, which serves as a means of prevention colds. These diseases can provoke the age of enuresis after successful treatment of the disease, and it is known from practice that cooling of an unhardened healthy body often leads to colds.
Enuresis is not only a medical, but also a pedagogical problem, therefore, in the complex treatment of this disease, a special role should belong to the child's parents. In children suffering from enuresis, there may be changes in behavior, character, which serves as an obstacle to communication with others, complicates being in a team. Pedagogical work parents should aim to strengthen the child's desire to recover. It is necessary to create an environment in which external stimuli are excluded during the child’s sleep, as well as worries and experiences. Much attention should be paid to normal relationships in the family.
Similar information.