Urethritis is an inflammation of the mucous membrane urethra(urethra), which serves to remove urine from the body. In men, the urethra is also a conduit for sperm.
In most cases, urethritis is caused by urogenital infections and conditionally pathogenic microorganisms(subject to decreased immune status or impaired barrier function of local immune factors).
Much less commonly, urethritis is caused by exposure to chemicals or trauma.
Inflammation that begins in the urethra, if not adequately treated, can spread and affect the bladder and other pelvic organs. This disease affects both men and women, regardless of age.
Especially at risk are young men 20-35 years old who are active sex life, and neglecting means of protection in the form of condoms, as well as men who practice anal sex.
Classification of urethritis
Below is a classification of urethritis, which is based on the etiology of urethritis and its origin.
Urethritis of sexual origin
Venereal (caused by naturally occurring sexually transmitted diseases and not found in healthy people microorganisms):
Chlamydia;
- Trichomonas;
- ureaplasma;
- herpetic ( primary infection virus herpes simplex 2 types).
Conditionally venereal:
Caused by pathogenic pathogens of non-venereal infections accidentally entering the urethra (candidal, bacterial, entamoeba, etc.);
- Caused by opportunistic microorganisms that usually live as saprophytes on the mucous membrane of the oropharynx (Neisseria non gonorrhoeae, gen. Mimeae, etc.);
- Gardnerella (due to Gardnerella vaginalis?) and caused by group B streptococci.
Urethritis of non-sexual origin
Infectious - urethritis, which arose secondarily during common infections or local infectious and inflammatory diseases (chronic prostatitis, etc.), as well as dysbacterial urethritis (candidal and bacterial).
Non-infectious:
Traumatic (from exposure to mechanical, chemical and thermal irritants);
- due to metabolic disorders (phosphaturia, oxaluria, uraturia);
- allergic;
- congestive;
- due to a tumor in the urethra;
- dermatous (symptomatic).
Causes of urethritis
The causative agents of the disease are bacteria and viruses. Often the cause of inflammation of the urinary tract is E. coli, as well as infections that cause sexually transmitted diseases (chlamydia, gonorrhea).
TO viral reasons may include cytomegalovirus and herpes simplex virus.
Chronic urethritis - a pathological condition that develops in the urinary tract as a result of Not proper treatment, or in its absence. In this case, periodic outbreaks are replaced by remissions. The long course of the disease leads to undesirable consequences: adhesions develop in the urethra, its lumen narrows, and associated complications arise.
G
onococcal urethritis.
This is an inflammation that occurs as a result of sexual contact with a partner who has gonorrhea.
The causative agents of gonococcal urethritis (in 80% of cases) are gram-negative intracellular diplococci.
Patients with gonococcal urethritis have a shorter incubation period than those with non-gonococcal urethritis, and they develop symptoms such as dysuria and purulent discharge.
Nongonococcal urethritis (NGU). The disease usually begins with dysuria or, less commonly, with mucopurulent discharge. Sometimes NGU is asymptomatic, unlike patients with gonococcal urethritis.
The pathogens are not G onococcal urethritis (15-55% of cases) are ureplasma, fungi of the genus Candida, chlamydia, trichomonas, etc. Often, the causative agents of the disease cannot be identified in the majority of patients with NGU.
Rare cases of NGU are associated with lymphogranuloma venereum, herpes simplex, syphilis, and mycobacteria. To others, more rare reasons include anaerobes, adenovirus, cytomegalovirus and streptococcus.
Intermittent catheter use can also cause NGU in 2-20% of patients. As practice shows, latex-based catheters are 10 times more likely to cause infection than silicone ones.
Urethritis of mixed etiology usually caused by gonococcal infection and other microorganisms in combination. The cause may be inadequate treatment and some other factors, such as:
Sexually transmitted diseases (gonorrhea, syphilis, chlamydia, herpes simplex virus or AIDS. Mycoplasma genital;
- Bacteria and other microorganisms located at the entrance to the urethra;
- Simple herpes;
- Adenovirus;
- Injuries in women during sexual intercourse;
- Reiter's syndrome;
- Escherichia coli;
- Sensitivity to spermicides or contraceptive jellies, creams, foams, etc.
If the patient has undergone medical procedures using foreign objects (for example, a catheter) in the urethra, then the cause of inflammation is most likely injury.
Causes of urethritis in men
Chemical irritation from soap, lotion, or cologne can cause temporary pain in the urethra. Spermicide in condoms, birth control gels, contraceptive creams or foams may also cause irritation.
- Mechanical manipulation of the penis or minor trauma can lead to urethritis. Medical procedures, uncomfortable clothing, vigorous sexual activity, or masturbation may cause temporary urethral irritation.
- Sometimes ejaculation causes a feeling similar to urethritis. As a rule, it goes away in a short period without any special treatment.
Risk factors for urethritis
The main risk factors for the development of urethritis include:
Reproductive age;
- Disorderly sex life;
-
Anal sex;
- Repeatedly recurring venereal diseases.
Symptoms urethritis
Urethritis regardless of etiological factor appear the same clinical symptoms with varying degrees of severity depending on the type of process. Although certain urethritis have their own clinical characteristics, for example, with trichomonas urethritis, the discharge has a characteristic “smell of fresh fish.” Depending on the type of process, the following are possible: acute form, subacute, torpid form (asymptomatic).
The symptoms of uncomplicated urethritis are summarized by the presence of discharge from the urethra (purulent, mucous, mucopurulent in nature), inflammatory changes in the external opening of the urethra, leukocyturia in the first portion of urine, pain, burning, and cramps of varying severity during urination.
Typically, signs of the disease begin to appear within 4 days to 2 weeks after exposure to an infected partner or may be asymptomatic. Here are the most frequent symptoms diseases:
- Discharge from the urethra. The discharge may be yellow, green, brown or with a hint of blood.
- Urinary disorder (dysuria). Difficulty urinating usually occurs in the morning and can be aggravated by alcohol consumption. Frequent urge to urination and urgency, as a rule, are absent, and they are associated rather with signs of prostatitis or cystitis.
- Pain. Men sometimes complain of a feeling of heaviness in the genitals. Testicular pain may indicate epididymitis, orchitis, or both.
- Menstrual cycle. Women sometimes experience worsening symptoms during their periods.
Simple urethritis usually does not cause fever or significant worsening physical condition. If complications occur, when the disease spreads to other organs of the genitourinary tract or the infection enters the blood, following symptoms:
Back pain;
- Abdominal pain;
- High temperature;
- Nausea;
- Vomit;
- Swelling of the joints.
Characteristic symptoms of urethritis in men:
Blood in urine or semen;
- Sometimes fever;
- Frequent urination;
- Acute pain when urinating (dysuria);
- Feeling of pain, itching or swelling in the groin area;
- Discharge from the penis.
Characteristic symptoms of urethritis in women:
Pain in the lower abdomen;
- Burning pain when urinating;
- Sometimes fever and chills;
- Vaginal discharge;
- Frequent urination;
Diagnosis of urethritis
The study involves passing the following tests:
Complete blood count (CBC);
- Test for C-reactive protein;
- Urine analysis and culture for pathogenic cultures;
- For women - pregnancy test and ultrasound of the pelvic organs;
- Identification tests venereal diseases- chlamydia, gonorrhea, etc.
The doctor will examine skin, the nature of the lesions of which may indicate other sexually transmitted diseases.
Women undergo an abdominal and pelvic examination, including a complete gynecological examination, including the cervix.
