Chapter6 Non-carious lesions of teeth
In our country, a number of classifications of non-carious lesions of teeth are known (V.K. Patrikeev; Yu.A. Fedorov, etc.).
In the International Classification of Diseases (ICD X revision, WHO), non-carious dental lesions are presented in the following forms:
K.00.3. Mottled teeth (endemic /fluorous/ mottled enamel /dental fluorosis/; non-endemic mottled enamel /non-fluorotic opacification of the enamel/; unspecified);
Why is tooth enamel destroyed?
Abrasion is defined as the physiological wear and tear of a tooth surface or repair caused by the contact of one tooth with another during the chewing process or function, which can occur in both the primary and permanent dentition. Erosion has been described as a progressive, pathological loss of tooth structure caused by a chemical process without involvement bacterial action. Typically, erosion is caused by exposure to acids in beverages, fruit juices, wines, sports drinks, all soft drinks, vinegar, organic acids, mainly lactic acid, citric and apple whey, used in food industry, and can be represented by clinical photographs, Salivation may be suppressed by hypolysis or excess acid.
K.00.4. Disorders of tooth formation (prenatal, neonatal enamel hypoplasia; aplasia and hypoplasia of cement; dilaceration /enamel crack/, odontodysplasia; Turner tooth; other specified; unspecified);
A 50.512. Hutchinson incisors;
A 50.52. Mulberry-shaped molars;
K.00.5. Hereditary disorders of the tooth structure, not classified elsewhere (incomplete amelogenesis, dentinogenesis, odontogenesis, dentin dysplasia, shell teeth; unspecified);
II. Damage to hard dental tissues
Hypofunction should be investigated salivary gland such as bulimia, diabetes, drug use, voluntary or involuntary regurgitation, heartburn, hernia hiatus. Erosion from dental exposure to gastric secretions is called perimolysis. Abfraction may affect only one tooth and clinically present a wedge-shaped, usually deep and defined edge. This type of lesion has more high level V lower teeth due to its smaller diameter coronary artery in the area of the cervix.
K.00.8. Other dental development disorders (discoloration during formation due to blood type incompatibility, birth defect biliary system, use of tetracycline; other specified disorders of dental development);
K.03. Other diseases of dental hard tissues:
K.03.0. Increased abrasion (wear) of teeth (occlusal, contact surfaces; other specified; unspecified);
Lesions after eruption
Abfraction is an example of a non-carious lesion that affects the cervical region and is not due solely and exclusively to acid dissolution and the mechanical action of abrasive agents. This phenomenon can be exacerbated by abrasion caused by aggressive cleaning, where once damaged enamel can be more easily removed by erosion or abrasion. Etiological factors of non-carious lesions.
The etiology of non-carious lesions can be multifactorial external factors, internal factors, dental mechanical wear resulting from the association of traumatic brushing associated with abrasive dentifrices and consumption of acidic substances, use of legal or illicit drugs, and mechanical processes resulting from bad habits, such as frequent use abrasives, teeth whitening without professional supervision, habits of putting pencils between teeth, toothpicks, pipe linings, hair clips, nail biting, cutting lines, improper use of toothbrushes and dental floss.
K.03.1. Grinding (abrasive wear) of teeth (caused by tooth powder - wedge-shaped defect, habitual, professional, traditional /ritual/; other specified; unspecified);
K.03.2. Dental erosion (occupational, caused by: persistent regurgitation or vomiting; diet; medications; idiopathic; other specified; unspecified)
Treatment and prevention of non-carious diseases
A pH of up to about 5 is sufficient to weaken and demineralize the enamel surface, while for dentin a pH of 5 or less has the same effect. harmful effect, depending on other factors such as the titrated acidity and the calcium, phosphate and fluoride content of the foods consumed.
Classification of non-carious enamel lesions
Recent decades have seen a significant increase in acid consumption in beverages such as soft drinks and fruit juices. It is necessary to warn that these substances are offered earlier when breastfeeding through their use in bottles. The process of weakening of teeth due to acid is usually attenuated by the action of saliva due to the presence of calcium, but frequent and prolonged contact with acidic substances leaves little time for remineralization. In this weakened state, the enamel is susceptible to wear and tear from the abrasive effects of toothpastes and toothbrushes.
K.03.3. Pathological resorption of teeth (external / disturbed /; internal / pink spot/; unspecified);
K.03.6. Deposits on teeth (pigmented plaque - black, green, orange; caused by the habit of using tobacco, chewing betel; white soft deposits; supragingival and subgingival tartar, dental plaque; other specified; unspecified);
A decrease in the pH of fluids that bathe teeth can be caused directly by consumption of acidic fruits and drinks or indirectly by ingestion of fermentable carbohydrates that allow plaque bacteria to produce acid. With a decrease in pH, the solubility of enamel apatite increases sharply. Simple calculations show that a drop in pH unit in the pH range from seven to four leads to a sevenfold increase in the solubility of hydroxyapatite.
