We all remember how our teeth once became loose when we were children. At a certain age, at the moment when baby teeth are replaced by permanent ones, this phenomenon is completely normal (although not very pleasant). Alas, there are cases when the teeth of a fully grown, and sometimes elderly, person begin to become loose.
This serious problem, which indicates that not everything is in order with your tissues. If you notice that one or more teeth have become unusually mobile, do not hesitate to visit a doctor. Only timely intervention by a specialist will help prevent the development of complications and tooth loss.
What does a moving tooth indicate?
The causes of loose teeth can be different, but the main ones are: various diseases periodontal disease, namely periodontitis and periodontal disease. These diseases are characterized by inflammatory processes that occur in bone tissue.
A tooth can also become mobile due to - in this case, the gums begin to bleed. Causes of gingitis - features of its course metabolic processes in your body plus insufficient quality dental care. It all starts, as a rule, with plaque, which then transforms into tartar. As a result, the tooth tissue becomes thin, vulnerable, loose, and the tooth begins to “walk.”
With periodontitis and periodontal disease, the bone tissue becomes inflamed. It might even start purulent process. Often a so-called “pocket” is formed in the gum. Because of it, the teeth of the upper and lower jaw They close incorrectly and eventually begin to move.
What can you do
By visiting our specialist and telling him about your problem, you will receive comprehensive advice on how to save your teeth. You will also be offered in-office treatment methods. The most common and effective of them is. This is a type in which healthy and mobile teeth are combined with the help of a special design - a splint. The load on periodontal tissue becomes less, is removed, and the chance that your teeth will remain with you increases sharply. In addition to using the tire, they also use special drugs, which help relieve inflammation and “calm” tissue.

The splinting process itself will be slow, but overall painless procedure: on teeth with inside a special thin but strong arch will be fixed, which will hold them in place, while helping to properly distribute the chewing load. This design can serve for a very long time. If necessary, it can be replaced. It is almost not felt in the mouth.
However, before installing the splint, the doctor will first put all your teeth in order: clean off plaque, treat if any is found. After all, any additional structure in the mouth requires additional attention to hygiene.
It can be extremely difficult to completely get rid of it. But splinting can extend the life of your teeth quite significantly.
Is it possible to prevent tooth mobility?
There is no specific prevention.
- don't forget to visit regularly,
- carefully monitor your diet,
- avoid vitamin deficiency and decreased immunity,
- take good care of your oral cavity: brush your teeth daily with a brush and floss, carefully getting rid of food fragments that tend to get stuck in the interdental spaces.
In addition, you should stop smoking - it has an extremely negative effect on the health of your gums.
The only exception in this case is a mechanical injury to the jaw, against the background of which the patient’s teeth may become loose and even spontaneously be lost. In other situations, the appearance of such problems is noted mainly in old age or in the presence of accompanying pathologies. The appearance of such a symptom as tooth mobility should never be underestimated or ignored. Over time, this can even lead to edentulism (complete or partial loss of teeth). It must be said that when certain diseases periodontal disease, traditional restoration is not always possible. We urge you to promptly contact specialists if there are such warning signs, or better yet, regularly attend dental examinations for preventive purposes.
Physiological and pathological mobility
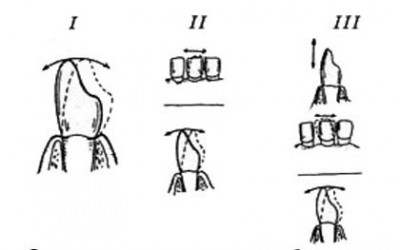
Physiological tooth mobility is invisible to you, but it is activated whenever you eat solid food. This is due to the presence of specific depreciation ligamentous apparatus, thanks to which the chewing load is distributed evenly across the jaws. In the absence of such a reflex, our teeth would very quickly deteriorate and begin to collapse. Especially those who, by definition, have to withstand the majority of the functional load. Noticeable tooth mobility is almost always pathological in nature. Most often, the appearance of such a symptom is associated with the development of periodontitis - an inflammatory process in periodontal tissues, due to which gradual destruction of the ligamentous apparatus and jaw bones occurs. usually has infectious genesis, and must be treated urgently when symptoms are first noticed. Subject to availability pathological reasons, tooth mobility is classified according to degrees of severity. On two early stages As the symptom develops, the teeth become loosened forward and backward, and the range of movements varies in intensity. At the third stage, the tooth also begins to move laterally, and at the final, fourth stage, it can rotate around its own axis. Unfortunately, the final stage of tooth mobility is a direct indication for their removal. In the first stages of loosening, treatment is possible, but it is lengthy and quite complex.
This can be successfully carried out in our dental clinic of Dr. Granov.
First of all, it is necessary to regularly seek preventive examinations to prevent common tissue diseases oral cavity.
Leave your phone number.
