V treatment practice infectious patients used a huge number etiotropic agents. This is due to the fact that highly pathogenic strains of pathogens appear and their drug resistance to antibacterial drugs occurs, as well as changes in the resistance of the macroorganism and secondary immunodeficiency. For correct application medicines and obtaining the desired results, one must have knowledge of the properties of drugs, adhere to the fundamental principles of the domestic science of treatment infectious diseases. Without this, it is difficult for a practitioner to navigate in a variety of antibacterial agents and in various methods their applications. The main provisions of the treatment of patients with infectious diseases, from the point of view of the clinician, were formulated by A.F. Bilibin (1958). The greatest attention was paid not only to the choice of antibiotic, the method of its administration, but also, which is especially important, to the infectious process, which is subject to three factors: "causative agent, macroorganism and environment."
At present, advances in microbiology and achievements in pharmacokinetics make it possible to choose antibiotics with a pronounced antimicrobial effect and a “narrow” focus, which reduces the risk of dysbacteriosis.
V this section general and particular provisions on the use of antimicrobial agents are presented. In contrast to the already published information [Yu. V. Lobzin et al., 1998] this work additionally presents the undesirable effects of the interaction of antibacterial drugs and other drugs, as well as clinical aspects antibiotic therapy infectious patients.
At present, in addition to data on the effectiveness of chemotherapy drugs, their increasing cost is of some importance, which can often affect the choice of antibiotic.
Fulfillment of basic application requirements antibacterial agents set out in the Guide is intended to promote successful treatment infectious patients.
Antibacterial agents significantly affect the course and outcomes of most infectious diseases. So complex treatment infectious patients should be directed primarily to the causative agent of the disease. The purpose of drugs is justified by the etiology of the disease, its pathogenesis, taking into account the physiological characteristics of the organism, the severity and period of the disease.
For influence on the pathogen chemotherapy and antibiotic therapy. Chemotherapy refers to antimicrobial, antiparasitic treatment using chemical substances. This term was introduced to fundamentally distinguish antimicrobial therapy from pharmacotherapy in general. The essence of antibiotic therapy is the treatment with drugs natural origin produced by microorganisms; this treatment is aimed at suppressing the growth or killing of disease-causing microbes in infectious diseases. Many modern antibiotics are semi-synthetic, i.e. created by modifying the original molecule.
The first of the antimicrobials in clinical practice sulfanilamide (1936) was used. A little later, in 1941, at Oxford University, A. Fleming obtained and successfully used penicillin for the first time. Today, the number of natural, semi-synthetic and synthetic antibacterial drugs is measured in the thousands. However, in practice, only dozens of antibiotics can be used, which are low toxic and, at the same time, have a pronounced antibacterial effect. A large number of antibiotics due to the diversity of pathogenic and opportunistic bacteria.
Classification of antibiotics.
The modern classification of antibiotics was developed at the State Center for Antibiotics [S. M. Navashin, 1994], according to which they are characterized by the mechanism of action, chemical structure, antimicrobial spectrum, type of action on the cell.
Based on the mechanism of action, antibiotics are divided into three main groups:
» inhibitors of microorganism cell wall synthesis (penicillins, cephalosporins, vancomycin, teicoplanin, etc.);
» antibiotics that disrupt molecular organization, functions of cell membranes (polymyxin, nystatin, levorin, amphotericin, etc.);
"antibiotics that inhibit protein and nucleic acid synthesis, in particular protein synthesis inhibitors at the ribosome level (chloramphenicol, tetracyclines, macrolides, lincomycin, aminoglycosides) and RNA polymerase inhibitors (rifampicin), etc. The following groups of antibiotics are distinguished by chemical structure: beta-lactams ( penicillins, cephalosporins, etc.), aminoglycosides, chloramphenicol, tetracyclines, fusidine, ansamacrolides (rifampicins), polymyxins, polyenes, macrolides, etc.
Depending on the type of effect on the microbial cell, antibiotics are classified into two groups:
» bactericidal (penicillins, cephalosporins, aminoglycosides,
rifampicin, polymyxins, etc.);
» bacteriostatic (macrolides, tetracyclines, lincomycin,
chloramphenicol, etc.).
For an infectious disease clinician, it is especially important to know the spectrum of antimicrobial action of antibiotics, since it is taken into account when choosing an antibiotic.
By spectrum antimicrobial action antibiotics are divided into the following groups.
1. Drugs acting on gram-positive bacteria and cocci: biosynthetic penicillins, isoxazolpenicillins (oxacillin), lincosamides, vancomycin, fusidine.
2. Antibiotics active against gram-negative bacteria: aztreonam, polymyxins.
3. Antibiotics a wide range actions active against gram-positive and gram-negative bacteria: aminopenicillins (ampicillin), carbenicillin, ureidopenicillins (piperacillin), cephalosporins, aminoglycosides, chloramphenicol, tetracyclines, macrolides, rifamycins, carbapenems (imipenem, morepenem), fosfomycin.
4. Anti-TB antibiotics (streptomycin, rifampicin, florimycin).
5. Antifungal antibiotics (nystatin, levorin, griseofulvin, amphotericin B, ketoconazole, ancotyl, diflucan, etc.).
The above properties basically dictate the choice of antibiotic for the treatment of an infectious patient. In this case, the pharmacodynamics and pharmacokinetics of the drug must be taken into account, individual characteristics patient (age, immune status, concomitant diseases, etc.).