The solubility of apatites depends on pH because: the hydroxyl concentration is inversely proportional to the hydrogen concentration, and the concentration of ionic phosphate complexes depends on the pH of the solution. When saliva is unsaturated, hydroxyapatite may still be a supersaturated fluorapatite. At pH = 4, saliva is unsaturated from both apatites and, therefore, loses its mineralizing ability. We can conclude that the pH value is one of the most important factors to consider in a liquid diet.
K.03.7. Changes in the color of the hard tissues of teeth after eruption (due to the presence of metals and metal compounds, bleeding of the pulp, the habit of chewing betel nut, tobacco; other specified; unspecified);
K.03.8. Other specified diseases of dental hard tissues (sensitive dentin, enamel changes caused by radiation; other specified). Taking into account this classification and domestic clinical classifications, the following division of non-carious lesions of teeth is accepted:
Other factors to consider are the type of acid and the degree of ionic dissociation of the acid. Of the characteristic factors, the most common cause of erosion is gastroesophageal reflux and regurgitation and affects more than 60% of people at some point in their lives.
Abuse of topical substances such as vital whitening products important teeth without professional supervision, medications for further use of vitamins and illicit drugs may be associated with abnormal tooth wear. Several drugs are responsible for hypolyzing and just to give one example, chewable tablets vitamin C have low level pH. The use of cocaine paste in the cervical third of the anterior teeth and the use of methamphetamine and lysergic acid should also be investigated.
I. Hereditary and congenital lesions of hard dental tissues:
1) anomalies in the size and shape of teeth (fused, spiky teeth, macrodentia, microdentia, invagination of teeth, enamel drop);
2) mottled teeth - endemic mottled enamel (fluorosis);
3) disorders of tooth formation - enamel hypoplasia (prenatal hypoplasia, neonatal hypoplasia, Turner's teeth, Hutchinson's teeth, mulberry-shaped molars, as a result of congenital syphilis);
How can you use a toothbrush and toothpaste to influence the process of non-carious lesions? According to some researchers, cleaning technique is not important for the occurrence of abrasive damage. A laboratory study stated that it would take 500 years to remove 1mm of enamel using a toothbrush alone, and it would take 100 years to remove 1mm of enamel using a combination of toothpaste and brush. The combination of cellulose with acids produced in the same amount will lead to wear after 2 years.
Abrasion wear in addition to exposure to a diet rich in food products with an acidic pH may be related to the method, strength and frequency of brushing, the hardness of the brush threads and the shape of the filament ends. Trauma to the brush may not cause direct gingival retraction, but may wear down the tooth and the Amelo-Cement junction, resulting in decreased cementation, decreased epithelial adhesion, and alveolar bone loss, and alveolar bone loss results in more gingival reintegration, in addition to what has been found to be that abrasion is significantly greater with linear cleaning compared to rotating and increasing its frequency will lead to an increase in the amount of pathological wear.
4) hereditary disorders of the structure of teeth - imperfect enamelo-, dentin- and odontogenesis;
5) other disorders of dental development (discoloration as a result of Rh conflict, malformation of the biliary system, taking tetracycline).
II. Disorders of teething and acquired damage to their hard tissues:
Although soft brushes Less abrasive than hard brushes, they can cause abnormal wear when used with a non-fluoridated acid dentifrice because they retain more toothpaste for longer. By definition, dentifrices contain abrasives for the purpose of removing stains and other deposits from the surface of the tooth. IN different formulas Different abrasives work, and some others. Relative Density Abrasiveness is a numerical scale that indicates the degree of abrasiveness and is useful for comparing different folders.
1) violation of teething;
2) increased abrasion, including as a result of the abrasive action of toothpastes, powders, brushes, bad habits, occupational hazards and folk customs;
3) wedge-shaped defect;
4) erosion;
5) change in color of hard tooth tissues after teething;
6) other damage to the hard tissues of the tooth - changes in the enamel as a result of radioactive radiation; dentin hyperesthesia.
Fluoridated toothpastes provide greater protection against tooth wear, and the interaction between fluoridated toothpastes and twice daily brushing is associated with a 30% reduction in erosion. Could dentin hypersensitivity be directly related to the process of non-carious lesions?
Dentin hypersensitivity is characterized by short-term and acute pain caused by exposure of dentin in response to thermal, evaporative, tactile, osmotic or chemical stimuli and cannot be attributed to any other type of defect or pathology. Evidence obtained from extracted teeth indicates that in hypersensitivity the dentin must be open and the dentinal tubule network open to allow fluid to move against the received stimulation, in fact this is the case.
III. Dental injuries:
tooth dislocation;
fracture of the tooth crown within the enamel, dentin, opening of the pulp;
tooth root fracture.