The clinic administrator will call you back.
Make an appointment
Initial consultation with a dentist
For free!
Causes of loose teeth
There are many reasons for pathological tooth mobility, and you should find out the catalysts for the disorder in your case by contacting a specialist. At Dr. Granov’s dental clinic you will be provided with timely, competent assistance in the diagnosis, treatment and prevention of diseases of the teeth and periodontal tissues.
Teeth begin to move for the following reasons:
- The presence of inflammatory processes in the internal structures of the periodontium;
- Atrophic processes in the alveolar processes of teeth;
- Endocrine disorders And hormonal imbalance in the body;
- Incorrect bite or incorrect position some teeth in rows;
- Shortening of the frenulum of the tongue;
- Pathological structure of the tissues of the dentofacial apparatus;
- Untimely or incorrect fixation of dentures (including bridges) or implants after the loss of some teeth;
- Mechanical injuries teeth and jaws (including fractures);
- Medical errors, committed by incompetent or unscrupulous dentists in the process of treating certain diseases of the oral cavity;
- Poor oral hygiene, against the background of which pathologies of teeth and soft tissues develop.
If one or more teeth are loose, you should seek professional help as a matter of urgency.
What to do if loosening occurs?
If you notice that your teeth are loose, sign up for an appointment as a matter of urgency. The specialists at Dr. Granov’s clinic are ready to help you at any time. We urge you not to ignore your symptom, since subsequently the treatment of the provoking pathology can become very complicated.
While you are at home, try to follow three basic rules:
- Never loosen the tooth with your fingers or tongue. Try not to touch it at all, so as not to aggravate the current situation;
- Rinse your mouth warm water(can be soft saline solution), but do not brush your teeth with a brush and toothpaste;
- If a tooth falls out, see a doctor immediately. If this has just happened, you still have the option of emergency implantation. The more you delay the process, the less opportunities there will be for high-quality restoration.
When a tooth falls out, we must not forget that parts of it may still remain inside the gums. And this can also turn out to be very dangerous consequences if you continue to ignore warning signs.
How can we help you?
Find out from a specialist exactly how you should care for your teeth at home, and how to correctly use products designed for your problems and risks.
Refer to the procedure in a timely manner to detect current violations and maintain dental health. In the case, our specialists will select the optimal orthodontic therapy for you. It can consist of both conservative and surgical methods corrections.
If the cause of mobility in your case is, our specialists will select the latest comprehensive treatment for you. It may also include medications and surgical methods. For high-quality prevention of complications, you will need to follow all instructions and recommendations of a specialist. Sometimes an acceptable solution for loose teeth is splinting them. But this option is not effective in all cases, and then the treating specialist decides to use other methods of treatment. If a tooth is lost, it is indicated or. Our specialists perform all types of similar services:
- Implantation;
- Restoration of one or more teeth, as well as complete restoration dentition.
Tooth mobility of the fourth degree requires them surgical removal. The decision on the subsequent installation of prostheses or implants is made on an individual basis, taking into account the characteristics of each case.
If you notice even weak mobility of a molar tooth, contact our dental clinic Doctor Granov. We will provide you with the most effective and timely assistance in eliminating your problem and give valuable advice regarding the subsequent prevention of oral diseases.
Continuing the calculations given in the previous article, we note that 1/4 of 0.2 mm will be 0.05 mm, which will correspond to physiological tooth mobility, measured in the cervical region. The middle of the surface of the tooth crown is located approximately 2 times further from the cervical part of the tooth from the center of rotation of the root (this does not mean the enamel-dentin border, but the section of the tooth root included in the tooth socket), therefore, the amplitude of movements in this area will be 2 times greater : 0.05 x 2 = 0.1, which approximately corresponds to the figures obtained in the experiment.
Deviations may be associated with varying crown, root, and number of roots of the tooth in question. Thus, tooth mobility, measured in the area of the middle of the coronal part of the tooth and equal to approximately 1/4 of the width of the periodontal sheath, corresponds to the physiological mobility of the tooth. Tooth mobility, measured in the area of the middle of the coronal part of the tooth and amounting to more than 0.1 mm, does not correspond to physiological mobility and indicates changes in the periodontium of the tooth.
If increased tooth mobility exceeds the boundaries of the periodontal sheath, this indicates changes in the bone wall of the tooth socket. Within certain limits, these changes can be reversible, which is radiographically confirmed by regression of the expansion of the periodontal sheath. Exceeding these limits indicates the irreversibility of changes in the bone wall of the tooth socket. Experimentally, this limit was set at 0.25 mm of mobility of the crown of the tooth.
Presented analysis was the basis for the ARPA classification of dental mobility, according to which there are various degrees mobility of teeth.
IN periodontics Miller's definition of tooth mobility is more often used. This classification provides for the allocation the following degrees mobility of teeth.