A man's medical examination includes:
Inspection of linen for the presence of discharge;
Examination of the penis: The doctor examines the skin for patterns of lesions that may indicate other STDs (for example, genital warts, herpes simplex, syphilis).
Examination of the urethra: The doctor will examine the distal urethra to look for a stricture (an abnormal narrowing of the urethra) or obvious discharge from the urethra; palpating along the urethra, determining the area of fluctuation (fluid accumulation) or abscess.
Examination of the groin area and testes: The doctor will try to identify the presence of inflammation, swelling, and tenderness to rule out diseases such as orchitis or epididymitis. The examination also includes a digital rectal examination.
In addition, when you see a doctor, you need to honestly answer some questions that are important for making a correct diagnosis and subsequent treatment.
Sexual contacts: the doctor will tactfully ask about your sex life, this is necessary to identify the nature and differentiate the disease.
Contraceptive use: In some patients, the use of spermicides can cause chemical urethritis, causing the same symptoms as infectious urethritis.
Age at first sexual intercourse: With the exception of some religious groups that encourage marriage and monogamy at a younger age, many young people have a strong correlation with contracting an STD at first sexual intercourse.
Sexual preferences: Homosexual men have the highest rates of sexually transmitted diseases. They are followed by patients leading a promiscuous sex life.
Treatment urethritis
The goal of treatment is:
Elimination of symptoms;
- Preventing the development of complications;
- Eliminating the cause of the infection.
Most cases of urethritis are caused by infection, and treatment often requires the use of antibiotics. It must be remembered that inadequate treatment with antibiotics can contribute to the progression of the disease to chronic form.
The choice of drug for treatment and its dose completely depend on the cause of urethritis, so prescribing drugs yourself without first consulting a doctor is very dangerous.
Antimicrobial therapy may include the following drugs:
Erythromycin 500 mg (used 4 times a day for at least 7 days, allowed during pregnancy).
- Tetracycline 500 mg (used 4 times a day - at least 7 days).
- Doxycycline 100 mg (used twice a day - 10 days).
- Ciprofloxacin 500 mg (used once a day).
- Ofloxacin 400 mg (used once a day).
- Clindamycin 300 mg (used orally 2 times a day - for at least 7 days).
- Ceftriaxone 250 mg (used once a day).
- Acyclovir 400 mg (used orally 3 times a day - for at least 10 days).
- Famciclovir 250 - 500 mg (used orally 2 times a day - for at least 10 days).
- Metronidazole 2 g (used orally once daily, contraindicated during pregnancy).
Drugs that can also be used:
Clotrimazole is an antitrichomoniacal, antifungal and antibacterial effect;
- Fluconazole (Diflucan) – in case of infection with a fungus of the genus Candida;
- Nystatin (Mycostatin) – when infected with a fungus of the genus Candida;
- Nitrofurantoin – for bacterial infections;
- Co-trimoxazole - combination drug, including sulfamethoxazole and trimethoprim - for bacterial infections.
The course of antibiotic treatment can last up to 14 days. In severe cases of the disease and complications that arise, hospitalization is required.
In cases of infection with sexually transmitted diseases, it is extremely important to use antibiotics regularly. In this case, all sexual partners must undergo treatment.
Having sex without using condoms is unacceptable during treatment.
You should tell your doctor immediately if your condition worsens or symptoms return while taking antibiotics.
It is recommended to drink plenty of fluids to dilute the urine. This will reduce pain when urinating.
Nonsteroidal anti-inflammatory drugs such as ibuprofen and acetaminophen (Tylenol) are used for pain relief.
The use of sitz baths is recommended to relieve irritation caused by chemical urethritis. To do this, fill the bath warm water, so that it covers the genital area, but it is not recommended to use foam or other bath products. Do this procedure several times a day.
Acupuncture procedures are also useful in strengthening the body's immune system and relieving pain from urethritis.
Nutrition and nutritional supplements for treatment urethritis
Appropriate nutrition, use of herbs, homeopathic remedies, as well as acupuncture treatments can be effective in fighting infection, relieving pain, and strengthening the urinary system. Always tell your doctor about the herbs and supplements you use.
The following tips may help reduce urethritis symptoms:
Consume foods with high content antioxidants, including fruits, berries and vegetables (such as blueberries, cherries, pumpkin, tomatoes, bell peppers).
- Try to eliminate potential food allergens. This may require you to take a test to check your food sensitivities.
- Limit your consumption of red meat, give preference to leaner varieties of meat; fish or beans are also good for protein.
- If possible, exclude refined foods such as white bread, sugar, pasta.
- Using healthy edible oils such as olive or vegetable oil is important.
- Reduce or eliminate the use of commercial bakery products(cookies, cakes, crackers, French fries, donuts, margarine) due to their trans fatty acid content.
- Try to completely stop drinking coffee, tobacco, alcoholic drinks and other stimulants.
- Drink at least 5 - 8 glasses of filtered water per day.
- Don't forget to do physical exercise.
The following additions to your diet may also be helpful:
Shortage nutrients and vitamins in the diet can be replenished by taking a daily multivitamin containing antioxidant vitamins A, C, D, E, vitamins and minerals such as selenium, zinc, magnesium and calcium.
- Use probiotic supplements (containing Lactobacillus acidophilus), 5 - 10 billion CFU (colony forming units) per day, to improve the functioning of the gastrointestinal tract and strengthen the immune system. Probiotic supplements must be refrigerated before use.
- Eat omega-3 fatty acids, helping to reduce inflammation and strengthen the immune system. They are found, for example, in fish such as salmon and halibut. A good option is to use fish oil - 1 - 2 capsules (1 tablespoon) 1 - 2 times a day. Fish oil also helps enhance the effect of some blood thinning medications.
- It is useful to use grapefruit seed extract in the form of 100 mg capsules, which helps strengthen the immune system and has antibacterial and antifungal activity.
- Methylsulfonylmethane 3000 mg twice a day is also used to reduce inflammation.
You can use natural hormone replacement therapy to treat chronic urethritis. Consult your healthcare provider.
Herbs for the treatment of urethritis
Herbs are relatively in a safe way strengthening the tone of all body systems. They can be used in any form, capsules, powders, extracts, tinctures, infusions, teas, etc.
Cranberry. Useful action Cranberry juice or fruit drink has an effect on the genitourinary system. You can also buy standardized cranberry extract in pharmacies.
Green tea. Has antioxidant, immunomodulatory, antitumor effects green tea. However, it is best used without caffeine-containing products.
- "Cat's claw." Antibacterial, antifungal and immunostrengthening and antitumor effect possesses "Cat's Claw", sold in the form of a standardized extract. It is necessary to take into account the fact that Cat's Claw may react with other medications, so when using it, you should consult a doctor.
Bearberry. Bearberry is effective for the treatment of genitourinary diseases. It has a diuretic, anti-inflammatory, antimicrobial effect. Also helps thin the blood.
Complications urethritis
With correct diagnosis and adequate treatment, urethritis usually does not cause any complications.
Characteristic for a man the following complications:
Inflammation of the bladder (cystitis);
- Inflammation of the epididymis (epididymitis);
- Inflammation of the testicles (orchitis);
- Inflammation of the prostate (prostatitis);
- Inflammation of the kidneys.
The following complications are typical for women:
Bladder infections (cystitis);
- Kidney infections;
- Cervicitis;
- Inflammation of the pelvic organs (uterus, fallopian tubes or ovaries).
In addition, urethritis can lead to irreversible damage to the urethra, narrowing of its lumen, and cause infertility.