In childhood, hereditary and congenital non-carious dental lesions mainly occur:
1) enamel hypoplasia;
2) fluorosis;
3) drug-induced and toxic disorders of the development of dental tissues;
Is it possible that toothbrush Using an abrasive toothpaste may or may not initiate dentin hypersensitivity may be supported by some scientific evidence, although mostly from laboratory studies and to a lesser extent from human studies. Many dentifrices appear to immediately remove the dentin layer of dentin to expose the tubules in a relatively short period, equivalent to days of brushing.
It could be said that this discussion shows that all dentifrices are etiological factors in dentin hypersensitivity, but this is not necessarily the case. Some formulas, although they remove a layer of dirt from the dentin, then cause the dentinal tubules to become narrowed, presumably through an abrasive slurry process. Some toothpaste removes a layer of dentin slab, then covers the tubes with inert abrasive particles.
4) hereditary disorders of the development of dental tissues. Non-carious lesions that occur after teething are found much less frequently in children:
1) dental injuries;
2) drug-induced and toxic disorders of the development of dental tissues;
3) increased tooth wear.
Hereditary and congenital lesions of hard dental tissues
Products containing artificial silica with non-ionic detergent appear to be most effective in this pathological process wear: frequent use of sodium lauryl sulfate, anionic detergent, apparently prevents the adhesion of artificial silica to dentin, probably due to ionic competition. It is clear that if dentin is subjected to friction alone or friction combined with erosion, dentin hypersensitivity may occur.
But again, this will mean that wear will open up the tubular system. Opening of the tubules will almost certainly occur and would be consistent with the relatively rare presentation of individuals with dentin hypersensitivity on the occlusal surfaces, indicating a habit of grinding teeth and ingestion of large quantities of fibrous citrus fruits. In this sense, field studies have shown that for some people, drinking one liter of soda per day, which is common in many countries, can lead to the removal of one millimeter of enamel over several years.
Anomalies in the size and shape of teeth are described in section18 " Dental anomalies". This group of hard tissue lesions includes enamel hyperplasia, which manifests itself in the excessive formation of tooth tissue. A synonym for enamel hyperplasia is “enamel drop” or “enamel pearl”. Their origin is associated with the process of differentiation of Hartwig vagina cells into anameloblasts.
In the cervicobuccal region of the teeth this will mean more than the thickness of the enamel at that point. Additionally, as mentioned, the rate of enamel loss will be accelerated by regular brushing. Laboratory research and on-site studies show that after dentin exposure, acidic drinks can remove a layer of dentin dirt, exposing the tubules after drinking the clinical equivalent of small doses of an acidic drink. Occupational exposure and dental erosion.
The first publications devoted to the relationship between professional exposures and manifestations of the Stomatognathal system date back to the beginning of the century. The study of the relationship between exposure to acid mists and dental erosion has dominated odontological research in relation to other potential effects. Reports from the specialized literature indicate that occupational exposure to acidic substances in their various physical forms is important factor risk of developing sexual pathologies, while maintaining consistent results regarding dental erosion.
Enamel drops are more often found in the area of the necks of the teeth, sometimes at the bifurcation of the roots. Their size reaches 2-4 mm in diameter. In the clinic they do not show themselves in any way and are discovered as an unexpected find. Cervical enamel drops are usually found with gingival retraction (see section2) and exposure of the neck of the tooth, the roots can be visible during x-ray examination or after tooth extraction.
Meanwhile, intradental (intradentinal) enamel drops are more common when the doctor, when preparing a carious cavity within the dentin, discovers a more rigid area with a drill.
Only cervical enamel drops are subject to treatment. They need to be ground with a diamond head and this area of the tooth should be polished, and then the patient should be given recommendations for daily applications of phosphate-containing toothpastes for 7-10 days.
Dental fluorosis is an endemic disease caused by fluoride intoxication, resulting from the consumption of drinking water with a high fluoride content during the formation of the dental follicle. One of the early signs of fluorosis is tooth damage. With a significant concentration of fluorine (above 5-10 mg/l), it is also affected bony skeleton humans and animals.
The main source of fluoride is drinking water. The prevalence and intensity of dental fluorosis among the population increases with increasing concentrations of fluoride in water. Thus, with a fluorine content of up to 0.5 mg/l, no changes in dental tissues are observed; at a fluorine concentration of 0.8-1.0 mg/l, mild forms of fluorosis occur in 10-12% of the population; at a concentration of 1.0-1.5 mg/l, fluorosis is observed in 20-30% of the population; with a fluorine content of 1.5-2.5 mg/l - 30-45%; at a fluorine concentration of 2.5-3.0 mg/l - in 80-90% of the population. In areas with hot climates, fluorosis can develop at a fluorine concentration in water of 0.5-0.7 mg/l, which is associated with its increased consumption. The presence of a significant amount of calcium in water reduces the intensity of fluorosis.