Grade I - mobility up to 1 mm in the horizontal direction.
Grade II - mobility more than 1 mm in the horizontal direction.
Degree III - significant mobility in horizontal and vertical directions.
When comparing these two classifications it's clear that we're talking about about different scales of mobility measurement. The Miller classification allows you to track the dynamics of treatment of acute inflammatory processes or chronic ones that are in the acute stage. ARPA classification is more suitable for defect evaluation supporting apparatus tooth after achieving remission of a chronic inflammatory process or healing of acute inflammation.
In general, from the standpoint of medicine based on evidence, the symptom of tooth mobility should be characterized as a test with high sensitivity and low specificity, since it indicates not only the presence of an inflammatory process in the periodontium, but may also be associated with various physiological conditions body. Thus, tooth mobility can increase during pregnancy, with Cushing's syndrome, and with scleroderma. Increased mobility It is also observed with partial loss of supporting periodontal tissues, even if they do not show signs of inflammation.
In this regard, the assessment degree of tooth mobility in itself cannot be used as a basis for determining the indications and choosing a tire design.
During a certain period To determine the indications for splinting teeth, a criterion such as the amount of destruction of the wall of the tooth socket was widely used. This principle is based on the doctrine of the reserve forces of periodontium by V. Yu. Kurlyandsky. According to this doctrine, intact periodontium is able to withstand double load. When the socket is atrophied by 1/2, the reserve forces are exhausted: the periodontium is still able to perform its function, but, as they say, at the limit of its capabilities.
The greatest danger is presented in such situation horizontal forces, which removable tires can successfully resist. When atrophy reaches 3/4 of the original height of the socket, functional insufficiency of the periodontium occurs, which is unable to withstand both horizontal and vertical loads.
IN similar situation clasp fixation of removable dentures(based on the technical capabilities of domestic dentistry at that time, the maximum that could be counted on in a relatively wide dental practice, - these are clasp splinting prostheses) could not hold the splinted tooth in the vertical direction, therefore, the optimal design of the splint was considered non-removable design. Accordingly, with destruction of 1/4 of the original height of the tooth socket, the periodontium still has a certain reserve of reserve forces, and therefore splinting may not be indicated.
The basis of such views was the idea that initially periodontal disease begins with dystrophy of the supporting tissues of the periodontium, and inflammation joins later when the compensatory capabilities of the periodontium are exhausted. With this approach, the expansion of indications for splinting is inevitable, since any clinical signs indicate rapid decompensation of the inflammatory-dystrophic process.
However, at present, when the role of microbial plaque is rated very highly, splinting without sufficient grounds will not only be useless, but also potentially dangerous, since the splint often contributes to the accumulation of microbial plaque and makes it difficult to carry out hygienic measures in the oral cavity.
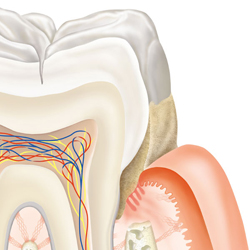
Periodontitis is an inflammatory process of autoinfectious origin, occurring in periodontal tissues, accompanied by progressive destruction of bone and periodontal tissues, often with the formation of periodontal pockets.
1 - healthy periodontium, 2 - periodontal disease
Etiology and pathogenesis of periodontitis
The etiology and pathogenesis of periodontitis is a very extensive amount of information, since the development of pathologies of periodontal tissues is influenced both directly and indirectly by a huge number of factors. All of them are conventionally divided into: local and general.
Local causes and factors contributing to the development of periodontitis
Dental plaque, dental plaque, tartar
The last few decades, namely the research conducted during this time, increasingly confirm the theory that the oral cavity is a separate, independent and definitely balanced biological system, and periodontal diseases are considered in in this context as an imbalance in the balance between oral tissues and bacterial symbiosis. Based on the aspects of this theory, the causes of periodontal disease are considered to be:
- The presence and condition of dental plaque and plaque, as well as metabolic products in them
- Specific factors of oral tissues that can, to one degree or another, influence the pathogenetic capabilities of microorganisms and their metabolic products
- General factors of the body involved in the regulation of metabolism in the tissues of the oral cavity, in particular, those responsible for the response of tissues to pathogenic influences

Four main formations in the oral cavity are considered to be particularly important for the study of periodontal diseases.
- The first two are non-mineralized: dental plaque and soft plaque
- The second two are mineralized, namely: supragingival and subgingival tartar
In this case, the first (dental plaque) gradually turns into tartar through mineralization, where gingival fluid and saliva are sources of minerals (phosphorus, calcium, carbonates, magnesium and other microelements).
Thus, dental plaque, as it grows, moves into the subgingival margin, causing irritation of the gum tissue.
