Improper oral care leads to the appearance of plaque and tartar. As a result of pathological processes, inflammation begins. At first, its symptoms are quite harmless. There is slight swelling and sometimes pain. It gradually increases, and a purulent secretion may appear. At this stage they are already talking about advanced periodontitis. To treat this disease, curettage of the periodontal pocket is used. What is this procedure? What other methods are used to combat the disease? You will find answers to these questions in today's article.
Brief description of the problem
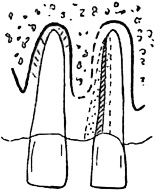
Against the background of the inflammatory process, bone tissue is gradually destroyed and replaced by granulation tissue. The latter consists mainly of osteoclasts and microbial elements. Day by day they spread to more and more areas, leading to even greater atrophy of the alveolar bone. A free area appears where there is no attachment of the gum to the surface of the tooth root.
As a result of the described changes, a periodontal pocket is formed. This is a space equal in size to the area of the destroyed bone. Its contents are granulation tissue, food debris and purulent secretion. The size of the gap formed is used to judge the degree of tissue deformation. U healthy person The depth of the periodontal pockets is no more than 3 mm, making it possible to freely clean the cavity from food debris. If this value exceeds the specified size, certain difficulties arise when caring for the oral cavity. The probability increases several times, which leads to the appearance of stone and plaque. The result active destruction tissue may result in tooth loss.
Diagnosis of pathology is carried out using x-ray examination or periodontal probe. Absence quality treatment Over time, it causes the pocket to deepen. The consequence of this process is the movement of the teeth into a “fan” position.
Causes of pocket formation
The main reason for the formation of a periodontal canal is poor hygiene oral cavity. Incorrect or lack thereof leads to the accumulation of bacterial deposits in the crown area. Microbes form a thin invisible film over the entire surface of the tooth enamel and begin to secrete products of their own vital activity. This is how inflammation of the periodontal pocket occurs.
Risk group
Among the factors that provoke the growth and reproduction of pathogenic flora, the following can be noted:
- improper diet, consisting mainly of carbohydrate foods;
- poor oral hygiene;
- bad habits;
- disturbances at the hormonal level;
- immunodeficiency;
- dental diseases;
- malocclusion;
- poor quality filling installation.
Symptoms of inflammation
The formation of a periodontal pocket can be asymptomatic for a long time. With the development of the inflammatory process, a characteristic clinical picture appears:
- discomfort in the gum area;
- bad breath;
- swelling, bleeding and redness of the gums;
- upon palpation, purulent secretion may be released;
- expansion of interdental spaces;
- deterioration of general condition.
If these problems occur, you should contact your dentist. A doctor's help is required even if the inflammatory process affects only one tooth. Every day the situation will only get worse, which can lead to the progression of the disease. 
Treatment methods
Before starting therapy, a diagnosis is carried out, with the help of which the doctor determines the degree of neglect of the disease. If the periodontal pocket does not exceed 0.15 mm and there are no signs of inflammation, therapeutic methods are used. The following procedures are commonly used:
- Hygienic cleaning using ultrasound. During the removal of stone and plaque, the gums are not damaged.
- Drug treatment. Prescribed immediately after ultrasonic cleaning. At mild degree pathological process Aseptic treatment is used (baths, irrigation, rinsing). During the procedures, Chlorhexidine or Miramistin are used. In particularly serious cases, the patient is prescribed a course of antibiotics. Characterized by the greatest efficiency the following drugs: Amoxicillin, Lincomycin and Azithromycin.
The listed procedures are ineffective if the pocket depth is more than 2 mm. The doctor will not be able to completely remove the accumulated stone. In addition, the likelihood of additional periodontal trauma increases. As a result of the manipulations, the inflammatory process and tissue destruction begin to progress.
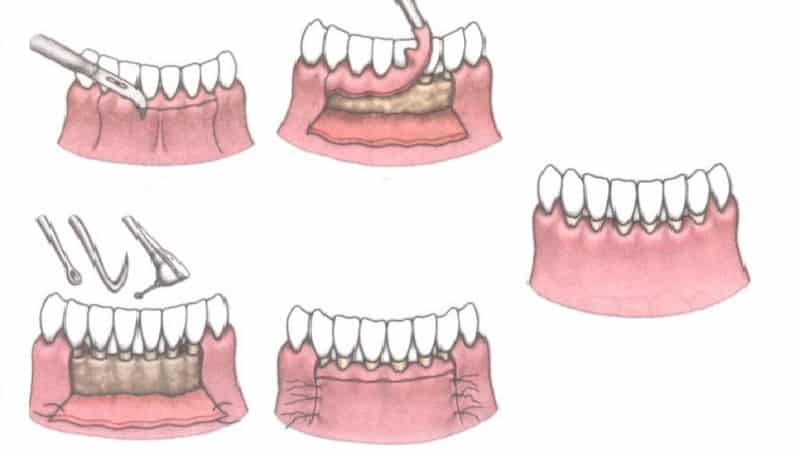
In case of complicated course of the disease, surgical intervention is recommended. This method treatment involves mechanical impact with dental instruments on the subgingival areas. Currently the most effective procedure This type is considered to be curettage of the periodontal pocket. What is it? There are several types of manipulations: closed, open and patch surgery. The procedure itself allows you to get rid of all the problems caused by periodontitis. Let's consider each of its options in more detail. 