Another source of fluoride in the body is food. The fluoride content of foods and beverages depends largely on the concentration in the water used to prepare food and beverages. In food, as well as in water, fluoride is in ionized form. However, food fluoride is less easily absorbed than water-soluble fluoride. Fish (especially cod), parsley, tea, contain large amounts of fluoride. walnuts, liver, beef
Dina, cocoa. The level of fluoride in lamb, veal and oatmeal is quite high.
Another source of fluoride is fluoride-containing toothpastes. Despite the fact that the adsorption of fluoride in the oral cavity is less than 1%, there is evidence of a connection between the frequency of enamel opacities (initial fluorosis) and brushing teeth with fluoride-containing toothpaste in the first two years of life (Sakharova E.B., 2001, etc.).
The exact mechanism of fluorosis is not yet fully understood. The idea of a hematogenous toxic effect of fluoride on anameloblasts during the development of the dental epithelial organ, leading to improper formation of enamel, should be considered more justified.
It is assumed that fluoride, being an enzymatic poison, reduces the activity of phosphatase and, thereby, disrupts the mineralization of enamel. Yu.A. Fedorov et al. (1972) believe that fluorine, when administered orally and even locally, quickly penetrates and blocks and affects the activity of the thyroid gland. It is likely that changes in thyroid function are the most likely explanation for the adverse effects of fluoride on enamel mineralization.
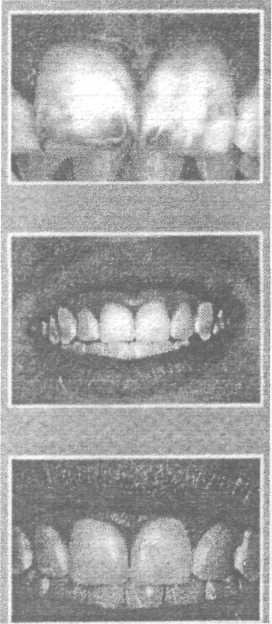
Teeth with fluorosis are called “speckled”, “pockmarked enamel”, “spotted enamel”, “burnt” (Fig. 6.1; 6.2).
Foci of endemic fluorosis are characterized by a decrease in the prevalence and intensity of dental caries. However, research by Koshovskaya V.A. (1975) and Kovalenko L.I. (1977) indicate that the incidence of caries in an endemic focus of fluorosis is influenced not only by fluoride, but mainly by other macro- and microelements contained in drinking water and food products.
The most vulnerable period in terms of the possible development of fluorosis is childhood, namely the period of mineralization of tooth germs (from 3 months to 4 years) and the period of incomplete mineralization of enamel in the first 1-3 years after the eruption of permanent teeth.
While the majority of people living in an endemic focus of fluorosis have significant changes in the dental tissues, some people have only mild lesions. Moreover, in such areas there are children whose teeth are completely healthy. This proves that the severity of dental fluorosis is determined by the degree of sensitivity of the body to fluoride intoxication and its ability to resist this effect.
With fluorosis, symmetrically located teeth are affected, and the degree of manifestation of the disease is usually the same. The most pronounced clinical picture of this disease is observed on the central incisors and first molars, which is associated with calcification of their crowns in the first year of life, when the child’s body is significantly exposed to adverse environmental factors. Teeth, mi-
Rice. 6.1. Dental fluorosis. Erosive form
208 ♦ Dentistry
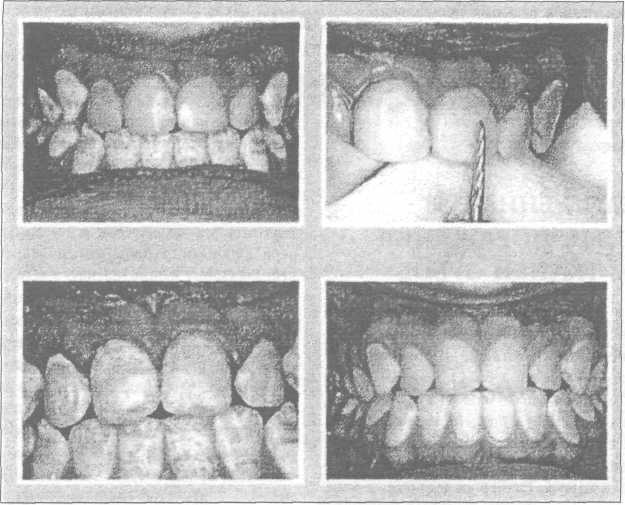
Rice. 6.2. Dental fluorosis. Chalky-speckled form (according to T.P. Kroll)
whose neuralization occurs at an older age are affected by a milder degree of dental fluorosis.