Efficiency treatment with antibiotics with their timely appointment is largely determined by the following factors:
» etiological diagnosis of the disease, clinical diagnosis of nosological forms of an infectious disease, isolation of the causative agent of the disease, followed by determination of its sensitivity to antibiotics;
» selection of the most active and at the same time the least toxic
for a specific patient drug;
» determination of the optimal dose of the antibiotic, the method of its administration to create a concentration in the focus of infection that is 2-3 times higher than the minimum inhibitory concentration (MIC) for this microbe;
» knowledge and consideration of possible adverse reactions for an antibiotic » the use of a combination of drugs, according to appropriate indications, in order to expand the spectrum of their action and / or enhance the antimicrobial effect.
Pharmacokinetics and pharmacodynamics of antibiotics.Pharmacokinetics- a section of pharmacology that studies the pathways of intake, distribution and metabolism medicinal substances in the body and their excretion.
Pharmacodynamics- a section of pharmacology that studies the reaction of organs, tissues or the body as a whole and the magnitude of this reaction in response to the administered drug, as well as the characteristics of the activity of antibiotics in relation to pathogens.
The clinical efficacy of an antibiotic is largely determined by its distribution in organs and tissues, the ability to penetrate the physiological and pathological barriers of the body. It can change with hepatocellular insufficiency, with violation of the excretory function of the kidneys, etc. The fate of antibiotics in the body is determined by their metabolism and the degree of protein binding. precondition for good therapeutic action is also sufficient absorption. In addition, antibiotics undergo enzymatic action (metabolism) in the body, resulting in the formation of inactive and sometimes toxic products.
The process of interaction of the antibiotic introduced into the body with "targets" is divided into three main chronological phases: pharmacoceutical, pharmacokinetic and pharmacodynamic.
In the pharmacoceutical phase, the disintegration of the dosage form occurs due to dissolution, release of the active and active ingredient which becomes available for absorption. As a result of the interaction of antibiotics and chemotherapy drugs with the ingredients of food and digestive juices some drugs may undergo various modifications, including inactivation. The binding of food components with drugs occurs mainly in the gastrointestinal tract, where insoluble or poorly soluble compounds that are poorly absorbed into the blood are formed. Antibiotics of the tetracycline series bind to calcium (including the calcium of milk, cottage cheese and other dairy products), sulfonamides - to food proteins. The absorption of sulfadimethoxine, sulfamethoxypyridazine and other sulfonamides slows down significantly in the first 3 hours after a meal. However, after 6, 8 and 27 hours, the concentration of sulfonamides in the blood becomes the same in everyone who took these drugs both on an empty stomach and immediately after a meal. Under the influence of food, the absorption of tetracyclines, penicillin, erythromycin, rifampicin, chloramphenicol and other drugs decreases quantitatively. Foods rich in iron salts, as well as inorganic iron preparations taken together with tetracycline drugs, cause inhibition of the absorption of these antibiotics, which leads to a decrease in their blood concentration by 50% or more. From this it follows that during the period of treatment with tetracycline it is necessary to refrain from taking iron preparations and food rich in iron salts. Furado-nin, introduced together with fatty foods, lingers longer in the stomach, where it dissolves and decomposes, which leads to a decrease in its concentration in the intestine, and as a result, to a decrease in therapeutic activity. At the same time, food intake does not affect the absorption of cephalexin, levomycetin and other antibiotics.
The recommendations offered in various reference books on the time of taking antibiotics and chemotherapy drugs cannot be unambiguous, but should be used taking into account many points and, in particular, the individual characteristics of the patient, the nature of the disease, functional state digestive system, dosage form and physical and chemical properties medicinal product.
In the pharmacokinetic phase, absorption, distribution, metabolism, and excretion of the drug occur. In this phase, the antibiotic has a biological effect on the pathogen. The phase lasts from the moment the drug appears in the blood until it disappears from it.
With the intravascular administration of an antibiotic, there is direct contact with the pathogen circulating in the blood, faster penetration into the focus of infection. If the antibiotic is administered subcutaneously or intramuscularly, then the rate of absorption is directly proportional to its solubility in water and lipids. At parenteral administration antibiotics, their bioavailability also largely depends on the speed of overcoming barriers, such as, for example, the blood-brain barrier. The permeability of the blood-brain barrier for penicillin, tetracycline, cephalosporins is limited. The concentration of antibiotics may decrease in the foci of infection (sinusitis, abscesses, etc.) due to a decrease in their penetration through inflammatory biological barriers [Yu. P. Finogeev et al., 1976]. In this regard, it may be more effective to administer chemotherapeutic agents and antibiotics directly to the site of infection, for example, in the form of aerosols for respiratory diseases [Yu. P. Finogeev, 1980], in solutions - into the cavity of amoebic liver abscesses [V. M. Volzhanin, 1992].
In the pharmacodynamic phase, the interaction of the antibiotic (chemotherapeutic agent) with the microorganism occurs when a certain biological activity is achieved. The duration of the 3rd phase is from several hours to several days (individual antibiotics and long-acting sulfonamides).
The strength of the drugs (antibiotics) is determined by the following factors:
» a dosage form that ensures the appropriate pharmacoceutical availability of the medicinal substance;
» amount of antibiotic; its integrity in tissues, organ (in the focus of infection), which is due to the rate of its metabolism and elimination.
The time intervals between medications, the duration of treatment also depend on the pharmacokinetics and pharmacodynamics of the drugs. It should always be remembered that any chemotherapeutic agent and antibiotic are foreign to the body, therefore they are sometimes called xenobiotics, and that chemotherapeutic substances are not always indifferent to the macroorganism.
