Each of us loves to soak up the warm sun in the summer.
But few people know that excessive exposure to the sun can cause many skin diseases.Sun fungus or solar lichen belongs to the group of infectious skin diseases.
Skin fungus begins its activity in the spring and summer. When exposure to the sun is especially dangerous for humans. The disease often affects people under 30 years of age.
The disease is called beach fungus or sun lichen. All dermatologists claim that the main reason for its development is damage to the upper stratum corneum of the epidermis a certain type fungi of the genus Malassezia and Pityrosporum.
The fungal pathogen can be transmitted to healthy person from a patient during prolonged direct contact. The contact must be long-lasting. The disease itself can be considered non-contagious.
The risk of infection can be defined as the state of the human body as a whole. At weak immunity any fungus is actively developing.
It can take a long time from the moment of infection to the appearance of the first signs of the disease - several weeks. If there are favorable conditions in the body, the fungus begins to actively reproduce. There are many other reasons for the development of sun fungus.
Let us note the effect of the sun and ultraviolet radiation on the skin, because of this the disease is called “beach fungus”, “solar lichen”.
Long exposure to ultraviolet rays of the sun or solarium poses a risk of high fungal activity.
Provoking factors may be:
- vegetative-vascular dystonia;
- decreased immunity;
- obesity;
- diabetes mellitus;
- frequent infectious and colds;
- long-term use of antibiotics;
- imbalance of intestinal microflora;
- excessive sweating;
- application low-quality cosmetics skin care;
- excessive use of sunscreens and lotions;
- presence of allergies.
Skin pigmentation appears during the warm season. Beach or sun lichen is a seasonal disease. The fungus spreads to the skin of women and men.
Complaints come from young people under the age of 25-30. But children and the elderly can get sunburn fungus.
Symptoms of sun beach fungus
Beach fungus appears characteristic symptoms. The main indicator of fungus is the appearance of uneven and asymmetrical spots on the skin. These spots have jagged edges and a rounded shape.
As for color, it can be from light milky, coffee to red.
Localization locations are varied:
- neck;
- back;
- stomach;
- breast;
- scalp in young children;
- armpits;
- limbs.
With sun fungus, inflammation of the skin is not typical. Therefore, the formation of blisters, bubbles, and elevations on the skin is not observed. Painful sensations no either. This disease rather brings aesthetic and cosmetic inconvenience to the patient.
If you scrub the stains a little, they may begin to peel. Over time small spots begin to join together, forming one large solid spot. Upon acceptance sunbathing, the rashes do not tan, so they are noticeable in contrast with dark tanned skin.
There is no itching, burning or pain observed. If the patient begins to complain of discomfort, it can be argued that a secondary bacterial infection has entered the body.
People often confuse sun beach fungus with sun allergy. These diseases differ in their characteristic features. At sun allergy the patient feels strong itchy skin, inflammation, pain, burning.
How to treat beach fungus
 This type of fungus manifests itself clearly severe symptoms. Treatment should only be prescribed by a doctor. You should not self-medicate. This way it will only be possible to hide the manifestations a little, but the problems will not go away.
This type of fungus manifests itself clearly severe symptoms. Treatment should only be prescribed by a doctor. You should not self-medicate. This way it will only be possible to hide the manifestations a little, but the problems will not go away.
Therefore, you need to visit a dermatologist. The doctor is not limited to just a visual examination. A series of tests are required to help the specialist identify the main causative agent of the disease.
This is how they resort to help following methods research:
- Luminescent study. The doctor examines the spots under a Wood's lamp. These mushrooms shine in certain shades and colors.
- Dermatoscopy of spots.
- Balzer test.
- Microscopic examination of the contents from the surface of the stains.
- Test for Besnier syndrome.
- General blood test.
After receiving the test results, the doctor may prescribe treatment. Among the methods of treating solar fungus, one can note the use of topical medications, strengthening the immune system, and compliance with preventive measures (avoiding prolonged exposure to the sun).
Dermatologists prescribe special creams and ointments to lubricate fungal-affected skin areas.
This is what local therapy is all about. High efficiency drugs noted:
- clotrimazole;
- terbinafine;
- sulfur ointment;
- sulfur solution;
- resorcinol alcohol;
- naftifine;
- cycloperox;
- Lamisil.