Prevention urethritis
There are simple rules that allow you to maintain health genitourinary system and prevent infection:
Maintain good personal hygiene;
- practice safe sex life with one sexual partner;
- avoid using products that may cause irritation in the genital area: soap, lotion, cologne, vaginal deodorants and aerosols;
- drink more fluids;
- wear cotton underwear.
For women during menopause replacement therapy estrogen may help prevent urinary tract infections.
Inflammation of the walls of the urethra (urethra). Signs include pain, stinging and burning when urinating, pathological discharge from the urethra, the nature of which depends on the causative agent of the disease. In complicated cases, the inflammatory process progresses and neighboring organs pelvis: prostate, bladder and scrotal organs. Another consequence of urethritis is a narrowing (stricture) of the urethra or its complete adhesion. An important point Diagnosis of urethritis is to determine its etiology. For this purpose, it is carried out bacteriological examination urine and urethral swab. Treatment of urethritis is carried out in accordance with its cause (antibiotics, metronidazole, antimycotic drugs), with the development of adhesions, bougienage of the urethra is indicated.

General information
– inflammation of the wall of the urethra. Usually has an infectious nature. It extremely rarely develops without the presence of an infectious agent (radiation, toxic, allergic urethritis). Sometimes the cause of the disease is injury during a diagnostic or therapeutic procedure (catheterization of the bladder in men, administration of drugs, etc.).
Infectious urethritis is divided into two large groups: specific and nonspecific. A specific inflammatory process in the urethra is caused by pathogens of sexually transmitted diseases (gonococcus, trichomonas, chlamydia, ureoplasma, mycoplasma). The cause of the development of nonspecific inflammation of the urethra is opportunistic flora (staphylococcus, streptococcus, fungi, Proteus, E. coli).
There are primary and secondary urethritis. With primary inflammation of the urethra, the infection penetrates directly into the urethra, most often through sexual contact with a partner who has a sexually transmitted disease. Secondary urethritis occurs when infection spreads from an inflammatory focus located in another organ (pelvic organs, seminal vesicles, bladder, prostate gland).

Bacterial urethritis
The cause of the development of nonspecific inflammation of the urethra is a conditionally pathogenic flora. Microorganisms penetrate the urethra during long-term catheterization of the bladder in women and men, transurethral endoscopic manipulation or sexual contact with a casual partner.
- Primary bacterial urethritis
There are acute and chronic bacterial urethritis. The course of an acute nonspecific inflammatory process differs from the clinical picture of gonorrheal urethritis. The length of the incubation period may vary. Local signs of inflammation are not so pronounced. Characterized by pain when urinating, itching, burning, purulent or mucopurulent discharge, slight swelling of the urethral mucosa and tissues surrounding the external opening of the urethra.
It must be remembered that based on the clinical picture and the nature of the discharge, it is impossible to carry out differential diagnosis bacterial and gonorrheal urethritis. The diagnosis is made only upon receipt of data laboratory research, confirming the absence of gonococci: culture for the presence of gonorrhea, PCR diagnostics, etc.
Chronic inflammation of the urethra usually has few symptoms. There is slight itching and burning when urinating, scanty mucous discharge and high resistance to therapy. The short and wide urethra in girls and women allows infection to easily enter the bladder, causing cystitis, which is diagnosed by ultrasound of the bladder. In men, chronic urethritis in some cases is complicated by colliculitis (inflammation of the seminal tubercle). Seminal tubercle - exit site excretory ducts prostate and vas deferens. Its inflammation can lead to hemospermia and ejaculation disorders.
- Secondary bacterial urethritis
The infectious agent enters the urethra from the local source of infection (in pelvic organs, bladder, prostate, seminal vesicles) or with an infectious disease (angina, pneumonia). Secondary nonspecific urethritis is characterized by a long latent course. Patients complain of mild pain when urinating, scanty discharge from the urethra of a mucopurulent nature, more pronounced in the morning. Children often have no pain when urinating. On examination, hyperemia and gluing of the sponges of the external urethral opening are revealed.
When conducting a two- or three-glass test, the first portion of urine is cloudy and contains a large number of leukocytes. In the second portion, the number of leukocytes decreases, and in the third, as a rule, it corresponds to the norm. To preliminary determine the nature of the microflora, a bacterioscopic examination of the discharge from the urethra is carried out. To clarify the type of infectious agent and its sensitivity to antibacterial drugs, a culture of the discharge or urethral wash is performed.
- Treatment of bacterial urethritis
Modern urology has effective methods of treating nonspecific urethritis. Treatment tactics are determined depending on the type of pathogen, the severity of symptoms, and the presence or absence of complications. The combination of urethritis with cystitis is an indication for complex therapy. For a chronic nonspecific process, taking antibacterial drugs is supplemented by instillation of solutions of collargol and silver nitrate into the urethra, measures are taken to normalize the immune system. The result of therapy for secondary urethritis is largely determined by the effectiveness of treatment of the underlying disease (urethral stricture, vesiculitis, prostatitis).
Gonorrheal urethritis
As a rule, it develops as a result of sexual intercourse with an infected partner, less often - through indirect contact through towels, sponges, linen, chamber pots. The reason for the development of infection in children may be living together with an adult patient or using a shared toilet.
- Symptoms and clinical course
The first symptoms of the disease appear 3-7 days after infection. In some cases, it is possible to increase the incubation period to 2-3 weeks. Depending on the duration of the infection, acute (disease duration less than 2 months) and chronic (disease duration more than 2 months) gonorrhea is distinguished.
Acute gonorrheal urethritis usually begins suddenly. There appears abundant yellowish-gray purulent creamy discharge from the urethra, pain, burning and pain when urinating. When the inflammatory process is localized in the anterior urethra, the patient's condition is satisfactory. The spread of inflammation to the posterior part of the urethra is accompanied by hyperthermia up to 38-39 ° C and general signs of intoxication. Pain when urinating becomes more pronounced.
Chronic gonorrheal urethritis develops:
- in patients with untreated or incompletely cured acute inflammation of the urethra of gonococcal etiology;
- in patients with weakened immune systems;
- when the prostate and posterior part of the urethra are involved in the inflammatory process.
The chronic inflammatory process is characterized by mild symptoms. Patients are concerned about itching and slight burning in the urethra. The onset of urination is accompanied by a mild tingling pain. Discharge from the urethra is scanty, mucopurulent, mainly in the morning. Examination of smears indicates the presence of gonococci and secondary microflora.
In chronic gonorrheal urethritis, the ducts of the paraurethral glands are often involved in the process. Inflammation impedes outflow, leading to blockage of the ducts, the development of infiltrates, abscesses and encysted cavities. The patient's general condition worsens, with sharp pain when urinating.
- Diagnosis
Microscopy of urethral discharge is performed. The diagnosis is confirmed by the presence of gonococci (Neisseria gonorrhoeae) - gram-negative bean-shaped aerobic diplococci. The standard examination consists of two stages and includes staining using the Gram method and brilliant green (or methylene blue).
- Differential diagnosis
Diagnosis is usually not difficult due to the presence of characteristic symptoms (pain during urination, purulent discharge from the urethra). Conducted differential diagnosis gonorrheal urethritis and inflammation of the urethra of another etiology (Trichomonas, non-specific urethritis, etc.). The diagnostic criterion is the results of bacterioscopic examination. The history reveals the presence of sexual contact with patients with gonorrhea.
- Treatment
Treatment of gonorrheal urethritis is carried out by venereologists. Recently, increasing resistance of gonorrhea pathogens to penicillin has been observed. The greatest effectiveness is observed when taking cephalosporins and fluoroquinolones. The patient is recommended drinking plenty of fluids. Alcohol, fatty and spicy foods are excluded from the diet.