The choice of antibiotic in the treatment of patients with bacterial infections. The main indication for antibiotic therapy of an infectious patient is the presence in the body of such bacterial pathogen, with which the body itself is unable to cope, or in which significant complications are possible. At the same time, the main and decisive factor in the choice of an antibacterial agent is the pathogen and its sensitivity to the chosen drug [V. G. Bochorishvili, 1988].
In most cases, initial antibiotic therapy is carried out empirically. However, prior to prescribing an antibacterial drug, it is necessary to select material (blood, cerebrospinal fluid, mucus from the tonsils, etc.) for bacteriological research, i.e. isolation of the causative agent of the disease and determination of its sensitivity to antibiotics. When establishing a clinical diagnosis of the disease, you can choose the drug that is most effective for this infection ( typhoid fever, pseudotuberculosis, erysipelas, diphtheria, leptospirosis, etc.). Meningitis, pneumonia, sepsis, nosocomial infections and some others pathological conditions can be caused by various pathogens, so after the appointment empirical therapy it is necessary to carefully control the dynamics of the process and conduct repeated bacteriological studies in order to accurately identify the pathogen and, thereby, make antibacterial therapy targeted, taking into account the sensitivity of the isolated microorganism, with preference for drugs with a narrow spectrum of action.
sick in serious condition antibiotic therapy is prescribed urgently, with an unspecified etiology, drugs with a wide spectrum of action are used, in some cases a combination of drugs is used. It is preferable for patients with immunodeficiency to prescribe bactericidal drugs: beta-lactams, aminoglycosides, vancomycin, fosfomycin, fluoroquinolones, etc.
Recommendations for optimal choice antibiotics depending on the etiology of the infectious disease are given in Table. 3, 4 and 5.
Antibacterial agents for the treatment of infectious diseases caused by gram-positive and gram-negative cocci
Table 3
Table 4

The clinician always needs to correlate laboratory data with the clinical course of the disease in dynamics, as well as take into account the possible change of the pathogen and especially the change in its sensitivity to the antibiotic (pneumonia, sepsis, etc.).
It should be pointed out that the sensitivity of pathogens to antibiotics can vary widely in different regions, depending on certain antibiotics used for a long time, on the state of the macroorganism and other factors. The reaction of organs and tissues or the organism as a whole to the administered drug depends not only on chemical features active substance, but also from its interaction with certain reacting organs.
Often in clinical practice infectious disease specialists use combined antibiotic therapy. The main indications for its implementation are as follows:
» mixed infections;
» the need to prevent the development of antibiotic resistance in microorganisms;
» expediency of strengthening the antibacterial effect;
» Insufficient sensitivity of pathogens to monoantibiotics.
The following options for the interaction of antibiotics with their combined use are possible:
» indifferent action - no change in the effect of each of the antimicrobial agents is noted (levomycitin + erythromycin);
» additive action (summation) - the antibacterial effect of the drugs used is equal to the sum of the action of each of them separately, independently of one another (ampicillin + oxacillin);
» synergistic action - effect joint application two antibiotics exceeds the simple summation of the action of each drug separately (betalactams + aminoglycosides);
»Antagonistic action - the effect achieved when several drugs are combined is lower than the effect of each separately (betalactams + tetracyclines).
Antagonistic interaction antibiotics is explained by their mechanism of action on the microbial cell. Betalactams, vancomycin, and fosfomycin act on microorganisms only during mitosis, and therefore, the simultaneous administration of bacteriostatics that disrupt microbial cell division can deprive bactericidal antibiotics of the substrate to which they act. The combination of two bactericidal antibacterial agents is optimal.
When combined various antibiotics bactericidal type of cases of antagonism, as a rule, is not observed. The combination of bacteriostatic and bactericidal drugs sometimes leads to their antagonism.
It is known that the properties of the microflora changed under the influence of antibiotics, the views on the mechanisms of resistance underwent a transformation, and multiple resistance appeared. This complicated the decision to use a combination of different antibiotics. However, in practice, the doctor should not completely abandon the combinations recommended in reference books and manuals. At the same time, a comprehensive consideration of the properties of infectious agents is necessary. However, it should still be borne in mind that monoantibiotic therapy is a priority, in which it is preferable to prescribe drugs with a narrower spectrum of action, especially in cases of prolonged treatment. When prescribing a combination of antibiotics, it is advisable to use their compatibility tables. Under certain conditionality, they will help to avoid unfavorable (decrease in efficiency, etc.) consequences.
Interaction of antibiotics with other drugs. The choice of antibacterial agents is influenced by the features of their pharmacokinetics and pharmacodynamics: penetration through the blood-brain barrier, changes in activity depending on pH.
During treatment bacterial infections with intracellular localization of the pathogen should be taken into account varying degrees penetration of antibacterial drugs into the cell. Aminoglycosides penetrate the cell in small quantities and exhibit low antibacterial activity in it. Macrolides and fluoroquinolones penetrate well into the cytoplasm and vacuoles of cells and have an antibacterial effect on intracellular bacteria. Betalactams penetrate only into the cytoplasm of cells and, with few exceptions, have low intracellular activity.
In case of infections of the central nervous system, it is important that the antibacterial drug penetrate the blood-brain barrier, through which levomycetin, sulfonamides, cotrimoxazole, nitroimidazoles, and fluconazole penetrate well. Penetrate only with inflammation - benzylpenicillin, ampicillin, oxacillin, piperacillin, cefuroxime, ceftriaxone, cefotaxime, ceftazidime, cefpirome, meropenem, aztreonam, amikacin, kanamycin, vancomycin, doxycycline, pefloxacin, ofloxacin, ciprofloxacin.