This happens due to toxins released by microorganisms living in this dental plaque. Further development of the process, as a rule, leads to inflammation of the adjacent tissues and damage to the epithelium lining the gum pocket, that is, to a condition called periodontitis.
The role of exotoxins and endotoxins secreted by microorganisms on the development of periodontitis
But it is worth noting that not all microorganisms are capable of causing a similar effect. As you know, all bacteria are divided into two types: gram-positive and gram-negative. In this case, gram-positive bacteria are permanent inhabitants of the oral cavity, and their metabolic products, exotoxins, do not have a pathogenic effect on oral tissues, in particular periodontal tissues.

Others, gram-negative representatives, that is, the toxins they secrete - endotoxins, are extremely resistant to temperature changes, are aggressive towards tissues at the site of bacterial application, and are stimulators of the formation of antibodies. They are capable of disrupting normal cellular metabolism, which is accompanied by hyper- and then hypoglycemia, and often leads to the development of hemorrhagic necrosis, which in general is nothing more than periodontitis.
Composition and properties of saliva
Particular importance in the role of metabolism and the formation of periodontal pathologies is given to saliva and its composition. After all, it is the source of enzymes that primarily break down food, a source of microelements, which means that, to a large extent, its properties can influence the formation of dental plaque and its composition.
Iatrogenic factors
Local factors contributing to the development of periodontitis include iatrogenic, namely local traumatic factors, for example: defects in prosthetics. But in this case, the form of the disease will be acute focal.
Periodontal overload
Also identified is the cause of periodontitis, such as overload of periodontal tissues, malocclusion, early loss of teeth, anomalies in their position. This is due to the fact that when the periodontium is overloaded, a change in trophism occurs - tissue nutrition, which inevitably leads to their change.
Periodontal underload
Insufficient chewing function and underload are also predisposing factors to the development of periodontal pathologies. The lack of load on the periodontium during chewing provokes the onset of the atrophic process in its tissues.
General factors influencing the development of periodontitis
Vitamin deficiency

Root causes common factors Deficiency of vitamins C, B1, A, and E is considered to influence the development of periodontal diseases. Vitamin C is especially distinguished. Since its deficiency significantly affects the condition of collagen fibers, which in turn are part of periodontal tissues.
Vitamin A contributes to the normal process of epithelialization of the gums, vitamins B 1, E, participate in metabolism, regenerative processes, play important role in maintaining overall tissue stability.
Vascular atherosclerosis
Vascular atherosclerosis is often the cause of the development of periodontitis, as it causes osteodystrophy, which leads to recession - a decrease in the alveolar processes of the jaws, the formation of periodontal pockets, immersion of the epithelium in them, and destruction of the circular ligament of the tooth. This condition becomes an excellent breeding ground for even more active proliferation of bacteria, and often leads to the development of purulent-inflammatory processes.
Body reactivity
Reduced reactivity of the body, that is, general decline protective immune forces of the body, is not the cause of the development of periodontitis, but is a factor predisposing to it, since when pathogenic effects endotoxins, the body is not able to provide sufficient resistance to them.
Endocrinology in periodontology
Risk factors also include endocrine disorders, especially dysfunction of the reproductive, parathyroid, and thyroid gland. There is also a tendency to periodontitis in people with diabetes. In the latter case, the picture of periodontitis is chronic and generalized in varying degrees of severity.
Gastrointestinal diseases
Gastrointestinal diseases (gastrointestinal intestinal tract), especially peptic ulcer stomach and duodenum, promotes the accumulation of histamine in the blood serum, the effect of which on blood vessels often leads to changes in the periodontium.

Diseases of the gastrointestinal tract
Blood pathologies
Diseases of the blood and hematopoietic system, such as anemia, leukemia, disorders of the coagulation and fibrinolytic systems, neutropenia, lead to dystrophic changes in the periodontium, hyperplasia of the gingival margin, resorption and osteoporosis of bone tissue.
Psychosomatics
Psychosomatic factors. Taking medications sedatives, neuroleptics, tranquilizers leading to xerotomy; hyperkinesia (bruxism) masticatory muscles under stress, it often becomes a factor contributing to the development of periodontitis.
Classification of periodontitis
Downstream:
- acute
- chronic
- aggravated (abscess)
- remission
According to the prevalence of the process:
- localized (focal)
- generalized (diffuse)
By severity:
- easy
- medium degree
- heavy
Characteristics of periodontitis of varying severity
Lightweight
Periodontitis first mild degree severity is characterized by a loss of alveolar bone to 1/3 of the height of the tooth root, the bottom of the periodontal pocket during examination is reached at a depth of up to 3.5 mm, while the teeth are motionless.
Average
The second degree - moderate - is characterized by the presence of a periodontal pocket, the depth of which reaches 5 mm, and the loss of alveolar bone is 1/2 of the height of the root, while pathological mobility of teeth of 1-2 degrees is observed.