Chronic gonorrheal urethritis is an indication for combination therapy. The patient is prescribed antibacterial drugs and local treatment. When growing granulation tissue and cellular infiltration (soft infiltrate), solutions of collargol and silver nitrate are instilled into the urethra. If cicatricial-sclerotic processes predominate (hard infiltrate), bougienage of the urethra is performed with metal bougies. Severe granulations are cauterized once a week with a 10-20% solution of silver nitrate through the urethroscope.
- Cure criteria
7-10 days after completion of treatment, a bacterioscopic examination of the urethral discharge is performed. If gonococci are not detected, a combined provocation is performed: biological (pyrogenal or gonovaccine intramuscularly) and chemical (injection of 0.5 solution of silver nitrate into the urethra). Mechanical (anterior urethroscopy or bougie insertion into the urethra), thermal (warming with inductothermic current) and nutritional (drinking alcohol and fatty foods) provocation are also used.
Then, every day for three days, prostate secretions, urine streams and smears from the urethra are examined. In the absence of leukocytes and gonococci, the provocation is repeated after 1 month. After another month, a third and final control study is carried out. If there are no clinical manifestations, and gonococci are not detected by culture and bacterioscopy, the patient is removed from the register. Acquired immunity does not develop with gonorrhea. A person who has had gonorrheal urethritis in the past can become infected again.
- Forecast
With proper, timely treatment of fresh gonorrheal urethritis, the prognosis is favorable. When the process becomes chronic and complications develop, the prognosis worsens. Gonococcal endotoxin has a sclerosing effect on the tissue of the urethra, which can lead to the formation of strictures (usually multiple) in the anterior part of the urethra. Frequent complications of chronic inflammation of the urethra with gonorrhea are vasiculitis, epididymitis, chronic prostatitis. The outcome of prostatitis can be impotence, the outcome of epididymitis can be infertility as a result of cicatricial narrowing of the vas deferens.
Trichomonas urethritis
- Symptoms and diagnosis
Symptoms of Trichomonas urethritis appear 5-15 days after infection. Characterized by mild itching, moderate whitish foamy discharge from the urethra. The diagnosis is confirmed by the detection of trichomonas (Trichomonas vaginalis) in native and stained preparations. Examine urethral discharge, urethral scraping or centrifuge of the freshly released first portion of urine. In native preparations, the movements of Trichomonas flagella are clearly visible.
Often, when studying the native drug (especially in men), motile Trichomonas cannot be detected. The reliability of the study can be increased by using additional methods(microscopy of stained smears, culture examination).
- Treatment
Specific anti-trichomonas drugs are used, the most effective of which are metronidazole, ornidazole and tinidazole. The treatment regimen depends on the patient’s condition, the severity of symptoms, the presence of complications and concomitant sexually transmitted infections. Self-medication is unacceptable, as it can contribute to the transition of an acute process to a chronic one.
In order to prevent re-infection, the patient's regular sexual partner is simultaneously treated. During therapy and for one to two months after its completion, the patient is recommended to drink plenty of fluids and exclude spicy foods and alcohol from the diet. For resistant chronic inflammation, both general and local therapy are prescribed. For 5-6 days, the patient is given instillations of a 1% solution of trichomonacid for 10-15 minutes.
In some cases, trichomoniasis in men is asymptomatic or accompanied by extremely scant symptoms. Patients are often unaware of their disease and spread the infection to their sexual partners. In 15-20% of cases with chronic trichomonas urethritis, prostatitis develops, worsening the patient’s condition and making treatment more difficult.
Chlamydial urethritis
A number of serotypes of Chlamydia trachomatis act as infectious agents. Chlamydia is located intracellularly, which is typical for viruses, but the presence of certain features (DNA, RNA, ribosomes, cell wall) allows these microorganisms to be classified as bacteria. Amazing epithelial cells urethra, cervix, vagina and conjunctiva. Transmitted sexually.
Chlamydial urethritis is usually sluggish and asymptomatic. The inflammatory process in the urethra is in some cases accompanied by joint damage and conjunctivitis (urethro-oculo-synovial syndrome, Reiter's disease). The diagnostic criterion is the presence of semilunar intracellular inclusions in a colored scraping from the urethra.
Treatment. Problems in the treatment of chlamydia are associated with insufficient permeability cell membranes for most antibiotics. Repeated manifestations are typical after courses of treatment. To increase effectiveness, broad-spectrum antibiotics are combined with corticosteroid drugs (dexamethasone, prednisolone). The maximum dose of prednisolone is 40 mg/day, the course of treatment is 2-3 weeks. During the course of therapy, the dose of hormones is gradually reduced until complete withdrawal.
Candidiasis urethritis
The causative agent is yeast-like fungi. Inflammation of the urethra of fungal etiology is rare and is usually a complication after long-term treatment antibacterial drugs. Sometimes it develops after sexual contact with a woman who suffers from candidiasis vulvovaginitis. The risk of infection increases with a history of inflammatory diseases or damage to the urethra.
Candidiasis urethritis is characterized by mild symptoms. Patients complain of a slight burning sensation, mild itching, and scanty whitish discharge from the urethra. Microscopy in an acute process reveals a large number of yeast-like fungi. In case of chronic inflammation, mycelium threads predominate in the sample. Therapy consists of discontinuing antibacterial drugs and prescribing antifungal agents(nystatin, terbinafine, fluconazole).
Inflammation of the urethra is considered one of the most unpleasant and at the same time common diseases. In medicine, this phenomenon is called urethritis, and it is not a life-threatening condition, but its symptoms cause severe discomfort and interfere with a person’s normal lifestyle.
Causes of the disease
According to statistics, the majority of patients are men, but urethritis in women, unfortunately, is also quite common. Often people independently diagnose themselves and begin treatment, but the problem is that this disease is very similar to cystitis.
A significant difference between the second is the pain that accompanies the entire process of urination and may not last long after its completion. However, these two diseases often occur simultaneously.
Causes of inflammation:
- Reduced immunity;
- Hypothermia;
- Kidney stones;
- The presence of sexually transmitted diseases, sexually transmitted infections;
- Poor nutrition;
- Malignant tumors of the urethra;
- Allergy;
- Venous congestion in the pelvis;
- Early sexual intercourse;
- Failure to comply with hygiene rules;
- Injuries to the genital organs;
- Alcoholism;
- Psycho-emotional overload, stress;
- Pregnancy.
Symptoms of urethritis in women
Often, the symptoms of the disease in females are less pronounced than in males. This is due to the difference in the structure of the genitourinary system. In men, the urogenital canal is narrower and longer, so they are more susceptible to inflammatory processes of various etiologies.
The most common signs of the disease are:
- Pain and burning during urination;
- Discharge of pus from the urethra. The color of the discharge directly depends on the pathogen, ranging from dark yellow to whitish;
- Redness of the external genitalia;
- Itching during menstruation.

With chronic urethritis, rare pain in the lower abdomen occurs, this applies not only to the period of exacerbation. Most often, in females, the pathology occurs without pronounced symptoms, so its diagnosis is sometimes complicated.
The disease becomes chronic if there is no treatment, or with incorrect and untimely therapy. After about three weeks, the acute form may become chronic. The main symptoms disappear and appear only after hypothermia, alcohol abuse, strong psycho-emotional arousal and at the time of sexual intercourse.
Urethritis has infectious and non-infectious origin. The most common is gonorrheal urethritis, which is sexually transmitted. Its signs appear through infection. Another common cause is chlamydia.
Non-gonorrheal forms of the disease
These include trichomonas and candidiasis urethritis.