Depending on the severity of dental changes in endemic fluorosis, the following clinical forms are distinguished (Patrikeev V.K., 1973):
- line form characterized by faint, chalky stripes on the enamel of the anterior teeth of the upper jaw;
- spotted form characterized by the presence of well-defined chalky spots located over the entire surface of the teeth. A special feature of this form of dental fluorosis is that the enamel in the area of the stain is smooth and shiny. Sometimes there is faint light yellow pigmentation;
- chalky (mottled) form manifests itself in the area of all, not just the front teeth, and is clinically very diverse: white shiny and matte spots, areas of pigmentation of spots from light to dark brown. The spots are usually located on the vestibular surface of the front teeth. Sometimes there are small round enamel defects - specks. With this form, there is rapid abrasion of the enamel with exposure of pigmented dentin of a dark brown color;
- erosive form is characterized by more severe damage to teeth and is accompanied by the formation of defects-erosions in the area of chalky altered enamel;
- destructive form characterized by a violation of the shape of the crowns due to erosive destruction and abrasion of hard tissues. The destructive form is observed in areas with increased content fluoride (10-12 mg/l) in drinking water. With this form, the dental tissues are fragile; their breakage and, as a consequence, injury to the oral mucosa are often observed.
Fluorosis of primary teeth is extremely rare (single cases have been described), even in endemic areas, and mainly on molars. This is explained by the ability of the placenta not to allow excess fluoride to pass through to the fetus. Fluorosis of baby teeth is associated with early complementary feeding of infants, or with an increased concentration of fluoride in breast milk.
Morphological changes in teeth affected by fluorosis are determined mainly in the enamel, more often in the surface
nom its layer. The structure of the enamel on the thin section appears to be sharply emphasized, which is explained by the partial resorption of both enamel prisms and the interprismatic substance. As a result of the resorptive process, the enamel prisms themselves adhere less tightly to each other.
The Gunther-Schräger stripes are clearly pronounced, arching and reaching the enamel; the Retzius stripes are clearly visible. The dentin-enamel junction has a jagged shape. The surface layer of enamel has a moiré pattern, which is caused by an increase in interprismatic spaces due to partial resorption of enamel prisms, zones of hypo- and hypermineralization.
Fluorosis at the spot stage is differentiated from caries, which is characterized by a single lesion in areas typical for caries. With fluorosis, the lesions are multiple, located over the entire surface of the tooth crown and appear from the moment teeth erupt. Mild manifestations of fluorosis may have a similar clinical picture to the spotted form enamel hypoplasia. Severe forms of fluorosis, accompanied by the formation of erosions and other defects of the tooth crown, must be differentiated from caries, banal erosion, wedge-shaped defects, etc. (Table 6.1; 6.2).
Treatment. Therapy for fluorosis depends on the stage of the process. For the spotted and streaked form, local treatment, the essence of which consists of bleaching followed by remineralizing therapy, has a positive effect. E.V. Borovsky (1978) recommends bleaching with solutions of inorganic acids.
Recently, they have been trying to replace acid etching of enamel with fluorosis by grinding its surface to 20-70 microns. T.P. Kroll (1990) proposed a method for grinding off fluorous stains using a paste containing hydrochloric acid, carborundum and silicon gel (Fig. 6.3 a, b, c).
In case of erosive and destructive forms of damage, accompanied by a violation of the integrity of the enamel, methods are used to restore the shape and color of the tooth crown. Delayed filling with composite and filling materials is recommended after remineralizing therapy (general and local). Prosthetics with veneers and crowns are also possible.
Non-carious lesions of teeth♦ 209
Table 6.1 Differential diagnosis of caries and non-carious lesions that occur before teeth eruption
|
Signs | |||
|
Enamel hypoplasia | |||
|
Time of occurrence |
After tooth eruption |
Before tooth eruption |
Before and after tooth eruption |
|
Which teeth are affected? |
Equally dairy |
Mostly permanent |
Mostly permanent |
|
and permanent | |||
|
Localization on the surface |
Fissures and pits, contact |
Symmetrical for names of the same name |
Atypical for caries throughout |
|
crown wear |
surface, cervical |
teeth. Vestibular and lingual |
tooth surface |
|
teeth area |
surfaces, cusps of molars and | ||
|
premolars. | |||
|
Number and color of spots on |
Most often single, chalky or |
Most often single, chalk |
Multiple, chalky, yellowish |
|
brown |
to brown, fuzzy line |
||
|
demarcation |
|||
|
Sounding results |
Defect surface |
The surface of the defect is dense |
|
|
rough | |||
|
Permeability for |
Increased significantly |
Not enlarged |
|
|
dye | |||
|
Fate of the spot |
Rarely disappear, often in place |
Doesn't disappear |
May disappear with age. More often |
|
spots appear superficial |
does not change, progresses slowly. |
||
|
Susceptibility increases |
Doesn't matter |
Occurs in areas with |
|
|
drinking water |
with a decrease in content |
increased fluorine content in |
|
|
drinking water. |
|||
Prevention. Preventive measures are divided into collective measures aimed at reducing the fluoride content in drinking water, and individual preventive measures. Reducing the amount of fluoride in drinking water can be achieved by replacing the water source or reducing the content through drinking water purification techniques.