Open curettage
Such an intervention requires high professionalism from the doctor. Therefore, this service is not provided in all medical institutions. The duration of the procedure is about 2.5 hours. It consists of the following stages:
- Cleaning teeth from tartar and plaque.
- Use of anti-inflammatory drugs.
- Splinting of mobile teeth.
- Dissection of the gingival flap with a scalpel.
- Removal of granulations and stones using ultrasound.
- Antiseptic treatment of tooth roots.
- Planting synthetic tissue into the pocket to enhance natural bone growth.
- Apply sutures and cover the damaged area with a gum bandage.
After about 1.5 weeks, the sutures are removed. After a few more months, the damaged tissues are completely restored. Gingival papillae can completely cover the spaces between teeth. In some cases, open curettage of periodontal pockets leads to exposure of the roots. Therefore, it is recommended to avoid eating hot, sour and cold foods for some time. 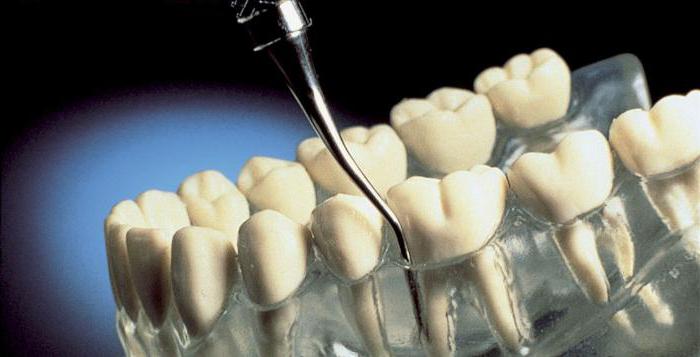
Closed curettage
The operation is effective when the pocket depth is 3-5 mm. The intervention is not complicated. It consists of the following steps:
- Examination of gums.
- Administration of local anesthesia.
- Treatment of periodontal pockets without cutting the gums.
- Tooth root polishing.
The intervention can simultaneously affect 2-3 teeth. Wound healing takes place within one week, but final recovery takes about a month. This is how long it takes for connective tissue to form and attach the gum to the tooth. The main disadvantage of the procedure is that the doctor at the time of the manipulation does not see whether everything is pathological formations deleted.
If the pocket depth is more than 5 mm, closed curettage will only halt the progression of periodontitis. Partial removal of deposits and granulations allows for a temporary respite, but in almost all cases the disease resumes its development.
Flap surgery
This surgical procedure involves cutting the gums to gain access to the periodontal pocket. Recommended if its dimensions do not exceed 4 mm.
First, the doctor makes two small incisions with a scalpel and peels off the mucoperiosteal flap. Then standard mechanical cleaning of the pocket and polishing of the tooth surface is carried out. After completing the treatment of hard surfaces, they proceed to the preparation of soft tissues. The flaps are placed in place. At the end of the procedure, an osteogenic medicine is applied to the affected area, and the gum itself is sutured. The entire operation lasts no more than 40 minutes, but involves the use of local anesthesia.
Some patients are additionally prescribed for external use (for example, Furacilin). It is also recommended to use ointments to stimulate the process of gum epithelization (Actovegin, Solcoseryl). 
Vacuum curettage
Subject to availability purulent abscesses and deep pockets (more than 5-7 mm), vacuum curettage is used. Cleaning is carried out using anesthetics. During this procedure, the doctor first scrapes off the tartar deposits and then polishes the tooth structure. After this, the specialist begins to remove granulations and damaged epithelium from the internal walls. The periodontal pocket is cleaned using a vacuum device, which sucks out necrotic masses along with stone fragments from the bottom of the cavity. At the final stage, rinsing with antiseptic preparations is mandatory.
Vacuum curettage is characterized by high efficiency. With the help of the procedure, lymph flow in the tissues is restored, the depth of the gum pockets is reduced and all inflammatory processes are eliminated.
Postoperative period
In order not to open periodontal pockets, it is recommended to refrain from eating and drinking for 10 hours after all manipulations. To get the desired result, you should brush your teeth carefully, using a soft bristle brush. Problem area must be avoided. After a week, you can start rinsing. To do this you need to use a weak brine or "Chlorhexidine". 
Regarding nutritional issues, preference should first be given to soft or pureed foods. Drinking cold or excessively hot drinks is strictly prohibited. For a week after curettage of periodontal pockets, it is recommended to avoid physical activity, playing sports, visiting the sauna. In the postoperative period, it is important to monitor the condition of the oral cavity. You can use hygiene products intended for sensitive teeth. If necessary, you should contact your dentist. The specialist will select procedures to reduce the sensitivity of the necks of the teeth.
Today it is very common dental pathology is periodontitis. This disease is characterized by the fact that in addition to the symptoms of inflammation, a pocket appears in the gum between the teeth, how to treat this process – important question. An untimely course of treatment can lead to serious consequences, up to the loss of all dental units.