Infection first occurs both through sexual intercourse (with unprotected intercourse) and by everyday means(carious teeth, tonsillitis, chronic sinusitis, tuberculosis, etc.). Symptoms of acute Trichomonas urethritis in women include the appearance of whitish foamy discharge one to two weeks after infection, as well as itching in the urethra.
But often this form occurs hidden. Treatment of trichomonas urethritis usually involves the use of metronidazole (Trichopol) for 8-10 days.
Candidal urethritis occurs when the canal is damaged by yeast fungi of the genus Candida. This form The disease is quite rare and occurs mainly due to long-term use of antibacterial agents in the treatment of other pathologies. Once the diagnosis is confirmed, antibiotics are stopped.
The first manifestations of pathology occur at the onset of menopause, menstruation, or the abolition of oral contraceptives. The doctor decides how to eliminate inflammation, guided by diagnostic indicators and the picture of the disease of a particular patient.
Diagnostics
During the examination, the doctor may detect hyperemia of the external opening of the urethra and surrounding tissues, and discharge from the urethra. The patient feels pain on palpation.
The following activities are required:
- General analysis of urine and blood;
- Extended study of urine according to Nichiporenko;
- Bacteriological analysis, which will allow you to accurately determine the type of etiological pathogen; at the same time, a test is carried out for its sensitivity to antibiotics;
- Analysis of bacteriological material (scraping from the walls of the urethra) using the PRC method;
- Study of urine for Mycobacterium tuberculosis.
Sometimes ureteroscopy is performed - endoscopic examination urethral mucosa, which allows you to take scrapings, eliminate scars and strictures. An ultrasound examination may also be prescribed to assess the general condition of the pelvic organs.
Treatment of urethritis in women

After diagnosis, antibacterial agents such as ciprofloxacin, pefloxacin, amoxiclav, and norfloxacin are prescribed. Antibiotics are mainly prescribed in tablet form, but other options are also available: intravenous and intramuscular injections, intravaginal suppositories and installations (infusion of a substance through a catheter into the urethra). They may prescribe either one type of antibiotic or a combination of two, three or even four drugs.
Procedures such as baths and rinses using calendula, chamomile, and potassium permanganate help to get rid of discomfort. Purely feminine remedies include warming applications, tampons impregnated with anti-inflammatory and antibacterial substances, and vaginal suppositories.
Medicines for acute urethritis in women include antihistamines, for example, the most common are Miramistin, Tavegil and Suprastin. If chlamydia is detected at the same time, azithromycin and doxycycline are prescribed.
How to get rid of pathology
Antibiotics and anti-inflammatory drugs cannot completely get rid of the disease, especially those caused by viruses and fungi. It is necessary to simultaneously increase the body’s resistance to such infections, restore normal microflora female genital organs.
Therefore, the doctor prescribes stimulants immune system: thymalin, Gepon, cycloferon, phlogenzyme, antioxidants, ribomunil, PP and B vitamins.
Treatment of the chronic form is a longer process. Antibiotics such as chloramphenicol and gentamicin are often prescribed for chronic urethritis in women. The sooner you start therapy, the faster the positive effect will occur.
The duration of treatment varies in each individual case and can last several weeks. Antiseptic urethral lavages and vitamin and mineral supplements are also prescribed.
If the causative agent is a gonococcal infection, an antibiotic is installed in the urethra. In the presence of granulation, installation with a solution of silver and collargol is used, as well as bougienage and cauterization of the urethra with a solution of silver nitrate (10-20%), but only with severe narrowing.
The chronic chlamydial form is treated with antibiotics and immunomodulators, probiotics, interferon preparations, enzyme therapy, hepatoprotectors (for the liver), vitamin therapy, and antioxidants.
TO non-drug methods disease control includes:
- Diet;
- Drink plenty of boiled water or freshly squeezed juice - about 2 liters per day;
- Subsequent proper nutrition with the exception of spicy, fatty, sour and salty foods.
is a disease characterized by the manifestation of an inflammatory process in the urethra. The most striking signs of urethritis are pronounced painful sensations during urination, as well as the appearance of discharge from the urethra. This disease is diagnosed in patients of both sexes.
Types of urethritis
Urethritis is an infectious disease, therefore, its development occurs due to exposure to an infectious agent. These may be viruses , mushrooms , bacteria etc. Also in especially rare cases, diseases occur radial , toxic , allergic urethritis and some other types of it.
Depending on which pathogen causes urethritis to develop, there are two types: different types diseases: urethritis specific And nonspecific . In the first case, the occurrence of specific urethritis is provoked ( chlamydia , gonococcus , trichomonas , ureaplasma etc.) Such infections can be combined with the effects of other viruses, fungi, bacteria, and there may be several infections in the body. In this case, the disease is complicated by the fact that, as a rule, a person does not record when acute stage the disease becomes chronic.
Nonspecific urethritis occurs due to exposure to opportunistic microflora. Its occurrence is provoked staphylococci , streptococci , coli , fungi etc. The disease in both cases develops and manifests itself almost identically. But it is very important to take into account that if a sexually transmitted infection is detected, all sexual partners of the patient must undergo examination and treatment.
Features of urethritis
As a rule, the manifestation of specific urethritis occurs after sexual intercourse. However, it happens that a person becomes infected while certain time becomes a carrier of infection. In this case, the disease can manifest itself at any time. Nonspecific urethritis may also occur as a result of sexual contact.
The cause of the development of the inflammatory process in the urethra is a failure of the immunity of the canal wall. The urethra is constantly infected, infection occurs through the blood, from the intestines, from the skin, and from other places. Particularly severe infection occurs during sexual intercourse. Therefore, as long as the wall of the urethra can cope with the infection, the disease will not develop. But at the slightest malfunction of the protective mechanisms, an inflammatory process occurs, which is accompanied by all the accompanying symptoms.
There are a number of factors that often become predisposing during the onset of the disease. First of all, urethritis in men and women can occur as a result of one-time or constant hypothermia. The occurrence of urethritis is influenced by the presence of a person. When sand or stone moves along the urethra, it is quite possible that injuries to the walls and the subsequent occurrence of urethritis may occur. Penile injuries that are too severe predispose to the disease physical activity, irregular sexual activity. However, too much sexual activity and frequent change partners can also trigger the development of the disease. It is not recommended to eat spicy foods too often, as well as over-salted, sour foods, pickled vegetables, large quantity alcohol. When substances from such foods enter the urine, they irritate the wall of the canal. As a result, inflammation may occur or progression of an existing disease may occur.
A provoking factor in the manifestation of urethritis is often insufficient drinking: irregular urination provokes the retention of bacteria in the body, because it is urine that washes them away from the wall of the bladder. With a several-hour break between urinations, the risk of developing inflammation increases markedly. Urethritis can also occur against the background of chronic inflammation that occurs in the body.
Thus, there are quite a lot of factors that can subsequently become decisive in the development of urethritis. Therefore, this disease can occur in anyone.
Symptoms of urethritis
 Already at the very beginning of the disease, pronounced symptoms of urethritis appear: severe pain and stinging, burning sensations and itching when urinating. Also, during the process of urination, a person may feel any other discomfort. Similar sensations occur in the genitals and perineum.
Already at the very beginning of the disease, pronounced symptoms of urethritis appear: severe pain and stinging, burning sensations and itching when urinating. Also, during the process of urination, a person may feel any other discomfort. Similar sensations occur in the genitals and perineum.