In the treatment of severe patients, it should be borne in mind that the activity of aminoglycosides in acidosis and hypoxia is reduced.
The route of administration of the drug is determined by its bioavailability, which refers to the part of the drug that, after ingestion, enters systemic circulation in active form.
Antibacterial drugs with a bioavailability of more than 60%: levomycetin, doxycycline, flucloxacillin, aminopenicillins (except ampicillin), enteral forms of cephalosporins, fuzidin, phosphomycin, rifamycins, fluoroquinolones (except norfloxacin), cotrimoxazole, nitroimidazoles should be administered enterally if possible, since high bioavailability ensures the closeness of doses of enteral and parenteral administration of the drug with minimal risk of adverse events, simplicity and cost-effectiveness.
Antibacterial drugs with a bioavailability of 30-60% are more effective when administered parenterally (oxacillin, cloxacillin, ampicillin, lincosamides), used orally with high sensitivity pathogens to them (tetracycline, metacycline, macrolides, phenoxymethylpenicillin, norfloxacin, nitrofurans).
Antibacterial drugs with bioavailability less than 30% - aminoglycosides, ureidopenicillins, injectable forms of cephalosporins, carbapenems, aztreonam, vancomycin are used parenterally. When taken orally, they give only a local effect [I. B. Mikhailov, 1998].
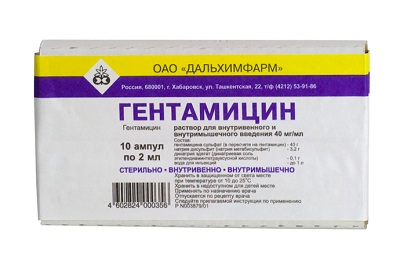
Mode dosing antibiotics (aminoglycosides), the activity of which depends mainly on their concentration (concentration dependent killing drugs), is to create possibly larger peaks in the concentration of the drug in the blood, close to toxic [C. N. Nightingall, 1998]. A single administration of the entire daily dose aminoglycosides, usually by intravenous drip. At the same time, a high peak concentration of the antibiotic ensures maximum destruction of bacteria, lower total toxicity, is more convenient for the patient, medical staff and economical [L. S. Stragunsky, S. N. Kozlov, 1998].
When using antibiotics of the groups of beta-lactams, macrolides and lincosamides, the activity of which mainly depends on the duration of concentration (time dependent killing drugs), it is necessary to constantly maintain the concentration of these drugs in the blood above the level of the MIC between their injections. The frequency of administration of these antibiotics, as a rule, depends on the half-life (Ti / 2), which largely determines the time to maintain the required concentration of the drug in the blood after a single injection. With the introduction of a constant maintenance dose of the drug at the same interval of administration, on average, after 4-5 Ti / 2, its equilibrium concentration is created in the blood plasma. So Ti / 2 benzylpenicillin is 1 hour, so it must be administered every 4 hours. Therapeutic effect from the use of bactericidal antibacterial drugs occurs in 1-2 days, bacteriostatic - in 3-4 days. After this time, the clinical effect of the antibacterial agent is evaluated.
The duration of antibiotic therapy depends on the clinical course. nosological form. In cyclic but recurrent infections (typhus), the antibacterial drug can be canceled 1-2 days after the clinical effect is obtained. In cyclic but recurrent diseases (typhoid fever, pseudotuberculosis) antibiotic treatment continue for as long as the disease would have continued without etiotropic therapy. In acyclic infections, which include sepsis, as well as most diseases caused by opportunistic flora, antibacterial drugs are prescribed in empirically established optimal timing, taking into account clinical recovery.
When treating with antibacterial drugs, it is necessary to keep in mind the secondary resistance of microorganisms. To beta-lactams, tetracyclines, lincosamides, chloramphenicol, vancomycin, fosfomycin, fluoroquinolones, nitrofurans, nitroimidazoles, secondary resistance develops slowly ("penicillin" type of resistance). To aminoglycosides, macrolides, rifamycins, fusidine, 8-hydroxyquinoline derivatives and quinolones I-II generations secondary resistance develops quickly ("streptomycin" type of resistance). Therefore, these drugs should be prescribed for a course of no more than 5-7 days or combined with other antibacterial drugs [I. B. Mikhailov, 1998].
The interaction of antibiotics with other drugs, when used simultaneously, can ultimately have both a positive and a negative result.
So, the drug of choice for the treatment of meningococcal meningitis is, as you know, benzylpenicillin. The required therapeutic concentration of penicillin in the central nervous system usually provided by its use in megadoses (200,000-500,000 IU per 1 kg of body weight per day). At the same time, the optimal daily dose of an antibiotic depends on its combination with various pathogenic agents that can reduce the concentration of penicillin in the cerebrospinal fluid (antagonistic pharmacokinetic effect) or increase it (synergistic pharmacokinetic effect). For example, the combination of penicillin with a complex of synergistic drugs (caffeine with eufillin or baralgin together with furosemide and isotonic solutions) allows you to get the best therapeutic effect in patients with meningococcal meningitis by reducing the daily dose of penicillin by 2 times by increasing its permeability through the blood-brain barrier [K. S. Ivanov, 1982]. At the same time, the antagonistic effect in the treatment of meningitis with penicillin is observed from the use of osmotic diuretics (mannitol, urea), hypertonic solutions, glucocorticosteroids. This is due to increased excretion of penicillin in the urine, a decrease in the permeability of the blood-brain barrier with hormone therapy due to its anti-inflammatory action. However, the joint administration of certain antibiotics (kanamycin) with glucocorticosteroids (hydrocortisone) leads to a longer maintenance of their high concentration in the blood [K. S. Ivanov et al., 1976].