Among modern drugs The doctor may prescribe some antifungal sprays and drops. This is at the discretion of the doctor, who takes into account individual characteristics the patient’s body, the course of treatment of the fungus by other means.
To consolidate the result and prolong the period of remission, means are used for general therapy. Sometimes prescribed antifungal tablets orgunal, fucis, ketoconazole, itraconazole.Taking cycloserine will help restore the usual color of the affected skin.
To strengthen the immune system, any immunomodulators are used. It is important to undergo therapy vitamin complexes. Such integrated approach to the treatment of solar fungus will help the patient get rid of the problem in a short period of time.
Prevention measures
 Lovers of chocolate and bronze tans may be at risk. Therefore, in order to prevent the development of sun fungus, it is worth following some prevention rules.
Lovers of chocolate and bronze tans may be at risk. Therefore, in order to prevent the development of sun fungus, it is worth following some prevention rules.
Staying in the sun for more than an hour and a half can cause the formation of fungal pigmentation.
Among the preventive measures, the following rules can be noted:
- try to avoid visiting the solarium;
- do not use antibacterial shower gels and soaps daily;
- stay in the sun only in the morning and evening;
- be sure to use in summer sunscreen before going outside;
- regularly strengthen your immune system;
- during the hot season, do not wear clothes made of synthetic material;
- in case increased sweating, treat with talc skin folds, armpits;
- control the functioning of the endocrine system.
Subject to these simple rules You can support the full functioning of the whole body. This will prevent the development of sun fungus.
A timely detection problems allows you to quickly get rid of the disease. Therefore, you need to listen to changes in the body.
A dermatologist will tell you how to treat solar lichen, since you can’t leave everything as it is - the fungus will spread to the surrounding skin, as a result the spots will become even larger.
During the hot season and early autumn, light spots devoid of pigment may appear on the skin. irregular shape. They don't look aesthetically pleasing, but at least they're not contagious.
Causes of the disease
Solar lichen develops under the influence of certain fungi that are activated on the skin due to a drop in general immunity or other reasons, namely:
- Neglect of hygiene rules - rarely taking a shower and irregularly washing clothes.
- Long stays in countries with hot and humid climates.
- Immunodeficiency conditions - AIDS, use of immunosuppressants, consequences of cancer and chemotherapy.
- Diabetes and obesity.
- Liver pathologies.
- Exposure to the sun during hours of unfavorable radiation (from 11 a.m. to 4 p.m.).
- Solarium abuse.
- Increased sweating.
Symptoms of pathology
 Symptoms of sun lichen include:
Symptoms of sun lichen include:
- Appearance of lighter or lighter skin dark spots incorrect configuration. They are localized on the neck, shoulders, chest, back and armpits. Gradually, the spots merge and form large depigmented areas. These areas no longer perceive tanning and therefore become very noticeable.
- In children, spots can be located on the scalp, as well as on the arms and legs.
- The spots do not protrude above the surface of the skin and do not show signs of inflammation - hyperemia, redness and swelling.
- Peeling of the skin when scraped.
- Sometimes there is mild itching.
Please note that solar lichen appears after a long incubation period. The causative agent of the disease is capable for a long time live on outdoors, upholstered on clothing or skin surface. After infection, it can take from two weeks to several months. At some point in time, a person notices that he has strange light spots against the background of his tanned body. So don’t be surprised that the disease only appeared in the fall. IN winter time the spots are pink or brown in color. If a bacterial infection is associated with sun fungus, soreness, itching and severe peeling may develop.
Diagnostic measures
A dermatologist diagnoses such diseases. After a visual inspection, he will conduct several tests:

- Balzer iodine test. To do this, depigmented skin is treated alcohol tincture Yoda. Diseased skin will be more colored than healthy skin.
- Definition of Besnier's symptom. The skin on the affected spot and beyond is scraped off a little. They look at how much more it peels off in the affected areas.
- Light areas of the epidermis are examined under the light of a fluorescent lamp. Typically a dark brown, yellowish-red, or blue-green glow appears.
- The skin scraping is sent to microscopic examination to search for pathogens.