Another important symptom Urethritis is the appearance of discharge from the urethra. They can be of varied nature. So, depending on what pathogen provoked the urethritis, the discharge can be very abundant or very scanty. During an exacerbation of the disease, the edges of the external hole may become inflamed and stick together. However, in some cases, the development of urethritis is not accompanied by discharge at all.
With each subsequent exacerbation of the disease, inflammation affects an increasingly significant part of the mucous membrane of the urethra. Therefore, the symptoms of urethritis become more pronounced with each exacerbation. Therefore, if the disease is not treated with adequate methods, complications of urethritis may occur.
If we consider the symptoms of urethritis from the point of view of their manifestation in each type of disease, then some differences in the clinical picture are noticeable.
Thus, with acute urethritis in men and women, the main symptoms are severe burning and pain during urination, the presence heavy discharge from the urethra, swelling and noticeable redness of the lips of the urethra. With torpid urethritis, subjective disorders are observed. They do not appear clearly, in some cases they are completely absent.
In the case of subacute urethritis, pain and swelling in the urethra decrease, and the amount of discharge also decreases. Only in the morning does a crust sometimes appear, gluing the external opening of the urethra. The urine is clear and may contain purulent threads.
For chronic urethritis, which manifests itself as a result of an incorrect approach to treatment or complete absence Thus, neurotic phenomena are possible. Most often, with this form of urethritis, small ones are present. They become more abundant subject to the presence of certain factors that provoke an exacerbation of the disease. This could be heavy drinking, agitation, or hypothermia. Symptoms of chronic urethritis are often similar to those torpid urethritis .
Total urethritis is characterized by inflammation of the urethra as a whole. The symptoms of this form of the disease are similar to those. It is important to take into account that in the absence of therapy, the symptoms of urethritis may disappear on their own. However, with each subsequent exacerbation of the disease, its symptoms will be even more pronounced. As a result, the patient may experience serious complications of urethritis.
Diagnosis of urethritis
 For proper treatment, it is necessary, first of all, to correctly establish the diagnosis. First of all, the doctor tries to find out what reasons provoked the occurrence of urethritis in the patient. Thus, to identify the causative agent of the disease, various laboratory tests are used (smear, DNA diagnostics, PCR). Often, the doctor prescribes an ultrasound examination of the pelvic organs to adequately assess their condition. Based on the results obtained, the patient is prescribed a specific therapy.
For proper treatment, it is necessary, first of all, to correctly establish the diagnosis. First of all, the doctor tries to find out what reasons provoked the occurrence of urethritis in the patient. Thus, to identify the causative agent of the disease, various laboratory tests are used (smear, DNA diagnostics, PCR). Often, the doctor prescribes an ultrasound examination of the pelvic organs to adequately assess their condition. Based on the results obtained, the patient is prescribed a specific therapy.
Treatment of urethritis
In order for the treatment of urethritis to be as effective as possible, it is necessary, first of all, to determine what infection provoked the inflammatory processes of the urethra. In the treatment of urethritis, the same treatment regimens are used as in the treatment , and a number of other diseases of the reproductive system. Various drugs are used to combat pathogenic microorganisms. First of all, this , as well as agents with antifungal and antiviral effects.
It is important that treatment of urethritis occurs in parallel in both sexual partners due to high probability transmission of infection during sexual intercourse.
Both specific and nonspecific urethritis are treated using the same principles. Similar classification important from the point of view of the specific selection of drugs for the treatment of urethritis, as well as for understanding whether there is a need to treat the patient’s sexual partner.
If a patient is diagnosed with a combination of urethritis and cystitis, then an integrated approach to treatment is important. In this case, the doctor must prescribe the use of physiotherapeutic procedures, as well as instillations medicines into the bladder and urethra. The treatment process can last several days or several weeks: it depends on the severity of the disease.
The correct approach to treatment on the part of the patient is also important. Not only drug treatment is effective, but also compliance with the doctor’s prescription. , abstinence from alcohol, drinking plenty of fluids.
After the course of therapy is completed and all symptoms of the disease have disappeared, you should mandatory Carry out tests again to monitor the patient's condition. This will help ensure that the infection has been eradicated.
Doctors
Medicines
Prevention of urethritis
As a measure to prevent urethritis, it is important to adhere to a healthy diet, excluding an abundance of spicy, salty, sour foods, and alcoholic beverages from the diet. Important and correct drinking regime: Every day a person should drink enough fluid. The best option is to drink plain still water. If necessary, you can use diuretics - linden tea, cucumber, blackcurrant and cranberry juice, and parsley are suitable for this.
You should also avoid hypothermia, wear warm and comfortable clothes in winter, avoid bowel problems, and carefully monitor genital hygiene. If you have symptoms of inflammation, you should immediately contact a specialist to treat the disease at an early stage.
Complications of urethritis
In the absence of the necessary treatment, urethritis in men can be complicated by a number of phenomena. First of all, acute urethritis can become chronic. Possible development of inflammation of the prostate gland ( prostatitis ), testicular inflammation ( orchitis ), inflammatory process of seminal vesicles ( vesiculitis ). Due to urethritis, it can also develop , balanoposthitis , possible narrowing of the urethra.
With urethritis in women, it is possible as a complication disturbance of vaginal microflora , Vinflammatory phenomena of the urinary tract .
List of sources
- Urology: national guide / ed. N.A. Lopatkina. - M.:GEOTAR-Media, 2009;
- Kozlyuk V.A., Kozlyuk A.S. Urethritis in men. Current issues in diagnostics. Cytomorphology. Treatment. - Kyiv: Style-Premier, 2006;
- Skriprin Yu.K., Sharapova G.Ya. Sexually transmitted diseases. - M.: Medicine, 2005;
- Molochkov V.A. Sexually transmitted infections. Clinic, diagnosis, treatment / V.A. Molochkov, O.L. Ivanov, V.V. Chebotarev. M.: Medicine, 2006.
Urethritis is an inflammatory process that is located in the urethra. This disease is very common, and the pathology develops regardless of the age and gender of the patient. In order to clearly understand what urethritis is in a man, what are the symptoms and methods of treating this pathology, it is necessary to clearly understand the anatomy of the male urethra.
Anatomical features and structure of the male urethra
The outlet of the bladder is the beginning of the urinary canal, which in medical and scientific circles is commonly called the urethra. This is a small-diameter reproductive tube, which has a length of 16 to 24 centimeters. It is worth noting that the female urethra is only 4 centimeters long. Exactly like this comparative characteristics and are the main reason for differences in the manifestations of urethritis in representatives of different sexes, respectively, if in women urethritis can pass without visible pathological symptoms, then in males the disease has very intense symptoms and can manifest itself soon after direct infection and the development of the inflammatory process.
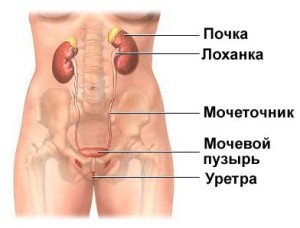
The male urinary canal consists of the following sections:
prostatic department. This is part of the urethra, which is located in the prostate gland and is about 4 centimeters long. The prostatic section is also called prostate;
membranous section. Also called membranous. Its length is 2 centimeters. The beginning of the department is behind prostate gland, and ends at the base of the penis. This space of the male urethra is the narrowest;
spongy section, or spongy. It is the longest section of the urinary canal and is located inside the shaft of the penis. Compared to the membranous and prostatic, the spongy section is characterized by mobility. This section of the urethra ends with an outlet called the meatus.