At planning complex etiopathogenetic therapy it is necessary to take into account the mutual enhancement of possible side (undesirable) effects of antibiotics, pathogenetic agents and alcohol. Data on the incompatibility of drugs with antibiotics are given in Table. 6, 7. Combinations of these drugs are not recommended for practical use, since they are more or less unfavorable for patients. Persons at increased risk of side effects of drug combinations with antibiotics include the elderly, as well as those suffering from kidney and liver failure. These patients with infectious diseases, as a rule, receive therapy for concomitant pathology when it is especially necessary to take into account the possibility of interaction of antibiotics, chemotherapy drugs with other drugs. The group of drugs whose combinations with antibiotics must be carefully monitored include anticoagulants, antidiabetic agents, metal salts, diuretics, non-steroidal anti-inflammatory drugs and other drugs.
Evaluation of the effectiveness of antibiotic therapy. In the practice of a clinician, a situation often arises when it is necessary to prescribe antibiotic therapy before determining the final diagnosis of the disease, clarifying its etiology (isolation of the causative agent of the disease and determining sensitivity to antibiotics and chemotherapy drugs). In such cases, the principle of starting antimicrobial therapy is used.
When to use Faringosept?
One of the most commonly used flavors in mouthwash is menthol for the feeling of freshness that goes away. However, the use of menthol in concentrations above 2% is not recommended and its use in cosmetic products in products intended for children under three years of age.
Video about the prevalence and history of the development of antibiotics
Usually used in urinary infections administered as a highly concentrated oral dose. It cancels its function and causes an osmotic imbalance. § Binding to penicillin-fixing proteins. Similarly, they prevent the synthesis of peptidoglycan from the cell wall and cause lysis. § Activates autolysins in the bacterial wall, causing abnormal mitosis and cell death. Penicillins: Penicillin fungus has been found to inhibit growth Staphylococcus aureus. Exploring from there, penicillins were discovered. Molecule of penicillanic acid. The basic chemical structure of penicillin consists of a thiazolidine ring attached to a β-lactam ring to which a side chain is attached. It is a beta-lactamase inhibitor. Esters of penicillin: sultamicillin and thalampicillin. They are very useful against abdominal infections. Third generation cephalosporins. It has an extremely wide spectrum. The only thing that is not affected is mycoplasmas and mycobacteria. It is provided in an aerosol for pulmonary lesion. Carbapenes: They have a penicillin-like structure with different properties from the rest of the β-lactica. Monobactam: β-lacquer, very active, have a β-lactam ring as a core and side chains. An example is aztreonam. They are absorbed into the intestinal tract, so their use is intravenous. They are widely used as a second option in emergencies because they have side effects. Both have side effects. They can cause kidney damage, especially vancomycin, as well as deafness. Teicoplanin acts on anaerobes. They are toxic at both the renal and hepatic levels, as well as at the neurological level, so their main use is ectopic. This only affects Gram - with a thin wall. It is given by aerosol in patients with cystic fibrosis, acting on the bacteria remaining in the cystic fibrosis mucus and reducing it. adverse effects. Polymyxin B: Active in infections against pseudomonas aneurysms. It is excreted from the kidneys and liver and produces side effects, liver toxicity, digestive problems, and some neurological problems. The best known is metronidazole: it is active against protozoa, gram and - but provided that they are anaerobic. They have no side effects and are administered orally with excretion mainly by the liver. The molecule itself has no activity, it is pro-antibiotic. They are small molecules and hydrophobic. They absorb well and easily penetrate organic compartments. - Norfloxacin: in urinary tract infections due to rapid renal excretion. They are very active and have a broad spectrum, being more active against aerobes than anaerobes. They have many side effects. Limiting its use to serious hospital infections. Usually used for infections with intracellular parasites active while they are extracellular. It is used in combination with β-lactica as they have a synergistic effect. They are given oral infections from intracellular parasites. Few side effects to accentuate dentine and bone fixation, causing brittle bones. That's why it's for adults only. It takes longer to inactivate than tetracycline. It is toxic, penetrates well into our cells and attacks mitochondria because they have ribosomes similar to bacterial ones. Mainly for respiratory diseases. It is used in cardiac conditions. It is more active against anaerobes than against aerobes. The activation system is similar to metronidazole. Therefore, drugs that block viral replication also change the functioning of normal cells, and the boundaries between therapeutic doses and toxic doses very narrow. General properties antiviral drugs: - selectivity. Its efficacy and toxicity are related to the immunological competence of the patient. Most of them are ineffective for latent viruses, they are effective only at the stage of virus replication. Therefore, it is only used topically for the skin and cornea. They are bacteriostatic for Gram-positive, Gram-negative and anaerobic bacteria. They also enter effective concentrations in synovial fluid, bone, dentin, tooth enamel also in saliva. The other part is secreted by bile, sweat, tears and breast milk. Gastrointestinal tract: When the agent is administered orally, epigastric discomfort, burning, nausea, vomiting, stomatitis and glossitis occur. Onychilysis and nail pigmentation sometimes occur at the same time. Hypoplasia of tooth enamel. Superinfection Development of resistant bacterial strains or yeasts of opportunistic fungi. The most affected device is gastrointestinal tract, and the most common infection is penicillin candidiasis affecting the fetal wall, requiring a logarithmic growth phase. It does not change when food is swallowed. As a result of changing the flora, it can cause oral or vaginal candidiasis. Toxic effects on newborns In newborns, especially premature babies, the use of chloramphenicol causes a condition known as neonatal gray syndrome. Toxic effects on the newborn. Start days 2 and 9 of treatment with vomiting, elimination of green and soft stools, bloating, anorexia, rapid and irregular breathing, cyanosis. Toxic effects on the newborn They then become lethargic, with hypothermia and a greyish discoloration on the skin. All this clinical picture due to hepatogenic immaturity of infants. The prototype is erythromycin. It is an alternative antibiotic for these microbes. susceptible bacteria. The presence of stomach contents generally delays the absorption of erythromycin. The chemical changes that have been made to these agents make them resistant to their degradation to inactive metabolites like erythromycin. A single dose of azithromycin is sufficient to treat genital infections.