The cause of the disease is dental plaque and poor hygiene care behind the oral cavity. As you know, teeth need to be brushed 2 times a day. In the morning, cleaning should be done after breakfast, and not before meals. Many patients do it incorrectly and brush their teeth after sleep. However, in this situation, after breakfast, food residues and plaque accumulated overnight remain on the teeth. These deposits continue to negatively affect  oral tissue throughout the day.
oral tissue throughout the day.
If a person does not brush his teeth for some reason before going to bed, then soft plaque begins to gradually transform into. First, it forms above the gum, and this leads to the development of inflammation. The inflammatory process is characterized by swelling of the gums, bleeding and pain.
If the patient does not remove plaque and tartar in time under conditions dental clinic, then supragingival tartar begins to grow towards the root of the tooth.
Such a stone sinks under the gum, pushing it lower and lower. As a result, gum recession occurs, a pocket appears in the gum between the teeth, how to treat this state- this is a question that at this moment begins to interest and disturb any patient. After all, no one is happy about the prospect of soon being left without teeth.
Treatment
Let's figure out how to treat a pocket between teeth and a photo of the pathological process.

Photo at the time of formation of supragingival tartar
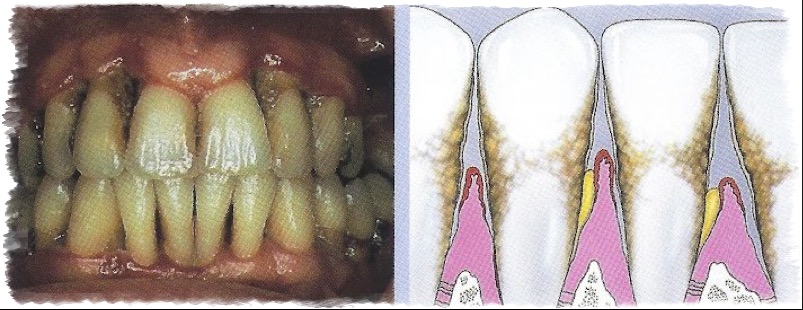
Photo at the time of formation of abundant subgingival dental plaque
Treatment of this pathological process is necessary only from a dentist. Many patients begin to look for information about the question: “A pocket in the gum between the teeth, how to treat it at home?” This can be called a big mistake. Home treatment It only relieves the symptoms of inflammation, but does not cure. The longer treatment is delayed, the more serious the complications will be.
Treatment at the dentist's office consists of: professional hygiene oral cavity. A large amount of plaque and granulation also accumulates in the periodontal pocket, so cleaning them is mandatory. To clean pathological periodontal pockets, use the open or closed curettage. Due to the fact that this condition is accompanied by gum recession, it needs to be returned to its place. For these purposes, use one of the many methods patchwork operations when the mucous membrane moves.
If the process is very prolonged, mobility of the affected teeth may be observed, then they need to be immobilized using a special splint. Today, dentists more often use special fiberglass tapes. They do not aesthetically differ from the color of natural dental tissues, so they will not be noticeable on the teeth. In terms of strength, the material also meets all requirements and is able to withstand chewing loads.
A periodontal pocket is the space between the gum and tooth. Normal soft fabrics fit tightly to the dentition, and the space between them does not exceed 1 - 2 mm. However, as the inflammatory process develops, the areas become larger and plaque and pathogenic microorganisms accumulate in them.
Periodontal pockets appear due to gum diseases – periodontitis, periodontal disease and gingivitis. Due to inflammation, the integrity of the soft tissues is disrupted, they begin to “move away” from the enamel, the necks of the teeth are gradually exposed, and atrophy of the alveolar bone occurs.
Only periodontitis is accompanied simultaneously infectious inflammation and tooth mobility. With periodontal disease, the destruction of connective tissue occurs without the formation of pus, and with gingivitis, the integrity of the dentition is preserved.
Periodontitis creates an ideal environment for the proliferation of microbes and bacteria. The bottom is filled with food particles, plaque and pus. The patient cannot fully clean the pocket on his own. Over time, the process worsens: the space is filled deeper and deeper with hard deposits, and granulation tissue and alveolar processes atrophy.
Important! The main methods for examining gum pockets are radiography and probing. The image clearly shows darkened areas in the place where the soft tissues move away from the tooth.
There are three stages of the disease:
- Easy. The pocket depth is up to 3.5 mm.
- Average. Destructions reach 4 mm.
- Heavy. Lesions exceed 5 mm.
Causes and symptoms
The main factor leading to the formation of periodontal pockets is the accumulation of bacteria and plaque, which literally sticks to the surface of the enamel. The reasons for the development of pathology include:
- Poor or improper oral hygiene.
- Use large quantity soft and carbohydrate foods: sweets, baked goods, fast foods.
- Lack of solid vegetables and fruits in the diet: hard food helps get rid of plaque, promotes proper blood supply to the gums and strong teeth.
- Bite defects: crowding, crooked teeth.
- Diabetes mellitus.