Heavy
The third degree, severe, is characterized by a depth of periodontal pockets of more than 5 mm, with a concomitant loss of alveolar bone by more than 1/2 of the root height, and 3-4 degrees of tooth mobility are detected.
- The 1st degree of mobility is diagnosed when the ability of a tooth to move, in relation to the neighboring one, in the palatal - buccal-lingual, vestibulo-oral directions, by no more than 1 mm.
- The 2nd degree is determined by pathological mobility of more than 1 mm in the same directions, with the addition of mobility in the palatal-distal direction.
- The 3rd degree is considered to be mobility of the tooth in all directions, including vertical; in the absence of adjacent teeth, it may be tilted.
- The 4th degree is pathological mobility of the tooth, in which it can make forced movements even around its axis.
Forms and types of periodontitis
Focal periodontitis
Focal periodontitis is a form of inflammatory process located locally, that is, separately in a certain area of the periodontium, in the area of one, two or several teeth, subject to complete or relative health of the remaining periodontal tissues. Most often, it is caused by local trauma, for example: an inflated filling, or an overhanging one, or rubbing of an incorrectly installed crown or bridge. Most often, localized periodontitis manifests itself in acute form, that is, it begins sharply, unexpectedly, suddenly, with rapidly increasing clinical symptoms.
Generalized periodontitis, otherwise called diffuse, is characterized by pathological changes in periodontal tissues in the area of almost all or all teeth in the dentition. Most often wears chronic form, has a bacterial etiology, the onset of the disease is usually asymptomatic and painless.

Acute periodontitis
Acute periodontitis is an inflammatory process in the periodontal tissues of the oral cavity, characterized by the sudden appearance of pain, swelling, bleeding, and often the appearance of purulent exudate or bloody discharge from the gum pocket.
Chronic periodontitis is a form of inflammatory process occurring in periodontal tissues, of a cyclical nature (alternation of relapses - exacerbations and remissions - attenuation).

Chronic generalized periodontitis
Chronic generalized periodontitis is a form of the disease that has diffuse damage to periodontal tissues. Characterized by alternating remissions and relapses.
Purulent periodontitis
Purulent periodontitis - pathological condition periodontal disease, in which purulent exudate. Advanced purulent periodontitis can cause the development of an abscess.
Abscessing periodontitis
Abscessing periodontitis is a complicated form of periodontitis, characterized by the development of a purulent focus - an abscess.
Aggressive forms of periodontitis
Aggressive forms of periodontitis are forms of periodontitis with an atypical course, caused by microorganisms that are able to penetrate faster and more strongly into periodontal tissues and have the most pronounced pathogenic properties.
Classification of aggressive forms of periodontitis
- Chronic periodontitis in adults
- Early-onset periodontitis (EAP)
- Prepubertal periodontitis
- Juvenile periodontitis (periodontal disease)
- Rapidly progressive periodontitis
- Type A.
- Type B.
- Refractory periodontitis
- Periodontitis associated with systemic diseases
Adult periodontitis
The name of this subtype speaks for itself. Adult periodontitis is a pathological, slowly developing form of periodontitis that affects people over 35 years of age. Most often, bone loss in such patients occurs horizontally, but vertical - angular loss - cannot be ruled out.
Characteristic feature of this disease is its etiology, namely the provocation of its development by gram-negative bacteria.

When examining patients with this form of the disease, pathologically altered blood cells are not detected. In the variety of periodontal diseases, it is this disease is the most common among the adult population.
Prepubertal periodontitis
Prepubertal periodontitis is considered to be periodontitis that occurs after eruption permanent teeth. On my own this form The disease is quite rare, but its prevalence still makes it possible to distinguish two forms: localized and generalized.

A small number of adolescents experience LUP - localized juvenile periodontitis. As a rule, the onset of pathology development occurs during puberty. The classic development of the disease is vertical bone loss in the first molars, often in this process the incisors are also involved. It is noteworthy that severe bone loss can develop almost asymptomatically.
Plaque is not detected in significant quantities. There are no symptoms of the inflammatory process, or they are very scarce.
Some periodontists support the theory of family predisposition, since with this disease neutrophils or monocytes that are functionally incomplete are found in the blood, but both types of cells cannot have defects in this pathology.
There is also a 3-fold increased incidence of LUP in females.
Sometimes the reason of this state may become one of the forms of nonspecific anaerobic bacteria, related to gram-negative. This is confirmed by the positive dynamics in the treatment of LUP with antibiotics in the composition complex therapy.
Among other things, for juvenile periodontitis, a generalized form is not uncommon, when the entire dentition is involved in the pathological process.
This form of periodontitis is typical for people who have left the puberty, and under 35 years of age. It is characterized by severe loss of alveolar bone, in a generalized form around most teeth. In this case, bone loss can occur both vertically and horizontally, as well as in their complex.