Individual preventive measures should be carried out from the moment the child is born. It is necessary to avoid artificial feeding and early introduction of complementary foods to the child. With the introduction of complementary feeding to a child, the main amount of water in food should be replaced with milk and juices. Additional introduction of vitamin C, D, and calcium supplements into food significantly reduces the manifestations of fluorosis. It is also necessary to remove children from the endemic area for the summer.
Prevention and treatment of dental fluorosis should be carried out comprehensively, taking into account the severity of the lesion, the general condition of the body and the influence of endemic factors. It should begin in early childhood and be carried out
systematically, using all available municipal and individual measures.
The general effect on the body and teeth affected by fluorosis should include:
1) stopping or at least limiting the intake of increased concentrations of fluoride into the child’s body from drinking water and food. For this purpose, it is recommended to use water from a water source with a low fluoride content for drinking and cooking. If this is not possible, partial defluoridation of water is recommended by boiling it for 5-10 minutes and then settling.
The removal of children from the endemic area for the summer period is very important in the prevention of fluorosis. Clinical observations have shown that replacing water sources for 3-4 months annually in the first 8-10 years of a child’s life helps normalize the formation of enamel and significantly reduces the percentage of dental fluorosis;
Table6.2
Differential diagnosis of non-carious lesions
|
Signs | ||||||
|
Superficial caries |
Hypoplasia |
Wedge-shaped defect | ||||
|
Short-term pain from chemical irritants |
Aesthetic defect, possible short-term pain from all irritants |
Aesthetic defect |
Short-term pain from all irritants is possible, but may be painless |
Short-term pain from temperature and chemical irritants |
||
|
Localization |
Fissures, pits, contact surfaces, cervical area |
Vestibular surface of incisors and canines in the middle third or throughout the entire crown |
Symmetrical, but atypical for caries. Vestibular, lingual surfaces, cusps of molars and premolars. |
Vestibular surface in the area of the tooth neck |
More often, the vestibular surface, the cutting edge of the front teeth, can be on any surface |
|
|
Characteristics of the lesion |
Roughness, defect within the enamel. The probe stays in the defect area |
Saucer-shaped defect, sometimes grooved, the bottom is hard and smooth. |
Defects in the form of small or large erosions, sometimes abrasion, chipped enamel |
Small depressions in the form of dimples or grooves with a smooth surface |
A defect in the form of a wedge with smooth bottom and walls |
Loss of enamel, reminiscent of increased abrasion. Sometimes the enamel takes on a chalky color |
Dentistry
Rice.6.3. Grinding off fluorous spots: a - fluorous spots on the central incisors; b - after sanding off the stains; c - 5 years after grinding (according to T.P. Kroll)
2) weakening the toxic effect of increased concentrations of fluoride on the body in general and dental tissue in particular, by prescribing a rational diet. Restriction in the diet of dishes prepared from sea fish, strongly brewed tea and other fluoride-rich foods. Recommended lean varieties of beef, pork, river fish. Dairy products - low-fat milk, cottage cheese. They are rich in calcium and, thanks to low content fats are better absorbed by the body. Juices made from vegetables and fruits growing in other areas are recommended for drinking;
3) the prescription of medications and specific treatment is carried out by a dentist, taking into account the severity of the lesion and general condition body. Considering the competitive relationship between fluorine and calcium, one of the calcium preparations is prescribed orally: glycerophosphate or calcium lactate in age dosages 1 hour before or 2 hours after meals. To weaken the ulcerogenic effect of calcium, before taking these drugs you need to drink 3-4 sips of warm, sweet, weak tea.
All children living in areas of endemic fluorosis are recommended to take drugs that increase the protective properties and resistance of the body (sodium nucleinate, potassium orotate, tinctures of Eleutherococcus, Schisandra, multivitamins);
Non-carious lesions of teeth do not depend on negative influence microflora on bone tissue. The main causes of pathology are congenital heredity, exposure to toxic substances, or the state of the mother’s body during pregnancy. This group diseases represents wide range pathological deviations of the hard tissues of teeth and the enamel layer of a congenital or acquired nature.
IN modern dentistry It is customary to divide pathological deviations in the hard structures of teeth into three classes:
- lesions of intrauterine development;
- lesions after the eruption of molars.
The first class of pathology includes following reasons deviations:
- intrauterine pathology of molar formation;
- abnormal developmental disorder;
- formation of endemic;
- hyperplasia/hypoplasia of the enamel layer.
The second class includes:
- abrasion of crowns;
- plaque and pigmentation;
- acid/radiation tissue necrosis;
- hyperplasia/hypoplasia;
- injury to the crown/root/neck;
- acid erosion.
Non-carious lesions are characterized by varying degrees of distribution: from damage to a single tooth to entire sections of the dentition. They can also include abnormal development molars after eruption:
- crown fracture;
- dislocation/fracture of the neck and root.