- Hormonal imbalance.
- Immunodeficiency.
- Poor quality or incorrectly made fillings, crowns, bridges, dentures.
The main factor leading to the formation of periodontal pockets is the accumulation of bacteria and plaque.
Important! Smokers are most susceptible to plaque formation on their teeth. Nicotine resins cover the surface of the enamel, especially with inside. For patients with bad habit mandatory professional cleaning to avoid the risk of developing periodontitis.
The formation of periodontal pockets is accompanied by:
- Itching in the gums.
- Bleeding due to mechanical impact.
- Bad breath that does not disappear even after brushing and rinsing with solutions.
- Separation of purulent contents when pressed.
- Reaction to cold, hot, sour, sweet.
- Discomfort while eating.
- Visual enlargement of the tooth due to periodontal dystrophy.
- Mobility and loosening of teeth - in severe stages.
Treatment
Treatment of periodontal pockets is carried out in several ways. Which technique will be chosen depends on the depth of the lesion and the stage of the disease.
Laser cleaning
It is used at the first stage of pathology. Tartar is removed using the Vector dental apparatus. High-frequency ultrasonic vibrations emitted by the scaler attachment remove deposits located in periodontal pockets. At the same time, the gaps are disinfected and pathogenic microorganisms are eliminated.

Laser cleaning is usually performed without anesthesia.
Important! Laser cleaning is usually performed without anesthesia. The procedure is painless, it is possible slight discomfort. Anesthesia is used if the patient has increased sensitivity or he is very afraid.
Photodynamic therapy
PDT – modern non-surgical method treatment of any stage of the disease. The gum pocket is cleaned of plaque and applied special drug– concentrated chlorophyll. It is made from seaweed– spirullina. The substance promotes the development of photosensitizers.
When exposed laser beam an oxidative reaction begins with the release of oxygen. Microbes and bacteria die, and a protective layer forms on the mucous membrane. At the end of the procedure, the gum pockets are closed. Further therapy is aimed at restoring bone and granulation tissues.
Curettage
The most common treatment method. There are two types of procedure:
- Open. It is carried out when the depth of the pockets does not exceed 5 mm.
- Closed. It is used in the third stage of the lesion.
The general principle of both closed and open curettage is the same. The only difference is the excision of soft tissue. It is carried out with the second type of method.
The procedure consists of several stages:

Important! Usually they prefer to perform an open type of curettage. It is more effective and gives full access to the gum pockets.
After the procedure begins recovery period. It lasts from 14 to 21 days. By the end of the third week, connective tissues are completely restored.
Flap surgery
Surgical intervention is carried out at the third stage of the disease, when the periodontal pocket has reached a depth of 5 millimeters or more. The operation is traumatic, painful, accompanied by physical and psychological discomfort. But it allows you to completely eliminate connective tissue damage.
Procedure steps:
- Anesthesia.
- Vertical excision of the gums in two places.
- Peeling of the periosteal flap.
- Mechanical removal of affected tissue, dental plaque, pus.
- Antiseptic treatment and application wound healing drugs stimulating the growth of new cells.
- Stitching.

After flap surgery.
Important! As the anesthesia wears off, patients begin to feel pain. Therefore, after surgery, it is recommended to take painkillers.
During the rehabilitation period, wound healing gels and antiseptic solutions for rinsing. The most commonly prescribed medications are Asepta, Metrogyl Denta, Solcoseryl, and Actovegin. If the disease is accompanied by an extensive inflammatory and purulent process, antibiotics are indicated.
Prices
The cost of treating periodontal pockets depends on the type of procedure and the amount of area treated. Average prices for therapy:
- Treatment with the “Vector” device - 2,500 per jaw,
- Closed curettage - 1,400 per tooth,
- Open curettage - 2,700 per tooth,
- Flap surgery - From 2,500 to 3,500 depending on the number of roots in the tooth,
- PDT - 1,500 for one gum pocket.
A periodontal pocket appears with the development of periodontitis. The disease is accompanied by pain, bleeding, and advanced cases– violation of interdental bonds and adentia. Treatment is carried out using laser devices, mechanical cleaning and surgical excision.
The depression that forms between the tooth and gum is called a gum pocket. In normal condition, the size of the depression does not exceed three millimeters. This allows it to clear itself of various epithelial remnants and food that accumulate in the space of the formed neck around the tooth.
Gum pocket is a reversible condition that can be cured proper hygiene. If you have a disease, such as periodontal disease, you will need treatment from a dentist. Especially in the case of inflammation, pain, swelling of the gums with pus discharge, surgery may be used. Otherwise, it will lead to tooth loss.
In case of inflammation of the gum pocket, treatment is carried out in different ways. Therapeutic methods are used if the depth is no more than 4 mm. First of all, it is necessary to clean the tooth from plaque, tartar, microbes, and deposits so that the neck closes and the attachment of the gums to the teeth is restored.
On early stages development of the disease, rinsing with antiseptic solutions, medications, and careful hygiene procedures is carried out.
If bleeding occurs, you should consult a doctor. Treatment procedures are carried out using:
- hand tools;
- ultrasonic scaler;
- photosensitizer;
- surgical operation.