This disease is also characterized by a discrepancy between the amount of plaque and the degree of destructive changes in the bone. Some cases of the development of rapidly progressive periodontitis can be associated with the presence of such systemic diseases, How diabetes mellitus, or Down syndrome, but they are often found in individuals who do not have such systemic pathologies.
Rapidly progressive periodontitis is further subdivided within its form into two types, both of which are characterized by rapid, generalized loss of bone and attachment, and are divided according to age category patients. Namely:
- Type A includes periodontitis that develops in patients aged 14-26 years
- Type B includes rapidly progressive periodontitis affecting the periodontium in patients aged 26 to 35 years.
Regardless of the type, the disease often recurs, despite the success and quality of the therapy.
Refractory periodontitis

Refractory periodontitis is a special type of periodontitis, which, despite constant therapeutic measures, continues to develop, which is accompanied by loss of bone tissue in several areas simultaneously.
Most often, this disease is a consequence of untreated acute necrotizing ulcerative gingivitis, especially long-term and recurrent forms, as well as when they are insufficiently treated. Episodically repeated activity of the pathology leads to the destruction of periodontal tissue, and as a consequence to the formation of both interdental and gingival craters. Also, the cyclical nature of the disease negatively affects the possibility of adequate care and treatment.
Conclusion
Periodontitis, the classification of which is described above, is actually not such a harmless disease. Despite its apparent frivolity, progressive and aggressive forms can lead to irreversible consequences, including tooth loss. The pathogenesis of periodontitis is extensive, which means that almost every person can suffer from this pathology. To protect yourself and your loved ones from this disease, you need to contact your dentist in a timely manner and undergo regular preventive examination, and, of course, know the symptoms of periodontitis.
Related materials
Periodontal diseases- this is a large group of periodontal lesions that vary in etiology and pathogenesis, mainly based on the principle of localization of the process and the similarity of symptoms or syndromes.
Research methods:
Radiologist
Targeted orthopantomography
Panoramic radiography
Diagnosis of gum inflammation:
Schiller-Pisarev
Determination of the resistance of gum capillaries
Thermometry
Rheoparodontography
Polarography
Capillaroscopy
Determination of the degree of mobility:
3 degrees of mobility
Determination of periodontal pocket depth:
With probe
X-ray contrast wedge
Occludiograms:
Normal
Frontal
Mixed
Distal
Determination of pulp electrical excitability
Determination of the electrical potential of a pathological gingival pocket.
The significance of periodontal disease as a general medical problem is explained by:
1) significant prevalence.
2) loss of a large number of teeth.
3) the appearance of lesions chronic infection in connection with the formation of gingival and periodontal pockets and their role in reducing the reactivity of the body.
Functional traumatic overload of the periodontium
Occupies a special place among local reasons in the etiology and pathogenesis of periodontal diseases. When chewing and swallowing, at the moment of closure of the dentition, the periodontium of each tooth perceives a force load, which, when normal conditions depreciated special devices periodontal (cemento-alveolar, interdental fibers, etc.). Then it is transformed and transmitted to bone structures jaws, temporomandibular joint and skull. Such physiological load contributes to the normalization of trophism and metabolism, stimulates the processes of growth and development.
At pathological processes in the periodontium, caused by common reasons(vitaminosis, diabetes and other disorders endocrine regulation, diseases of the gastrointestinal tract, cardiovascular system and nervous systems etc.), the resistance of periodontal tissues decreases.

As a result of weakening of the periodontium, the usual occlusal load begins to exceed the tolerance of its structures and turns from a factor stimulating development into a traumatic one, disrupting the trophism of the periodontium and destroying its tissues. Traumatic occlusion occurs, which subsequently plays a leading role in the course of this disease.
The term “traumatic occlusion” was proposed by P. R. Stillman in 1919. Other terms have been proposed to characterize and define periodontal overload:
- “traumatic articulation”
- “functional traumatism”
- “pathological occlusion”
- “functional traumatic overload of teeth”, etc.
According to the mechanism of development, three types of traumatic occlusion are distinguished:
Primary
Secondary
Combined
Primary traumatic occlusion develops against the background of unaffected periodontium as a result of the action of an occlusal load that is excessive in magnitude and/or direction.
Thus, primary traumatic overload of healthy periodontal tissue can occur due to excessive magnitude, abnormal direction and duration of action of the occlusal functional load and steam function of the masticatory, facial muscles and tongue. More often than not, overload is caused by the simultaneous action of several causes.
Secondary traumatic occlusion:
Its pathogenesis is based on pathological changes periodontal tissues. At the same time, degenerative and inflammatory processes which are accompanied by:
1). resorption of bone tissue of the alveolar process.
2). Gingivitis.
3). destruction of the periodontium with the formation of a pocket.