Let us consider the symptoms and characteristics of lesions of hard dental structures in detail.
Hypoplasia and hyperplasia
This pathology refers to a defect in the formation of enamel mass due to disruption of metabolic cycles in tissue structures. The protein/mineral cycle, which occurs with deviations, causes irreversible pathological degeneration: underdeveloped enamel persists for life and cannot be restored.

Clinical picture of hypoplasia
This pathology is characterized by the appearance of grooves different sizes, pits and spots with missing enamel. Often grooves and rounded pits appear simultaneously on one molar. Non-carious lesions are located parallel to the chewing part and cover the entire surface of the tooth.
There are three types of hypoplasia:
- focal odontodysplasia - pathology of adjacent molars;
- systemic hypoplasia - pathology of several molars;
- local hypoplasia - damage to a single molar.
Focal pathology occurs in healthy babies. This type of disease is characterized by a reduction in the crown due to insufficiency of the enamel layer. The crowns have a yellowish coating and are rough. At the moment, the etiology of the deviation has not been identified.
Systemic is characterized by a deficiency of mineralization of all teeth or several molars of one period of formation. The pathology is provoked by a violation of metabolic cycles in the mother’s body during gestation or a violation of the baby’s diet after birth, or it is a consequence past infection. TO this disease may result from the mother taking tetracyclines during pregnancy or administering the medication to the child.
Hypoplasia also occurs in children:
- with congenital allergies;
- premature;
- due to hemolytic jaundice;
- due to birth trauma.
Hypoplasia permanent molars occurs due to an unbalanced diet and serious illnesses experienced by the baby:
- rickets;
- ARVI;
- brain disorders;
- gastrointestinal pathologies;
- pathology of the endocrine system;
- other serious illnesses.
Pathology in the formation of molars is observed in the first year of a baby’s life, when any disruption of metabolic cycles as a result of diseases can affect the formation of bone and enamel structures. Hypoplasia affects individual molars, however, with repeated somatic diseases the pathology spreads to the remaining teeth.
Hyperplasia
It is a point localization of excess amount of dental tissue due to disruption of metabolic cycles during the formation of molars. Hyperplasia looks like pearly (enamel) drops on the surface of the crown.

Endemic fluorosis
Non-carious lesions of this type are formed due to an excess of fluoride in tap water. Fluorosis is the localization of chalky inclusions on the surface of the enamel. Constant fluoride intoxication provokes changes in the enamel mass, as a result of which it loses its natural gloss and protective properties.
There are 4 degrees of fluorosis:
- weak - single inclusions, difficult to distinguish during visual inspection;
- medium - the spots acquire a yellowish tint, the lesion covers half of the tooth crown and spreads to several teeth at once;
- moderate - the lesion covers the dentition, is localized on most of the dental crowns and is characterized by pronounced pigmentation;
- severe damage - in this case, multiple spots merge into large lesions, characterized by severe abrasion and deformation of the teeth.
Important! Fluorosis is curable. Therapeutic measures are carried out by the dentist, however, to prevent the re-development of fluorosis, it is necessary to replace fluoride water with purified water and take care of proper metabolism.
Non-carious lesions in the form of abnormalities in the structure of the teeth
Developmental anomalies include several congenital factors:
- incorrect localization of molar primordia;
- abnormal formation bone tissue jaws;
- fusion of the roots of adjacent molars.
Jaundice in newborns can also lead to an anomaly due to Rh conflict between mother and fetus. However, this pathology affects only baby teeth, causing changes in the color of the enamel.
Note! Treatment of babies with tetracycline after six months leads to permanent molars turning yellow.
““ is also considered an anomaly. This pathology is formed due to the accumulation of tetracycline in the dental tissue. Not even large number the injected medicine turns the enamel yellow. A feature of this pathology is the color change of the crown from yellow to gray/brown under the influence of daylight.

Congenital abnormalities
Pathology data concerns abnormal development dentin. Treatment of pathology is carried out by masking the affected teeth orthodontic structures from various materials - metal, plastic, porcelain. When teeth are lost, dentures are prescribed.
Pigmentation and plaque
Pigmentation (staining of the dental crown) can be caused by several factors:
- consequences of serious illnesses;
- consequences of taking aggressive medications;
- due to pulp necrosis.
Temporary pigmentation also appears as a result of eating certain foods (blueberries, carrots), rinsing oral cavity medicines. Constant pigmentation is present in smokers: the enamel turns yellowish, sometimes brown.
Plaques can be soft or hard. When plaque hardens, it is referred to as tartar. Deposits of a loose consistency appear as a result of unscrupulous sanitation of the oral cavity or disease of the gum tissue. A person with healthy gums and a correct bite does not have deposits on their teeth. When the oral cavity is neglected, loose plaque hardens and turns into tartar.