The pocket area is cleaned with an ultrasonic sclera, then the surface of the tooth root is treated with polishing. Excess growths are removed from the inflamed tissue. Thus, conditions are provided for the restoration process for normal attachment of the gums to the teeth.
Photodynamic therapy – modern method, with which they are treated launched form illness without surgical intervention. The principle of the method is that after brushing your teeth, a special substance consisting of concentrated chlorophyll is applied to the surface of the gums.
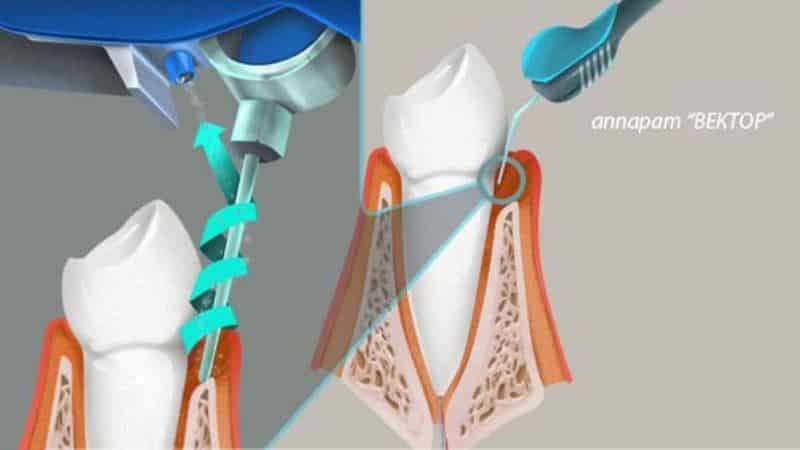
Operating principle of the ultrasound device “Vector”
It is obtained from spirullina - seaweed. Photosensitizers develop in destroyed, inflamed cells under the influence of the drug, and after that, after a certain period of time, the specialist applies a laser beam to the gums. Its light affects photosensitizers with the release of oxygen. In this case, an active oxidative reaction occurs, as a result of which pathogenic flora and harmful bacteria die. When the affected tissue areas in the periodontal pocket are removed, it closes completely. With one procedure, you can completely cure the pocket and get rid of inflammation and bleeding. If the treatment is carried out with a laser, a protective formation is created on the mucous membrane, preventing microbes from entering the gums, and also promotes restoration normal condition pocket After procedures to remove infected gum tissue, it is necessary to restore bone tissue. Successful therapy will be in the case full recovery periodontal joints and gum functions.
If the pocket exceeds 4 mm, surgery will be required.
For this, a patchwork technique is used, in which the gums are peeled off in the area of several teeth located nearby. Pockets are cleaned after opening manually, and then the tooth root is treated and the gums are sewn on.
Surgical treatment of gum canal
This operation is almost always performed with a positive effect, but the only disadvantage of the procedure may be the difficulty in psychological aspect for the patient himself. You can see the result of the dental pocket operation, the photo of which is presented above.
Many patients are interested in how to treat a pocket in the gum between the teeth using curettage technology, which is often recommended by specialists. It is considered effective and less painful. There are open and closed methods. During the procedure, the gum pockets are thoroughly cleaned of deposits, tartar, and altered tissues.
The dentist prescribes cleaning based on the degree of the disease.
- Closed curettage carried out with a laser, ultrasound at a small depth of formation, not exceeding 5 mm.
- Open curettage represents surgery which is carried out using anesthetic drugs. The process involves making an incision in the gums in the area of the interdental papillae, then cleaning and applying an effective healing agent, after which the wound is sutured.
The result after curettage is noticeable after two weeks. Swelling, redness, and bleeding of the gums disappear, and the depth of the pocket is reduced. To find out how to treat pockets in the gums, which method will be better, you need to seek advice from specialists at the first signs of the disease.
Treatment, which will be carried out under the supervision of doctors, will prevent various complications.
Preventive measures
To prevent re-treatment in the dental pocket, should be carried out preventive measures timely. When the curettage procedure is performed, the doctor prescribes a series preventive measures that should be performed regularly:

To prevent gum disease, you should visit the dentist at least twice a year.
- brushing teeth;
- use cleaning products and pastes that have an abrasive effect, where deposits are removed with the help of solid particles and polished teeth;
- use floss ( dental floss) for cleaning between teeth;
- preventative visit dental clinic at least twice a year;
- Following additional doctor’s recommendations will reduce the growth of pockets and prevent complications of various types.
Treatment with folk remedies
Patients, when visiting a dentist, often ask whether a dental pocket can be treated at home.
Experts say it is quite possible to carry out treatment folk remedies if the disease does not have serious complications.
In this case, antiseptic solutions and decoctions of medicinal plants with a wound healing effect. Several recipes can be found below.

In conclusion, it should be noted that self-treatment It is not recommended to treat gum disease without consulting specialists. Preferably medical procedures perform in combination traditional methods with traditional medicine.