- It is broad spectrum and hydrophilic.
- It can be used as a second option for tuberculosis.
- Bacitracin: Very active against streptococci and gram staphylococci.
- Absorption is greater if there is no stomach content.
- They bind to plasma proteins to varying degrees.
Undesirable effects in the interaction of antibiotics with various drugs (according to V. E. Novikov, 1994)

The main criterion for effectiveness Antibacterial therapy is most often a decrease in the degree of intoxication with a decrease in body temperature. Along with clinical monitoring of dynamics infectious process bacteriological techniques are used - the isolation of the pathogen, the quantitative and qualitative determination of its sensitivity to antibiotics, the comparison of pharmacodynamic and pharmacokinetic indicators.
In the targeted therapy of bacterial infections, it is ideal to use methods bacteriological diagnostics disease and antibiogram knowledge. Only in this way can the right choice be made effective drug among many close on the spectrum of action. This is especially important in connection with the wide distribution of antibiotic-resistant strains of microorganisms.
Susceptibility of microorganisms to antibiotics. Since the discovery of antibiotics, some pathogens of infectious diseases have little changed the nature of the initial sensitivity to these drugs (group A streptococci, pneumococci, meningococci, brucella, some salmonella).
At the same time, most pathogenic microbes eventually acquired resistance to widely, sometimes uncontrolled and unreasonably used antimicrobial agents. Highest value The problem of microorganism resistance has to do with staphylococci, shigella, Escherichia, Proteus, among which antibiotic-resistant strains are isolated with the greatest frequency.
According to the degree of sensitivity to the main antibiotics, microbes are divided into sensitive, moderately sensitive and resistant. The group of sensitive includes most strains of microorganisms, the growth of which on nutrient media stops when using concentrations corresponding to the average therapeutic doses of antibiotics. If it is suppressed when using only the maximum doses of drugs, then such microorganisms are moderately sensitive to the antibiotic. If growth suppression is achieved in a laboratory experiment only at very high concentrations drug that cannot be created in the body, then such infectious agents are resistant to the antibiotic.
To determine the sensitivity of microbes to antibiotics There are a number of methods: the method of serial dilution in liquid nutrient medium or nutrient agar, the method of diffusion in agar, the method of disks saturated with antibiotics and accelerated methods. The disk method is simple, widely used, but gives only a qualitative answer. A more reliable and accurate quantitative method is the method of serial dilution of antibiotics in a nutrient medium under standard experimental conditions. In most cases, the correlation of laboratory data with clinical data is quite complete, and therapy is effective when studied in dynamics, not only clinical course process, but also a possible change in the pathogen or its sensitivity to antibiotics.
The concentration of antibiotics in tissues and body fluids, as well as their antimicrobial activity, are among the main parameters that determine the effectiveness of antibiotic therapy. In its study, microbiological research methods based on the ability of an antibiotic to retard the growth of a test microbe are most widely used. Among the microbiological methods for determining the concentrations of antibiotics in body fluids and tissues, the most widely used are the agar diffusion method and the serial dilution method in a liquid nutrient medium.
At present, microbiological systems for automated and semi-automated identification and assessment of antibiotic resistance have been created, which can significantly speed up bacteriological analysis and increase its accuracy. There are accelerated physicochemical and chemical methods (enzymatic immunoassay, immunofluorescence, etc.) for studying the pharmacokinetics of antibiotics, which help to quickly optimize treatment regimens, individualize them and increase the effectiveness of etiotropic therapy.
When choosing an antibiotic, information on the minimum inhibitory concentrations for individual pathogens should be used, which may be different in relation to both the type of microbe and the different tissues (environments) of the patient's body. In practice, therapeutic activity is achieved by prescribing antibacterial drugs in doses that ensure their higher level in the environments of predominant habitat and pathogens.
Reasons for the lack of effect of antibiotic therapy. The failures of antibiotic therapy are primarily due to the fact that the treatment is carried out without taking into account the sensitivity of the pathogens of an infectious disease to the prescribed drug, while the individual tactics of antibiotic therapy are not followed. In addition, treatment failures may be due to the wrong choice of doses and methods of drug administration, late initiation of treatment, the use of antibiotics in low doses in combination therapy, and insufficient duration of the course. It is not always taken into account the possibility of inactivation of drugs by enzyme systems of the body, their binding by blood and tissue proteins. Even with the proper sensitivity of the pathogen to the antibiotic, unsatisfactory results of treatment are possible due to poor penetration of the drug into the focus of infection due to insufficient blood supply, the formation of a biological barrier (granulation shaft, the presence of fibrin deposits, tissue necrosis, etc.) around the focus of infection, unfavorable absorption conditions in generalized capillary toxicosis.
Currently, there is the concept of "chemotherapeutic resistance of the macroorganism", when the lack of treatment results is not associated with an antibiotic, but is determined by the state of the patient's body, a decrease in its reactivity. Therefore, the use of etiotropic agents must necessarily be combined with active pathogenetic therapy. Antibiotics often do not have a final sanitizing effect in infectious diseases that occur against the background of the use of glucocorticosteroids, cytostatics, with concomitant radiation sickness, etc.