Classification of urethritis
The clinical picture and methods of therapy depend on the type of infectious agent that caused the inflammation, the stage of neglect and intensity of the disease, the presence of concomitant diseases and provoking factors. That is why the prescription of effective and adequate treatment depends on the nature of the pathology.
|
Classification of urethritis according to etiological indicators |
|
|
Non-infectious urethritis |
Infectious urethritis |
|
Non-infectious diseases include: congestive urethritis - may appear due to venous stagnation in the pelvis; traumatic urethritis - appears against the background of ruptures and tears of the urethra, as well as after surgical interventions(catheterization, cystoscopy); allergic urethritis - develops due to exposure to allergens. |
Each type of infectious urethritis has its own specific type of pathogen, and only with mixed urethritis can inflammation occur against the background of the action of two or more pathogenic organisms: tuberculous; mixed; gardnerella; chlamydial; ureaplasmic; mycotic; bacterial; trichomonas; viral; mycoplasma; Trichomonas. |
|
Classification according to severity of symptoms |
Classification according to the characteristics of the disease |
|
Chronic urethritis is divided into periods without exacerbations and the acute stage: low-active urethritis; moderate degree of disease activity (urethritis); high degree of inflammation of the urinary canal. |
Fresh urethritis is divided into: torpid; subacute; |
|
Classification by disease specificity |
Classification according to the characteristics of the onset of the disease |
|
specific – these are sexually transmitted infections (chlamydia, trichomoniasis, gonorrhea) and tuberculosis; nonspecific - the causative agent of the infection is microorganisms that are constantly present in the body, but are suppressed by a healthy immune system. |
primary – the disease occurs as an isolated pathology; secondary – develops due to the presence of other diseases in the body. |

In most cases, the causative agents of urethritis are chlamydia and gonococci, while in approximately 50% of cases these infectious agents cannot be detected when examining the material.
Symptoms of urethritis
After direct infection of the body, symptoms of urethritis appear after some time, and the time period from the moment of infection to the first signs of pathology directly depends on the incubation period of the pathogen. For allergic urethritis it is several hours, for tuberculosis - several years, for viral - several months, for candidiasis and trichomoniasis - two to three weeks, for chlamydial - 7-14 days, for gonorrheal - 3-7 days.
Most typical symptoms male urethritis are:
the presence of characteristic discharge that appears from the urethra;
burning, itching and pain when urinating.

Other symptoms characteristic of STDs, by type general weakness and hyperemia, is not observed with urethritis. However, the nature of the discharge can be different and depends on the type of pathogen that caused urethritis. In most cases, green or white discharge appears with unpleasant smell, against which yellow crusts may form on the penis. The discharge is most noticeable in the morning.
In addition, along with the discharge, redness and sticking of the external opening of the urethra may be present. Pain in the lower abdomen can occur regardless of the type of urethritis, but even they are not constant symptom pathology.
The process of urination is also disrupted, which in the initial stage is often accompanied by cloudy urine and pain, and at the same time the number of daily urges to urinate increases. The end of this process may be accompanied by sharp pain and sometimes blood.
If the disease has become chronic, then the symptoms of the disease may disappear altogether, there will be no discharge, and the patient may only be bothered by mild itching and discomfort in the urethral area. More pronounced symptoms are observed only during periods of exacerbation of the disease.
With bacterial urethritis, purulent discharge is observed, with trichomoniasis - whitish, with gonorrheal urethritis - gray-yellow or greenish. Also, the discharge may be insignificant or completely absent, but the man will be bothered by blood in the semen or urine, burning and itching during urination, swelling of the penis, and pain during sexual intercourse.

The table shows the most characteristic symptoms of urethritis for its different types.
|
Non-infectious urethritis |
|
|
Traumatic urethritis |
Symptoms depend on the nature of the injury - burning and pain when urinating. |
|
Allergic urethritis |
Also pain and burning, however, a feature is the presence of allergic edema. |
|
Congestive urethritis |
Classic symptoms are often completely absent. It manifests itself in different types of sexual dysfunction. |
|
Infectious urethritis |
|
|
Tuberculous urethritis |
In most cases, it occurs against the background of renal tuberculosis or genital tuberculosis. Mycotic tuberculosis bacteria penetrate into the urethra through urine flow. It is asymptomatic (sweating, increased fatigue, low-grade fever). |
|
Gardnerella urethritis |
Incubation period from one week to several months. In most cases, it is present as a component of mixed urethritis. |
|
Chlamydial urethritis |
There are no stinging or burning sensations, slight discharge. In most cases it occurs chronically. |
|
Ureaplasma urethritis |
Most often accompanied by trichomoniasis or gonorrheal urethritis. The incubation period is about 1 month. There is green or white discharge, burning and itching when urinating. Symptoms worsen due to sexual intercourse or alcohol consumption. |
|
Mycotic urethritis |
The incubation period is about 20 days, there is burning and itching. The discharge is watery or mucous, sometimes pale pink in color. |
|
Bacterial urethritis |
Purulent discharge. The symptoms are erased. The incubation period can last several months. |
|
Trichomonas urethritis |
Different constant itching in the area of the head of the penis, the presence of grayish-white discharge and difficulty urinating are also characteristic. |
|
Viral urethritis |
The course of the pathology is sluggish, the symptoms are mild. May be accompanied by conjunctivitis or joint inflammation |
|
Mycoplasma urethritis |
Quite rarely occurs in isolation. In most cases it is combined with gonorrheal or trichomonas urethritis. |
|
Gonorrheal urethritis |
Gray-yellow discharge from the urethra, acute pain at the time of urination. The pus contained in the urine gives it a cloudy color. Blood impurities appear in semen and urine. |

Treatment of urethritis in men
The choice of treatment for urethritis, like any other disease, is made based on diagnostic data. First of all, laboratory test results are used. A general blood and urine test, urethroscopy data, examination of urethral smears, bacteriological culture urine.
Treatment procedures can be carried out on an outpatient basis; during treatment it is important to be systematic and accurate in following medical instructions; hospitalization is not necessary. If the intake of antimicrobial drugs is interrupted, carried out irregularly, or the patient drinks alcohol during therapy, the disease threatens to become chronic.
It is quite obvious that the selection of drugs for drug treatment male urethritis is carried out by a doctor, and the patient must comply with necessary rules: drink plenty of fluids, do not consume pickled, smoked foods, spices, herbs, avoid alcohol, observe personal hygiene rules, exclude sexual activity.

The selection of medications is carried out purely individually. Any infectious urethritis is treated with antibiotics. The most pronounced effect is achieved when using an antibacterial drug selected on the basis of a sensitivity test. It is thanks to this research that it is possible to select the most effective remedy for treatment.
Treatment of bacterial, gonorrheal urethritis
Antibiotics of the cephalosporin group demonstrate excellent results in the treatment of gonorrheal urethritis. In addition to them, kanamycins, oletethrins, erythromycins, and tetracyclines can be prescribed. In this case, kanamycins must be used with extreme caution, since these drugs are highly toxic. Long-acting drugs - bicillin-5 and bicillin-3 - should be prescribed in short courses. In some cases, if gonorrheal urethritis is complicated by other infections, simultaneous use of several antibacterial drugs is practiced. In such cases, it is best to use the complex “Gentamicin” and “Azithromycin” (“Ecomed”, “Hemomycin”, “Azitrox”, “Azicide”, “Z-factor”, “Sumamed”).

In order to prevent the occurrence of candidiasis due to prolonged antibiotic therapy, Levorin, Fluconazole, Nystatin, Pimafucin and other antimycotic drugs are prescribed. The most important aspect treatment is an individual selection of drugs. Quite often, men who suffer from gonorrheal urethritis ask friends to “prick” and use antibiotics uncontrollably and without consulting a doctor. Such self-medication is unacceptable, since long-term use of strong anti-inflammatory drugs without a clear treatment plan and control of cure can lead to the transition of urethritis to a chronic form and the development of resistance of the pathogen to drugs.