Clinical observations have shown that timely use surgical methods treatment according to indications for complex treatment periodontal diseases allows you to provide the most long-term remission processes in the periodontium, reduces treatment time and prevents the progression of diseases.
Opening the abscess. Abscess is limited purulent inflammation fabrics.
Abscesses located in the thickness of the interdental papilla are opened in a “blunt” way - through the pathological periodontal pocket, a thin stroker is used to enter the abscess cavity. Such an autopsy can be performed under topical anesthesia - a turunda soaked in an ultracaine solution is first introduced into the periodontal pocket. An abscess that forms in the attached gum and below is opened with incisions, often vertical. After opening, treatment is carried out with antiseptics (dioxidine, peroxide, hypertonic solution, etc.).
Curettage. Curettage of periodontal pockets is one of the main surgical methods of periodontal treatment. The purpose of curettage is to eliminate periodontal pockets. To do this, mechanically ingrown epithelium, granulations, necrotic cement of the tooth root, subgingival calculus are removed, then they influence the microflora, stimulating reparative processes in periodontal tissues. The ideal task is to increase the level of periodontal attachment, therefore curettage is carried out under a number of conditions: relieving inflammation, eliminating supracontacts, eliminating perigingival defects and restoring interdental contacts using filling. However, the main condition for curettage is the patient’s stable hygienic motivation.
As a result of curettage, a clean wound surface is obtained. During the operation, blood flows into the cavity of the periodontal pocket and forms blood clot, which is organized in connective tissue, cicatricial wrinkling of the periodontal pocket occurs, and connective fibers grow into the layer of newly formed root cement.
To perform curettage, use a set special tools: hooks, excavators, rasps, set of curettage spoons.
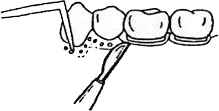
Curettage (scraping) is carried out to eliminate periodontal pockets, the depth of which does not exceed 4-5 mm, since with deeper pockets it is impossible to visually control all manipulations. During the operation, blood is poured into the cavity of the pocket, which is organized into a blood clot, which has a beneficial effect on the wound healing process.
No more than 3 periodontal pockets can be treated at the same time after infiltration anesthesia 1-2% lidocaine solution and more modern anesthetics. Subgingival tartar and pathologically altered cement are removed using sharp hooks, excavators, and a rasp. All tooth surfaces are sequentially treated - vestibular, approximal and oral. When removing dental plaque, the instrument is directed from the apex of the root to the crown of the tooth. Then the softened cement is removed, after which the root surface is finally treated with a scaler. The pocket cavity is washed from a syringe with a solution of furatsilin (1:5000) to remove solid residues.
Next, begin processing the bottom of the pocket. Using sharp instruments, carefully scrape out the granulations. The last stage - de-epithelialization of the gingival wall of the pocket - requires caution and skill from the doctor in carrying out such an intervention. Thumb press the gum to the tooth, insert a sharp curette to the bottom of the pocket and, under finger control, cut off the epithelial lining by moving the instrument towards the crown of the tooth, eliminating the barrier to the attachment of the gum to the tooth. Next, the gum is pressed against the tooth and a protective bandage is applied.
The patient is given instructions on observing the rules of oral hygiene, is prescribed a gentle diet, and is recommended to rinse with alkaline and hypertonic solutions. Probing the pocket is prohibited. The gum bandage is changed every other day for a week. It is not recommended to inject medications into the pocket so as not to disrupt the process of formation of new connective tissue attachment and resumption of bone growth.
After curettage, periodontal tissues may develop inflammatory reaction, accompanied by pain on percussion, swelling, and, less commonly, the appearance of lymphadenitis. Complications most often arise due to rough curettage. Treatment consists of frequent rinsing with a solution table salt And baking soda(1 tsp per glass of water) with the addition of 1/2 tsp. Lugol's solution in a glass of water or herbal infusions (sage, chamomile, etc.).
Increased sensitivity (hyperesthesia) to temperature and tactile influences occurs after removal of pathologically altered cement and the surface layer of dentin. Treatment comes down to the prescription of fluoride preparations (applications of a 1-2% sodium fluoride solution, fluoride varnish, fluoride-containing gels, a preparation for deep fluoridation).
Contraindications to curettage include thin gingival pocket walls and the presence of bony pockets.
Removal of gingival papillae produced for hypertrophic gingivitis, gum fibromatosis. The operation is performed under infiltration (intrapapillary) anesthesia. An incision is made at an angle of 30-45° to the bottom of the gingival sulcus, after which the overgrown tissue is removed. Using sharp excavators and hooks, tartar is removed, the wound surface is coagulated and a gingival bandage is applied, which is changed every other day until complete epithelialization.
The indication for curettage is a periodontal pocket with a depth of 3-4 mm, absence of erosion of the gingival wall, uniform bone resorption of the alveolar process (absence of bone pockets).
Curettage is contraindicated in acute inflammatory process(abscess, gum erosion), tooth mobility of the III degree.
Basic principles of curettage formulated by V.E. Krekshina:
- complete anesthesia of the operated tissues;
- simultaneous treatment of no more than 2-3 teeth;
- careful treatment of processed tissues;
- blood clot protection;
- maintaining oral hygiene.