Manifestations of solar lichen must be differentiated from other skin diseases - Gibert's disease, leprosy, vitiligo, secondary hypopigmentation, leucoderma and syphilitic roseola. In this regard, the patient may be referred to additional research— PCR diagnostics, analysis of scrapings for the presence of Treponema pallidum and others.
Treatment of the disease
How formerly man If you consult a doctor, the easier and faster the cure will come. Initially, only local antifungal drugs are used in the form of sprays, lotions, solutions and creams.
They are distributed more evenly over the skin, do not interfere with its breathing and do not stain clothes. If the disease does not respond to therapy or relapses occur, the patient is additionally prescribed systemic medications.
 Most often, doctors recommend rinsing with anti-dandruff shampoos - Sebozol, Dermazol, Nizoral or Perhotal - before applying antifungal agents to the skin. After rinsing and drying, the epidermis is treated with a prescribed solution - Miramistin, 5% resorcinol and salicylic alcohol or lotion with selenium sulfide. The last product should be kept on the skin for 10 minutes and then washed off. Lamisil, Bifalazole, Mycozolon, Cycloperox, Clotrimazole, Naftifine, Terbinafine or others ointment is applied to dry skin. This is done 1 or 2 times a day. Please note that you should not treat skin with burns, abrasions or other injuries. Sometimes some antifungal medications can cause local allergic reaction- itching, redness and burning. In this case, it is better to observe and then consult with your doctor.
Most often, doctors recommend rinsing with anti-dandruff shampoos - Sebozol, Dermazol, Nizoral or Perhotal - before applying antifungal agents to the skin. After rinsing and drying, the epidermis is treated with a prescribed solution - Miramistin, 5% resorcinol and salicylic alcohol or lotion with selenium sulfide. The last product should be kept on the skin for 10 minutes and then washed off. Lamisil, Bifalazole, Mycozolon, Cycloperox, Clotrimazole, Naftifine, Terbinafine or others ointment is applied to dry skin. This is done 1 or 2 times a day. Please note that you should not treat skin with burns, abrasions or other injuries. Sometimes some antifungal medications can cause local allergic reaction- itching, redness and burning. In this case, it is better to observe and then consult with your doctor.
Daily procedures are continued for 2 weeks. This is followed by a month-long break, during which the result of the treatment is assessed. Usually, after rest, the course of treatment is repeated. To improve overall immunity, it is usually recommended to take a monthly course of complex vitamins.
If this treatment did not help or relapses are observed, the doctor will use systemic antifungal drugs in tablets and capsules - Itraconazole, Ketoconazole or Orungal. These medications should speed up healing and improve general condition patient. The duration of taking the drug and dosage are selected by a specialist. When strong adverse reactions he can replace the medicine with an alternative one.
During treatment, you need to bathe 2-3 times a day to keep your skin clean and dry. It is possible that the doctor will prescribe antihistamine to prevent itching, as scratching slows down the healing process.
 If you are one of the obvious opponents traditional treatment or are afraid to go to a dermatologist, you can try folk recipes. If you notice small, light spots on your skin, try treating sunburn at home. Treat discolored areas every three hours apple cider vinegar, 5% salicylic alcohol or tincture of iodine. Try to alternate solutions. After drying in air, apply 5% salicylic, 5-10% sulfur or sulfur-salicylic ointment to the affected areas of the skin.
If you are one of the obvious opponents traditional treatment or are afraid to go to a dermatologist, you can try folk recipes. If you notice small, light spots on your skin, try treating sunburn at home. Treat discolored areas every three hours apple cider vinegar, 5% salicylic alcohol or tincture of iodine. Try to alternate solutions. After drying in air, apply 5% salicylic, 5-10% sulfur or sulfur-salicylic ointment to the affected areas of the skin.
It is recommended to treat clean, dry skin with depigmented spots sea buckthorn oil, oil tea tree or rosehip. Calendula is known to be a strong antiseptic. Prepare homemade tincture from calendula flowers. Pour one part of the dried flowers of the plant into five parts of alcohol and leave for 2 weeks. Strain and pour the tincture into a dark glass bottle. Wipe the affected areas as often as possible throughout the week.
If you don't have skin allergies, try making turmeric paste. Mix a teaspoon of spice with a small amount of water (less than 1/2 teaspoon). Apply the paste to depigmented skin twice a day. Keep it on for 30 minutes and then rinse with water. If this does not help, you still have to visit a doctor.