Sometimes there are positive results treatment even if the isolated pathogen is resistant to this drug. This is due to the use of antibiotics (especially benzylpenicillin) in high ("mega") doses, much higher than that established in the laboratory of the IPC.
Side effect of antibiotics. In the process of antibiotic and chemotherapy, it is necessary not only to know well the antimicrobial activity of the drugs used for treatment, but also to be aware of the possibility of their side effects, its pathogenesis, forms of manifestation, prevention and treatment. The side effect of antibiotics and chemotherapy drugs is mainly reduced to allergic, toxic reactions or depends on the side effect of chemotherapy - bacteriolysis reaction, dysbacteriosis, superinfection, etc.
Types of antibacterial agents
Therefore, this definition includes medical pharmacology: the science of elements used in the prevention, diagnosis and treatment of diseases, as well as important role chemicals that are in environment and which cause disease and use certain products chemists as molecular tools for the study of normal biochemistry and physiology. Toxicology is the branch of pharmacology that deals with the adverse effects of chemicals in biological systems.
Clinical manifestations allergic reactions expressed in the form of anaphylactic shock, skin lesions, mucous membranes, Quincke's edema, asthmatic bronchitis.
The manifestation of toxic reactions is characterized by clear symptoms and occurs more often than allergic ones. When taking aminoglycosides, they are characterized by neuritis auditory nerve, defeat optic nerve, vestibular disorders, possible development polyneuritis, toxic kidney damage. Tetracyclines, rifampicin, erythromycin, sulfonamides have a hepatotoxic effect. Chloramphenicol, rifampicin, streptomycin can have a pathological effect on the hematopoietic system. Tetracycline, erythromycin, amphotericin B, etc. have a toxic effect on the gastrointestinal tract.
TO side effect antibiotics, associated with biological activity should include the Jarisch-Herxheimer reaction, infectious-toxic shock, which are caused by the so-called "toxin shock" as a result of massive bacteriolysis. Infectious-toxic shock often develops in infections with intense bacteremia (meningococcemia, typhoid fever, leptospirosis, etc.), especially in cases of using bactericidal antibacterial drugs. The development of shock is prevented by the simultaneous administration of glucocorticosteroids (pulse therapy), infusion-detoxification therapy. For the same reason, the treatment of patients with meningococcemia is recommended to begin with the use of a bacteriostatic drug - chloramphenicol.
Antimicrobial drugs can cause dysbacteriosis, a decrease in the intensity of the body's immune response, which ultimately manifests itself as reinfection or superinfection. Due to suppression normal microflora intestines may develop hypovitaminosis.
The basis for the prevention of adverse reactions from antibiotics and chemotherapy drugs is radical therapy with the knowledge common properties the drug, its mechanisms of action, pharmacokinetics and application regimens.
Microorganisms sensitive to linezolid
A drug is any molecule that, when introduced into the body, alters the function of the body through interactions at the molecular level. Drug interactions with the body are conveniently divided into two classes: pharmacodynamic interactions, the effect of a drug on the body, and pharmacokinetic interactions, the form or mechanisms by which the body processes the drug. The quantitative aspects of pharmacodynamics are the concept of pharmacological receptor and dose-response relationships, while the principles of pharmacokinetics are uptake, distribution, metabolism and elimination.
Antibacterial drugs, or antibiotics, are one of the most commonly used groups of medicines in medicine. Antibiotics are actively used to treat various infectious diseases of a bacterial nature, ranging from common bronchitis, and ending with sepsis of heavy treatment.
In connection with wide application antibacterial agents, very often the question arises of which antibiotic is better?
These pharmacokinetic processes determine the rate, concentration and residence time of the drug in the target organ. The main pharmacokinetic variables are bioavailability, distribution and clearance. Ideal antimicrobial drug is relatively toxic. This term implies that the drug is harmful to the parasite, worse not to the host. In many cases, selective toxicity is relative rather than absolute, meaning that the drug can damage the parasite at concentrations that the host can tolerate.
Types of antibacterial agents
Antibiotics are a group of medicines, different in origin (bacterial, plant, semi- and synthetic nature), capable of inhibiting the growth of bacteria and a number of protozoa.
There are several classifications of antibacterial agents. However, the greatest clinical application found only three.
The goal of antibiotic chemotherapy is to help the host's defenses to control and eliminate microorganisms that are temporarily overwhelmed by the host's defenses. Pharmacodynamics, on the one hand, is a function of the human-drug relationship and the bacteria-drug relationship. On the other hand, the boundaries of antibiotics are certain numbers artificially set by a group of individuals. This predefinition leads to the definition of resistance levels such as sensitive, medium or high.
The first classification, which will be described below, is based on chemical structure molecules of antibacterial agents and is most often used in medical practice.
 The following division of antibiotics occurs on the basis of their effect when exposed to bacteria:
The following division of antibiotics occurs on the basis of their effect when exposed to bacteria:
Antibacterial hygiene products without triclosan
Antibiotic boundaries are only human interpretations of the data and do not always reflect reality. The bactericidal effect, also called "microbiological activity", is achieved through 3 necessary mechanisms. First, the antimicrobial agent must bind to specific sites of attack in bacteria, which are different for each drug class. Second, the drug must receive sufficient concentrations to occupy a critical number of sites. Finally, the drug must remain at the binding sites for a sufficient period of time so that while the bacterium tries to carry on with its normal biochemical metabolism, it fails due to the presence of the antibiotic.