Before curettage, antiseptic treatment of the oral cavity and periodontal pockets is carried out with weak antiseptic solutions: hydrogen peroxide, furatsilin, chlorhexidine bigluconate. Strong antiseptic solutions delay healing.
Curettage begins with curettage of the inner wall of the periodontal pocket. The tooth surface is carefully freed from subgingival tartar and necrotic cement using an excavator, hook or rasp.
| Rice. |
Then the pocket is washed with a warm isotonic solution, pressed against the tooth and a protective bandage is applied for 3-5 days. Protective dressings should not irritate or put pressure on the gum tissue.
Dentol, stomalgin, upin, septopakley MK are used as dressings; a therapeutic dressing consisting of sodium preparations on fir balsam, rosehip oil, methyluracil, zinc oxide and dentin.
In the postoperative period, the patient is prescribed a gentle diet, oral baths with herbal infusions, and rational oral hygiene (the curettage area is not treated with a toothbrush for 2-3 days). The pocket should not be probed after curettage for 3 weeks. Restoration and epithelization of the gap occurs after 7-10 days, maturation of collagen fibers - on the 21st day.
The disadvantage of curettage is bleeding, which significantly impairs vision surgical field, which hinders the thoroughness of its implementation. In this case, it is possible for fragments of tartar to penetrate deep into the soft tissues and cause periodontal infection.
After curettage, there is a risk of developing the following complications: lymphadenitis, abscess, retrograde pulpitis, bleeding, increased sensitivity of teeth to temperature and tactile stimuli.
For lymphadenitis and abscess, antibiotics and sulfonamide drugs are prescribed; for pulpitis, the tooth is depulped; heavy bleeding from the pocket it is washed with hemostatic agents, and the gum is pressed to the tooth with a tight bandage. Dental hyperesthesia is relieved with fluoride preparations.
Curettage is carried out no more than once a year, because repeated interventions thin tissues and reduce their reactivity.
Curettage options include vacuum curettage and cryo-curettage.
Vacuum curettage- scraping of periodontal pockets under vacuum conditions. It is carried out using an apparatus consisting of containers and a compressor. When the device is turned on, after 3-5 seconds a vacuum is created in one of the containers, which allows blood, mucus, plaque, particles of tartar and granulation, and destroyed parts of the alveolar bone to be sucked out. At the same time, excess pressure is created in the second vessel, allowing the solution to be supplied medicine into the area of the surgical field. Before surgery, curettes are fixed in a special tip-holder. This device was designed by N.F. Danilevsky in co-authorship.
Vacuum curettage is indicated for periodontal pocket depths up to 7 mm, with the development of single or multiple abscesses. In the presence of bone pockets, vacuum curettage is combined with gingivotomy. Anesthesia is performed first.
Vacuum curettage is carried out in the following stages:
- Subgingival tartar and destroyed cement are removed from the surface of the tooth root: from the neck to the apex of the tooth root and to the bottom of the periodontal pocket. The operation is completed by polishing the treated surface.
- The overgrown granulations and strands of epithelium from the outer wall of the pocket are scraped out ( inner surface gum facing the tooth) using a curette and crescent hooks.
- The bottom of the pocket and the alveolar ridge are treated. Granulations from the bottom of the pocket are removed with sharp hollow tips, and the alveolar edge is smoothed with cutter-like instruments. The surface of the interdental septa is freed from areas of bone that have undergone destruction. At the same time, the wound is irrigated with a stream of medicinal substance through thin tubes attached to the curettes. If gingivotomy was performed before vacuum curettage, gum flaps are placed along the incision line and fixed with glue.
Cryocuretage in periodontics it is used in the presence of periodontal pockets up to 5-7 mm deep with abundant granulations, hypertrophic gingivitis, hypertrophic gingivitis, papillitis. Contraindication: gum erosion.
In Nikitin's apparatus during evaporation liquid nitrogen a vapor-liquid jet is formed, which flows out of the needle and cools the gum tissue. In modern devices, the refrigerant is cooled by cryozoid without coming into direct contact with the tissues. Cryodestruction occurs at a temperature of minus 60-140°C when using nitrogen and minus 170-178°C when using medical oxygen.
Before curettage, tartar and damaged tooth cement are removed, selective grinding and anti-inflammatory treatment are carried out.
Cryodestruction is carried out in the area of the 3rd-4th teeth in one visit. Exposure time 8-9 s. The gum is moved away from the tooth, and the tip of the device is inserted to the bottom. After 2-3 days, you can perform repeated cryodestruction. The gum pocket is freed from necrotic masses after 2-4 days. Regeneration occurs in 6-12 days. In the first days after surgery, the pockets are washed with antiseptic solutions and no bandages are applied. On the 4th day, proteolytic enzymes are injected into the pockets on turundas in an isotonic solution for 15-20 minutes. On the 5-6th day, therapeutic dressings are applied to stimulate healing (methyluracil in an oil solution of vitamin A) for 2-3 hours.
The patient must carefully observe oral hygiene.
Electrosurgical treatment. Currents are used to carry it out high frequency- diathermocoagulation.