Prevention of pathology
In a person suffering from solar fungus under the influence ultraviolet rays the spots become even more contrasting compared to the rest of the skin, so it is recommended to refrain from tanning under the sun and in a solarium. As prophylactic to all fans beach holiday It is advised to use high-quality sunscreen, always lie on clean towels, not on sand, and wear light sandals. But with spots on your skin, it’s better not to show off on the beach. Surely, dissatisfied neighbors on the sunbeds will look sideways at you.
People with excessive sweating It is recommended to always wear clothes made from natural fabrics; they absorb sweat well and prevent the skin from steaming. In hot weather, you need to change your outfits daily, and after washing, iron them on both sides. Cotton bedding in the summer is useful not only for people with hyperhidrosis, but also for everyone else suffering from heat.
Personal hygiene is equally important. After visiting the beach, you should always shower with a cleanser. As a protective measure, it is suggested to use antifungal shampoo with ketoconazole, purchased at a pharmacy. It can also be used to wash the body. In the summer you need to swim as often as possible - 3-4 times a day, and in winter a little less often. Manifestations of solar lichen look ugly. It is reassuring that the disease is not dangerous, but it is necessary to be treated. Please note that only a doctor can distinguish this disease from the symptoms of vitiligo, leprosy and others.
Pityriasis versicolor, which is popularly called “solar” or “multi-colored” due to the peculiarities of the appearance and course of the disease, can be found on the body by lovers of a strong tan. The symptoms of the disease are pronounced and appear as spots that stand out on the skin with their color. Treatment of this disease does not cause difficulties, but the lack of therapy leads to relapses, then it is more difficult to cure the disease.
Causes of the disease
Main causes of the disease:
- Excessive exposure to sunlight, which provokes the growth of fungus on the skin and damage acid balance. Often pityriasis versicolor called a “marker” of liver disease and biliary tract- it appears to a greater extent in people who have problems with the operation of these internal organs.
Excessive sweating can lead to the appearance of sun lichen. - Predisposed to illness endocrine diseases such as obesity and diabetes.
- Weakening of the immune system;
- Frequent use antibacterial agents skin care products that violate normal level RN on the skin.
- Stress on the skin caused by frequent visits solarium.
It is these reasons that cause the appearance of solar lichen, which manifests itself in the form of spots of white, milky, beige color on areas of the skin that are most susceptible to ultraviolet rays: on the back, shoulders, forearm, arms, décolleté.
Symptoms of the disease
Having noticed the first symptoms in the form of spots, it is recommended to stop exposure to the sun. But it should be borne in mind that solar lichen may not manifest itself for a long time - incubation period The illness lasts from 2 weeks to 3 months. Therefore, it can appear not only in summer, but also in the cold season, most often in autumn.
The course of the disease itself is long - about 2 weeks, but solar lichen is not contagious. It is transmitted from person to person only through very close and prolonged contact with the source of the disease.
There are the following stages of disease development:
Solar lichen, apart from a cosmetic defect, does not cause any particular harm to the body. At timely diagnosis the disease is not difficult to treat and you can sunbathe in the future without fear of serious consequences.
Treatment of deprivation
Before starting treatment, the doctor conducts a diagnosis to exclude from suspicion diseases whose symptoms are similar to solar lichen - vitiligo, syphilis, leprosy, Gibert's disease.
It is not difficult to cure solar lichen if you follow all the recommendations of a dermatologist. When choosing a drug, it is better to give preference to forms in the form of sprays, lotions, solutions, ointments - they are distributed more easily and evenly over the skin. It is recommended to treat lichen on the body by adhering to the following scheme:
- Before applying to ringworm antifungal ointment, it is recommended to wash the areas of the body affected by deprivation with shampoo that is used to treat dandruff: Nizoral, Sebozol, Dermazol, Perhotal.
- Then antifungal ointment Clotrimazole or similar drugs: Miramistin, Cycloperox, Lamisil, Bifalazole, Terbinafine, etc.
The course of treatment is determined by the doctor and is usually 2 weeks of daily use. antifungal drugs. After this, a month-long break is taken and the treatment is repeated.