- Bacteriostatic antibacterial drugs inhibit the growth of bacteria, but do not directly destroy them. Their task is to reduce the population of bacteria, and its remnants will be completely destroyed. the immune system organism.
- Bactericidal antibiotics - destroy bacteria, affecting their vital systems.
The latter classification is based on the magnitude of the impact:

Prescribing broad-spectrum drugs
The appointment of broad-spectrum antibiotics is indicated in the following cases:

How to use antibiotic medicines correctly?
When prescribing and taking antibacterial agents, especially a broad spectrum of action, it is necessary to observe a number of simple rules and recommendations:
The liver is the main organ human body who takes an active part in the transformation medicines accepted by man. That is why it is so it is important to protect your liver from negative impact after or during forced antibiotics with ...

The main groups of medicines
Antibacterial drugs of a wide spectrum of action, are divided depending on their chemical structure into several large groups.
The main feature of these antibiotics is the presence of the so-called beta-lactam ring. The first representatives of this group of antibacterial agents were obtained from fungi of the genus Penicillium, from which they got their name.
 This group of drugs has several distinct advantages:
This group of drugs has several distinct advantages:
- the widest spectrum of activity among all antibiotics (however, in Lately species of bacteria resistant to penicillin began to spread);
- pronounced bactericidal effect, contributing to the rapid destruction of bacteria in the body.
Penicillins act on the mechanisms of bacterial wall formation, blocking these processes, which leads to the destruction of unwanted bacterial flora.
 Penicillins exist in several dosage forms: tablets and solutions, which allows them to be used both for oral administration and for intramuscular and intravenous injections.
Penicillins exist in several dosage forms: tablets and solutions, which allows them to be used both for oral administration and for intramuscular and intravenous injections.
The most commonly used antibiotics in this group are Ampicillin and Amoxicillin. The latter has a protected form - Amoxiclav, which allows it to be used in the destruction of bacteria that are not sensitive to penicillins.
Important! This group antibacterial drugs, most often provokes allergic reactions in the patient's body. In this connection, it is necessary to use these antibiotics with great caution in people with allergic manifestations and diseases.
Cephalosporins
Cephalosporins are the second most commonly used group of broad-spectrum antibiotics. They are the most resistant drugs to the effects of various protective enzymes of bacteria.
As a rule, all cephalosporins are divided into several generations: starting from the first, oldest, and ending, modern drugs fourth generation.
Typical representatives of cephalosporins:
- Cefotaxime;
- etc.



Macrolides
It is used with caution for the treatment of diseases, due to the high risk of developing side effects and allergic reactions. However, on this moment, it is macrolides that are considered the most effective antibiotics wide spectrum of activity.
A prominent representative of macrolides is Azithromycin, which has been used to treat many bacterial infections: from inflammation lymph nodes before purulent diseases internal organs.
Tetracycline series
Like previous antibiotics, tetracyclines are characterized by a wide spectrum of action and are often used to treat various infections.
Feedback from our reader - Maria Ostapova
I recently read an article that said that you need to start treating any disease with cleansing the liver. And it was told about the "Leviron Duo" remedy for protecting and cleansing the liver. With help this drug you can not only protect your liver from the negative effects of taking antibiotics, but also restore it.
I was not used to trusting any information, but I decided to check and ordered a package. I started taking it and noticed that I had strength, I became more energetic, the bitterness in my mouth disappeared, discomfort in the abdomen, complexion improved. Try it and you, and if anyone is interested, then below is a link to the article.
Preparations of this group can suppress the growth of bacteria, and have a pronounced bacteriostatic effect.
Aminoglycoside preparations
Most effective for aerobic microorganisms, however, they can also have an effect on other bacteria, and therefore, they also belong to the group of broad-spectrum antibiotics.
The main advantage is a strongly pronounced bactericidal effect, which allows you to quickly cope with any infectious disease, regardless of the route of administration of the drug and concomitant diseases sick.
They are the drug of choice for immunodeficiencies in a patient.
The most effective representatives of this group of antibacterial drugs:


Fluoroquinolones
They have a strong bactericidal effect. Capable of influencing atypical forms bacteria, which helps to cope with severe forms of diseases. Very important feature fluoroquinolones - their contraindication for use in pregnant and lactating mothers, due to the risk of complications from the fetus and child.
 Representatives of this group of drugs:
Representatives of this group of drugs:
- Moxifloxacin.
Taking broad-spectrum antibacterial agents necessary measure with the development of many infectious diseases. In this regard, it must be remembered that their appointment is the prerogative of the doctor.
Your body strives to be healthy, help it in this!
Do you and your family get sick very often and are treated with antibiotics alone? Have you tried many different medicines, spent a lot of money, effort and time, but the result is zero? Most likely, you are treating the effect, not the cause.
Weak and reduced immunity makes our body DEFECTIVE. It cannot resist not only infections, but also pathological processes that cause TUMORS AND CANCER! If you are familiar with:
- frequent respiratory colds and viral diseases;
- SARS with long and severe course;
- persistent pustular skin lesions;
- swollen lymph nodes;
- fungal infection nails, skin and mucous membranes (onychomycosis, candidiasis);
- tuberculosis infection in any form and manifestation;
- resistant to treatment and constantly recurring diseases respiratory tract, sinuses, urinary system;
- poor wound healing;
- general weakness, chronic fatigue.
We urgently need to take action! That is why we decided to publish an exclusive interview with Alexander Myasnikov in which it is divided penny method strengthening immunity.