High frequency currents have a bactericidal effect. The operation is bloodless and there is no postoperative pain.
Indications for use this method is gingival fibromatosis, hypertrophic gingivitis, periodontitis with a pocket depth of 3 mm, periodontal abscesses. Disadvantages of this method: healthy areas of the gums can also be coagulated, and not just granulation tissue; An overdose can cause burns that deform the gums.
Gingivotomy - dissection of the periodontal pocket and its curettage, involving removal granulation tissue, removal of epithelial vegetation, necrotic tissue of the alveolar bone.
Indications: narrow, deep, one-sided periodontal or bone pocket (more than 5-7 mm) in the area of one or more teeth, single recurrent periodontal abscesses.
For gingivotomy, incisions are used various shapes: vertical along the tooth axis; from the axis of the tooth to the interdental papilla; interradicular, not reaching the edge of the gum. Most often, a semicircular incision is used at a distance of 3-4 mm from the gum edge. The convex part of the cut faces the apex of the root. This incision is the most gentle and most adequate for subsequent manipulations; it ensures rapid regeneration of damaged tissue.
Main stages of gingivotomy: antiseptic treatment of the oral cavity, infiltration or conduction anesthesia, dissection of the periodontal pocket, curettage, application of guide sutures (sutures are not applied to the lateral areas).
Disadvantages of gingivotomy: retraction of the gingival margin, limited indications, insufficient visibility of the surgical field.
 |
| Rice. |
Postoperative care: In the first 2-3 days, the patient is prescribed weak antiseptic solutions daily for hygienic treatment of the operated area. If there are stitches, they are removed on the 5-6th day after surgery. Probing of the periodontal pocket is contraindicated for 3 weeks. The patient is recommended to carefully observe hygiene: in the first 5-6 days, clean the mouth without using a toothbrush, often rinse the mouth with antiseptics, and a gentle diet.
Gingivectomy. Gingivectomy - excision of the gum edge. By volume surgical intervention distinguish between simple and radicular. The purpose of the operation is to excise periodontal pockets to their full depth.
Indications for gingivectomy: the presence of periodontal pockets more than 4 mm deep, when the underlying bone tissue retains normal shape and the zone of attached gum is quite wide; hypertrophic gingivitis, gingival fibromatosis.
Gingivectomy is contraindicated in cases of deep bone pockets reaching the apical region and in cases where the gingival attachment zone is narrow.
A simple gingivectomy is performed as follows. After anesthesia, the depth of the pockets is measured with a special probe and marked with dots on the alveolar process. A horizontal incision is made 1 mm above the marked points on the vestibular and lingual sides. The gum edges are removed and curettage is performed under visual control.
 |
| Rice. (scheme) |
To avoid excessive exposure of bone tissue, the gum is excised at an angle to the surface of the alveolar process. A gum bandage is applied to the wound. Maintaining postoperative period the same as after curettage.
Removal of gingival papillae can be done using a diathermocoagulator.
When cryodestructing gingival papillae, a cryoprobe is inserted into the gingival groove and the device is turned on for 3-10 s; After thawing, the cryoprobe is removed. Cryonecrosis occurs within 24-48 hours, and regeneration of the damaged area occurs after 6-12 days.
Management of the postoperative period during cryosurgery has important. Protective medical dressings after surgery are not applied during the first 2-3 days, until rejection of the necrotic part of the gum occurs. In the first days, careful oral care is necessary. To accelerate lysis, proteolytic enzymes with antibiotics are prescribed, after rejection of necrotic tissues - medicinal substances that stimulate metabolic processes and gum regeneration (solcoseryl, mundisal-gel, oil solutions vitamin A and vitamins A + E, carotoline, sea buckthorn oil). After cryosurgery, the wound heals 2-3 times slower than when using other techniques; scar change tissues and, as a result, exposure of the necks of the teeth and hyperesthesia. After surgical treatment There may be relapses; after cryodestruction, relapses are rare.
At radicular gingivectomy not only periodontal pockets are excised, but also the alveolar process is partially leveled. The surgical technique is similar to that of a simple gingivotomy, only a horizontal incision is made 2 mm below the designated pocket depth.
Part of the gum is removed after horizontal or several arc-shaped incisions. This exposes the bone and partially bone pockets. The altered bone tissue is removed with a milling cutter, bur or curettage spoon, smoothing and leveling the alveolar edge, granulations and remains of tartar are removed. A gingival bandage or iodoform turunda is applied to the wound surface.
Disadvantage of Gingivectomy- exposure of the necks of the teeth.
Postoperative care: In the first few hours after surgery, bleeding may occur from the wound at the gum edge. Therefore, food intake is allowed only after a few hours. The gum bandage is removed after 24-48 hours. Subsequently, warm astringent rinses with decoctions of chamomile, sage, and oak bark are prescribed. You can rinse your mouth with dental elixirs. During a visit to the doctor, the patient undergoes a local application of carotolin, rosehip oil, methyluracil and other agents that promote epithelization and faster healing.
"A practical guide to surgical dentistry"
A.V. Vyazmitina