Erasing
Erasure of the chewing plane is present in all people to varying degrees. Pathological abrasion was recorded in 11% of people and is formed by several factors:
- body constitution and heredity;
- pathology of metabolic cycles;
- defects in the functioning of the endocrine system;
- deviations in the functioning of the nervous system;
- some chronic diseases;
- quality of drinking water (increased mineralization);
- eating excess amounts of berries/fruits.
Pathological abrasion is caused by additional load when chewing due to the loss of a dentition or several molars, incorrectly selected dentures, and defects in tissue structures. Work in enterprises where there are a large number of mechanical particles in the air can also lead to abrasion.
There are three levels of washability:
- at the level of the enamel layer;
- at the level of the enamel-dentin layer;
- loss of 2/3 parts of the crown.
Teeth can wear down horizontally and vertically, sometimes mixed horizontal-vertical abrasion of the surface occurs.

Wedge-shaped defect
Non-carious lesions of this type are common among patients with problematic gums - periodontal disease. A wedge-shaped defect is characterized by exposure of the neck of the tooth. Dentists agree that the cause of the pathology is the presence of internal diseases:
- central nervous system;
- endocrine system;
The presence of these diseases affects the health of the periodontium, which, in turn, causes exposure of the neck of the teeth. Pathology can affect single teeth, but multiple lesions of periodontal tissues are more common.
Hard tissue erosion
It is considered a pathological decrease in the hard structures of the teeth. Sometimes the enamel itself becomes thinner, sometimes the enamel decreases along with the dentin. Some scientists believe that non-carious lesions of hard tooth tissues are caused by the abuse of juices and pulp of citrus fruits. Also the cause of the pathology are some internal ailments:
- endocrine abnormalities;
- neuropsychiatric disorders;
- violation of salt metabolism, etc.
Acid erosion can occur with an unhealthy diet dominated by acidic foods, frequent vomiting and improper use of medications.
Necrosis
This pathology can provoke the loss of single molars or all the patient’s teeth. A type of necrosis of solid structures is cervical necrosis, which can occur with certain metabolic cycle disorders. This disease often occurs in pregnant women. The disease is characterized by the formation of chalky streaks and thinning of the enamel coating on the affected surface.
Necrosis can form when:
- exposure (radiation);
- exposure to organic acids (acid);
- taking medications for Achilles gastritis (mild).
If dental care is not taken properly, caries forms in the affected areas. At active process pathological changes the enamel of the entire surface is loosened and dentin is exposed. When the enamel layer is lost, teeth become sensitive to temperature changes and other irritants.
Injury
A fall or careless chewing of rough food can cause injury. After an impact, you can lose one or more teeth at once. The consequences of an impact injury are:
- bruised/dislocated tooth;
- root/neck/crown fracture;
- fracture of a section of the crown;
- trauma to the molar bud in children;
- combined defeat.
Hyperesthesia
This pathology is characterized by increased sensitivity of dentin to force, chemical or temperature effects. A person experiences pain while drinking water and brushing his teeth. Hypersensitivity may occur when:
- exposure of dentin canals;
- transmission of stimulus impulses through tooth cement.
In addition, heightened sensitivity may appear due to the close location of the nerve roots to the surface of the tooth, which is due to the constitution of the structure. It is more common with carious lesions of dental tissue, pathological abrasion, and thinning of the enamel.

Hereditary pathology
These deviations are characterized pathological form mutation that is independent of environment. All hereditary pathologies can be divided into two classes:
- chromosomal;
- genetic
Gene mutations are transmitted along a related line and are characterized by the constancy of clinical manifestations. The class of gene pathology includes:
- defective dentinogenesis;
- defective odontogenesis;
- defective amelogenesis;
- discalorite.
Defective dentinogenesis forms three degrees of deviations:
- translucent bone, weak enamel;
- high bone fragility and abrasion of the crown, discoloration of the enamel coating;
- unusual shape and pigmentation of teeth: dome-shaped crowns, opalescent enamel color.
Enamel pathology is expressed in a reduced mass of the layer (hypoplasia), insufficient calcification (hypocalcification), and pathological structuring of apatite crystals in the enamel mass.
With imperfect odontogenesis, molars are distinguished by a gray tint, increased abrasion and fragility of the enamel surface. Amelogenesis imperfecta is characterized by a defect in the enamel mass: the surface of the crown has either partial or complete absence coverings.
With discoloration, the natural color of the enamel is disturbed. The color depends on the prerequisites for the formation of the disease:
- Rh conflict of blood groups of mother and baby;
- incompatibility of parental blood;
- pathology of the biliary system;
- porphyria (pathology of the metabolic cycle of pigment cells);
- treatment with tetracycline drugs during pregnancy.
Hereditary pathologies cannot be cured; in dentistry, cosmetic restoration is used - covering with crowns, veneers, etc.
(votes: 1, average: 5.00 out of 5)