4). suppuration from it.
Resorption of the bone tissue of the sockets leads to a disruption of the normal biological patterns of the structure and function of the periodontium. From this moment on, a radical change occurs in the biomechanical relationship between teeth and surrounding tissues.


Thus, a change in the ratio between the outside and inside the alveolar part of the tooth is one of pathogenetic mechanisms in the development of traumatic occlusion.
The clinical picture of secondary traumatic occlusion is diverse and depends on the age of the patient, the form of the underlying disease (periodontal disease, periodontitis), its severity and stage of development, the presence of dentition defects, malocclusion or tooth position, pathological abrasion and other traumatic factors.
If for primary traumatic occlusion orthopedic intervention is sufficient, then for secondary occlusion complex therapeutic (local and general), surgical and orthopedic treatment is required. The prognosis also varies. In case of primary traumatic occlusion, after eliminating the overload of the teeth in all periodontal tissues, reparative processes occur.
Pathological tooth mobility syndrome
Pathological mobility of teeth is one of the symptoms of periodontal disease. The symptom of tooth mobility sometimes becomes prevalent over other signs (gingivitis, bleeding, osteopathy, periodontal pockets, destruction or atrophy of the bone tissue of the alveolar process, cementopathy) (decalcification, pigmentation, root caries), or these symptoms are summed up, which creates even greater difficulties in achieving positive effect of complex treatment.
The degree of tooth mobility is an objective indicator of the depth of damage to periodontal tissues.
There are three degrees of pathological tooth mobility:
I. Degree – tooth mobility in the vestibular-lingual direction;
II. Degree – tooth mobility in the vestibular-lingual and mediadistal directions;
III. Degree – tooth mobility in all directions.
Classification of tooth mobility byMiller
1st degree – slight mobility
2nd degree – horizontal deviation up to 1 mm
3rd degree – tooth mobility in all directions
Today, the dominant assessment scheme in clinical periodontology is the tooth mobility index. According to her normal tooth has a physiological minimum deviation, which is designated as zero degree of mobility.
Pathological mobility can be of three degrees:
Tooth deviation to the sides is up to 1 mm.
Tooth deviation to the sides is within 1-2mm.
Lateral deviation of the tooth is more than 2 mm and vertical mobility.
Orthopedic methods in the complex treatment of periodontal diseases are aimed at:
1) Restoring the lost unity of the dental system and transforming teeth from separately acting elements into a single whole.
2) Redistribution of the functional load over the entire dentition with unloading of teeth with the most weakened periodontium.
3) Protecting teeth from the most dangerous horizontal load for periodontium.
4) In case of defects in the dentition - their replacement with an appropriate prosthesis.
Selective grinding of teeth
One of the most common methods in the complex therapy of periodontal diseases. According to some data, 95.8% of patients with periodontal pathology need it.
Objectives of selective teeth grinding:
1. Elimination of premature occlusal contacts
2. Elimination of moments that block and interfere with the movements of the lower jaw
3. Elimination of deformation of the occlusal surface of the dentition.
There are different ways grinding teeth, the most popular methods are Jenkelson and Schuller.
The technique proposed by Jankelson (1979) is considered functional method, however, premature contacts are removed in central occlusion.
According to Jenkelson's classification, premature contacts are divided into 3 classes:
1st contacts on the vestibular slopes of the buccal cusps of molars and premolars and the vestibular surface of the lower incisors
2nd contacts on the oral slopes of the palatine tuberosities upper molars and premolars;
3rd contacts on the vestibular slopes of the palatal cusps of the upper molars and premolars.
Indications for selective grinding:
The presence of premature contacts of antagonist teeth in central, anterior and lateral occlusions;
Absence or uneven wear of hard dental tissues;
Deformations of occlusal surfaces;
Malocclusions
Method of selective grinding of teeth:
It is carried out before therapeutic and surgical procedures or in parallel with them.
- Preliminary grinding of teeth involves shortening protruding teeth and is intended to eliminate significant deformations of the occlusal surfaces that occur due to defects in the dentition. If significant shortening is necessary, depulpation of the latter is indicated.
- The final sanding is carried out in a certain sequence. First, premature contacts are eliminated in various types occlusion, then - when moving the lower jaw from central to anterior and lateral occlusions.
- Before grinding, an occludogram is obtained, which is stored to monitor the results of grinding. After carrying out this manipulation, it is necessary to polish the ground surfaces and coat them with fluorine varnish.
Orthodontic preparation for orthopedic treatment for periodontal diseases
In patients with periodontal pathology clinical picture is often complicated by deformations of the dentition; in addition, malocclusions in some cases can themselves lead to periodontal pathology, so orthodontic preparation before orthopedic treatment is of great importance.
Structurally, orthodontic appliances have some differences from classical ones, these include:
Use minimal force to move teeth.