In addition to antibiotics, the patient should take immunostimulating drugs and vitamins. To be completely sure that the body has freed itself from gonococcus and is completely cured, it is necessary to take control smears three times. Only after receiving negative results studies, we can assume that the patient is completely healthy.
Gardnerella, ureaplasma and mycoplasma urethritis
These types of urethritis are treated with the antibiotics lincosamines, fluoroquinolones, macrolides and tetracyclines. The tetracycline group, specifically doxycycline, is considered the most effective. A group of macrolides (clarithromycin) also gives excellent results. Immunostimulants are also prescribed.

For any specific urethritis, it is necessary to carry out simultaneous therapy for both sexual partners.
Trichomonas urethritis
If a man is diagnosed with trichomonas urethritis, when selecting drugs, they turn to metrogil, trichopolum and metronidazole. If urethritis is chronic, antibiotic therapy is added to treatment. In case of inadequate treatment, infertility may develop.
Candidal urethritis
Treatment of candidal urethritis in men requires a completely different approach. The main drugs to combat this pathology are antimycotic drugs, such as Pimafucin, Nystatin, Clotrimazole, Fluconazole. High-quality treatment of the underlying disease, which is the cause of candidal urethritis, is important.
Chlamydia urethritis
The only antibiotic that actively fights the causative agent of this infection is azithromycin. If you choose the wrong drug for chalmydia urethritis, serious complications can occur - inflammatory diseases, epididymitis, Reiter's syndrome, infertility. If the patient has an individual intolerance to azithromycin, the following alternatives are used: doxycycline, levofloxacin, erythromycin, ofloxacin, clarithromycin. Immunostimulating drugs and vitamins should also be used in combination.
Viral urethritis
Treatment is carried out with antiviral drugs. The sooner treatment is started, the faster the recovery will occur. Among antiviral drugs, preference is given to: “Gerpevir”, “Famciclovir”, “Riboverine”, “Acyclovir”. It is not advisable to use antibiotics for this form of pathology, since they are not able to fight viruses.
Nonspecific chronic urethritis
Treatment of nonspecific chronic male urethritis is not as fast as for infectious ones. Chronic course the disease is quite often aggravated associated pathologies, and signs of the disease are mild or may be absent altogether. Therefore, therapy for chronic urethritis should begin with taking immunostimulants. Only this approach makes it possible to activate the body’s defenses to fight infection. After receiving the result, antibiotic therapy is selected individually. Main feature Treatment of nonspecific forms of urethritis is the absence of the need to treat the sexual partner.

Non-infectious urethritis
For allergic urethritis it is necessary to use antihistamines. If urethritis is caused by stagnation of blood in the pelvic area (congestive), it is necessary to eliminate the cause of this stagnation. For traumatic urethritis, in addition to antimicrobial therapy, surgical intervention may also be required.
Antibiotics may be prescribed for:
installation of the drug through catheter administration into the urethra;
intravenous infusions in 0.2% of cases of acute urethritis;
intramuscular injections in 18%;
oral administration in 81%;
use of only one antibiotic - monotherapy 41%;
two – 41%;
three – 13%;
four antibiotics – 5% of cases.
The most popular antibiotics for acute male urethritis, which are prescribed by a doctor depending on the type of pathogen
|
Trichomonas urethritis in combination with atypical agents |
Gonococcal urethritis |
Mixed urethritis |
|||||
|
"Ornidazole" |
"Doxycycline" |
"Josamycin" |
|||||
|
"Josamycin" |
"Ciprofloxacin" |
"Ceftriaxone" |
|||||
|
"Azithromycin" |
"Metronidazole" |
"Ornidazole" |
|||||
|
"Doxycycline" |
"Azithromycin" |
"Secnidazole" |
|||||
|
"Metronidazole" |
"Ceftriaxone" |
"Fluconazole" |
|||||
|
"Doxycycline" |
|||||||
|
"Azithromycin" |
|||||||
|
Non-gonococcal urethritis, which is caused by atypical agents |
Urethritis of unknown etiology |
||||||
|
"Clarithromycin" |
"Clarithromycin" |
||||||
|
"Secnidazole" |
"Ciprofloxacin" |
||||||
|
"Josamycin" |
"Tinidazole" |
||||||
|
"Metronidazole" |
"Nimorazole" |
||||||
|
"Doxycycline" |
"Josamycin" |
||||||
|
"Ofloxacin" |
"Secnidazole" |
||||||
|
"Fluconazole" |
"Fluconazole" |
||||||
|
"Azithromycin" |
"Ceftriaxone" |
||||||
|
"Doxycycline" |
|||||||
|
"Metronidazole" |
|||||||
|
"Azithromycin" |
|||||||

Additional treatments
In addition to the basic course of treatment with antibacterial drugs that suppress the acute symptoms of the disease, other therapeutic methods are also widely used, which relate to local and physiotherapeutic procedures.
Local procedures involve the injection of medications directly into the opening of the urethra. Urethral installations are performed using the drug hydrocortisone, Dioxidin and Mirimistin. Local treatment gives good results when used in combination with other drugs.
Physiotherapeutic treatment is used exclusively in cases chronic urethritis, use these methods for acute inflammatory processes is strictly contraindicated. Magnetic therapy, laser therapy, UHF, electrophoresis may be prescribed. However, all these methods should be carried out only systematically and only under the supervision of specialists.
Causes of urethritis in men
sexually transmitted infections are the most common cause urethritis in men who are sexually active. If sexual intercourse is performed without the use of barrier contraception, then the likelihood of pathogen penetration into the urethra is very high;
urolithiasis - found much more often in men than in women. This disease causes traumatic urethritis, due to the fact that stones, moving along the genitourinary tract, actively injure the mucous membrane and lead to the attachment of pathogenic microorganisms;
any injury to the penis and heavy physical activity can cause the development of urethritis;
hypothermia is one of the most important provocateurs of exacerbations chronic diseases(including extrapulmonary tuberculosis, viruses, infections), since in this case the protective functions of the body are significantly reduced;
general decrease in immunity - smoking, alcohol abuse, overwork, lack of sleep, poor nutrition leads to natural exhaustion protective forces body;
medical manipulations (catheterization of the bladder, smear) - carry the risk of injury to the mucous membrane of the urethra, and urethritis can develop if the necessary disinfection measures are not followed;

nutrition - an abundance of sour, spicy, salty foods leads to irritation of the mucous membranes, which contributes to the addition of infection. Lack of fluid causes rare urination; therefore, the genitourinary tract does not naturally flush out harmful microorganisms that may accidentally enter the urethra.
Prevention of complications of urethritis
Statistics say that every second man on the planet after 50 years has prostatitis. Do not think that prostatitis can directly cause urethritis. However, quite often the occurrence of prostatitis occurs against the background of active infectious diseases genitourinary system. Urethritis can cause the development of Reiter's syndrome, infertility, sexual dysfunction, colliculitis, balanoposthitis, orchitis, vesiculitis. In order to minimize the risk of complications of urethritis, a man should:
avoid excessive and intense physical activity;
do not get carried away with salty, spicy, fatty foods, alcohol;
empty the bladder at the first urge to urinate, try to “tolerate” less;
avoid hypothermia;
promptly treat any chronic pathologies;
lead a decent sex life, observe the rules of intimate hygiene.