Longer active treatment and retention period.
Temporary splints can be used as retention devices.
Splinting
Connecting individual teeth into a single block to limit their mobility and redistribute the functional load. In acute cases, high-quality production of a splint is difficult and it is necessary to stop the acute inflammatory process.
There are temporary and permanent splinting. Both temporary and permanent splints must meet the following requirements:
Create a strong block from a group of teeth, limiting their mobility in three perpendicular directions;
Be rigid and firmly fixed to the teeth;
Do not irritate the marginal periodontium;
Do not interfere with therapeutic and surgical procedures;
Do not have retention points for food retention;
Do not increase height lower section face and not create premature contacts on its surface;
Don't call gross violations aesthetics and speech of the patient;
The production of a splint, if possible, should not be associated with tooth preparation.
Indications for temporary splinting:
Consolidation of the results of therapeutic and surgical treatment.
It is difficult to predict the condition of individual teeth or their groups immediately after conservative and surgical procedures.
Tooth extraction (during the healing period of the hole)
Permanent splinting:
Permanent splints are divided into non-removable and removable.
When choosing a tire design, consider:
1). form of damage (generalized or localized process).
2). periodontal condition and degree of mobility of splinted teeth.
3). condition of antagonist teeth.
4). presence and topography of dental defects.
5). degree and uniformity of resorption of the alveolar process.
Comparative characteristics of removable and non-removable tires
Removable:
1. Limit mobility only in the horizontal plane
2. Does not injure the marginal periodontium
3. Do not interfere with ter. And hir. Treatment
4. Do not violate oral hygiene
5.Minimal need for preparation
Fixed
1. Limit mobility in three planes;
2. May cause periodontal trauma;
3. May interfere with ter. And hir. Treatment;
4. Violate oral hygiene;
5. There is often a need for significant tooth preparation
Removable splints are indicated for:
a) Generalized periodontal disease with uniform resorption of the alveolar process of no more than 1/2 of the root length;
b)B initial stages diseases to eliminate or reduce horizontal overload;
c)As preventive devices;
d) For indications for the manufacture of removable dentures.
Fixed tires are indicated for:
a) Uneven resorption of the alveolar process of more than ½ of the root length;
b) Localized process;
c) The presence of teeth with different degrees mobility;
d) Elimination of overload in the vertical direction.
Modern reinforcements for splinting are divided into two large groups based on fiber composition:
1.materials based on inorganic matrix - ceramic and fiberglass:
- "Glasspan"(Glasspan)
- "FiberSplint"(Polydentia)
- “Fiberkore”(Splint it. Jenerik/Pentron)
2. Materials based on an organic matrix - polyethylene:
- "Ribbond"
- “Connect”(Kerr)
- “DVA” (Dental ventures of America).
The reinforcements consist of many very fine fibers, 3-5 microns in diameter, intertwined with each other. The special strength of the reinforcement is obtained by impregnation with resin and flowable composites.
3.metal based materials:
SPLINTMATFINE (PULPODENT,USA)
SPLINTLOCK (COLTENE|WHALEDENT,Switzerland)

Types of adhesive splints:
By service life:
Temporary (3-4 weeks);
Long-term (up to 10 years);
According to the method of fiber impregnation:
Pre-filled (impregnation is carried out at the factory) Fiber, Kor, Vektris
Fillable (impregnated before use) Glasspan, Connekt, Ribbond
According to the technique of preparing abutment teeth:
Non-invasive (on-coronal)
Invasive (intracoronal)
By manufacturing method:
Direct method (intraoral)
Indirect method (laboratory)
Requirements for splinting structures:
Rigidity and ensuring reliable immobilization of mobile teeth.
Elimination of periodontal overload.
Elimination of additional irritation by splints of marginal periodontium.
Creation of optimal conditions for therapeutic and surgical treatment.
Aesthetics.
Atraumatic in production (small volume of preparation of abutment teeth.
Hygiene.
Biocompatibility with surrounding tissues.
The splinting effect of removable splints is ensured by a system of support-retaining clasps and occlusal pads connected into a single splint. The production of such a tire is possible only by casting on fire-resistant models.
Direct prosthetics
The denture is made before teeth are removed and is applied immediately after surgery. Lamellar prostheses are more often used as immediate prostheses.
In addition to preventing functional overload, immediate prostheses serve as a protective bandage and a shaping apparatus.
Errors and complications during orthopedic periodontal treatment
1). Errors in choosing a tire design;
2). Errors that occur during the treatment stages.
Protocols for the provision of dental care (prosthetic dentistry):
MKH-10 K 05.30 Periodontitis of localizations (hostria)
MKH-10 K 05.30 Localized periodontitis (chronic)
MKH-10 K 05.30 Periodontitis of localizations (restricted)