Also practiced by others less effective methods treatment of solar lichen:
- You can cure extensive lichen by using sulfur, salicylic or sulfur-salicylic ointment.
- Small lesions can be treated with iodine or iodosalicylic alcohol, apple cider vinegar, 5% salicylic alcohol. These drugs are applied to the lichen very often - every 3 hours.
- Because pityriasis versicolor appears due to disturbances in the functioning of the immune system, then in parallel with the main treatment, the doctor prescribes a course of multivitamins.
Treatment with folk remedies
Treatment is often practiced fungal infection skin traditional methods, which many consider less dangerous and more effective than the use of pharmaceutical drugs.
- St. John's wort, rose hip, peach and sea buckthorn oils cope well with fungal skin diseases. Can be purchased ready-made drugs at the pharmacy and lubricate the affected areas on the body.
- You can prepare your own tincture from 5 parts vodka and 1 part calendula flowers. Apply ringworm very often - up to 5 - 6 times a day.
- Also effectively copes with this disease onions, the juice of which is used to wipe stains on the skin.
- Since lichen occurs due to an imbalance in the acid balance of the skin, sorrel can be used for treatment. To do this, its roots and leaves are crushed into a paste, mixed with sour cream and rubbed into the affected areas. This ointment works very well against sunburn.
- It is also recommended to treat pityriasis versicolor from the inside. To do this, prepare a drink from baking soda, a teaspoon of honey and a tablespoon of apple cider vinegar.
Disease prevention
- do not overexpose yourself to the sun;
- be sure to use sunscreen;
- before sunbathing after swimming, the skin must be wiped with a towel, only then exposed to the sun;
observe safe hygiene measures to avoid catching the fungus from other people: do not use other people’s towels, be sure to lay your own bedding on the sunbed, do not lie on bare sand; - wear clothes made from natural fabrics.
You can cure this disease using traditional methods, but it is better to entrust the treatment to proven pharmaceutical antifungal drugs, which will be selected by a dermatologist.
Solar lichen, or beach lichen (also called pityriasis versicolor, pityriasis versicolor) is an infectious disease that affects the skin on different areas bodies. U of this disease The seasonal nature of the flow is noted: greatest number cases of sun fungus infection occur in spring and autumn. Most often registered in young people and children.
As a rule, pityriasis versicolor is characterized by low contagiousness (doctors classify it as low contagious infectious pathologies skin): the disease can be transmitted from a sick patient to a healthy one only through prolonged and close contact. The likelihood of developing such a pathology is strongly influenced by factors that create favorable conditions for infection in a person.
Most dermatologists believe that they affect the stratum corneum of the skin and hair follicles fungi belonging to the genus Pityrosporum or Malassezia. Spores can only be transmitted through prolonged skin-to-skin contact. Infection of children often occurs in kindergartens, summer camps or in others public places.
The likelihood of “catch” a sore increases with certain disorders in the body.
After fungal spores come into contact with the skin favorable conditions active reproduction of the infection with the formation of spots and lesions begins after a few weeks.
Favorable factors for the development of fungus:
- malfunctions of the immune system;
- insufficient blood supply to the skin due to vegetative-vascular dystonia;
- endocrine disorders (diabetes, overweight);
- acute respiratory infections and acute respiratory viral infections with severe course;
- long-term antibacterial therapy;
- the predominance of synthetics in clothing;
- application antibacterial soap or gel that disrupts the normal balance of skin microflora,
- increased sweating,
- use of low quality cosmetics;
- long stay under sun rays, including under UV radiation in a solarium.
In addition, among dermatologists there is an opinion that high risk the occurrence of pityriasis versicolor occurs in persons diagnosed with lymphogranulomatosis or tuberculosis.
Symptoms
Often patients do not know what solar lichen is, and initial stage They mistake illness for some minor irritation. The first thing you need to pay attention to if you suspect a sun fungus infection is the presence of large quantity spots that have uneven, scalloped, clearly defined boundaries. The affected areas are yellowish, brownish or dark brown in color. There is peeling of the skin and severe redness when combing it.
The spots do not show pain or swelling. Inflammatory process also no. As the disease progresses, the affected areas grow, uniting with each other and forming a large irregularly shaped lesion.
 The skin most often affected is the scalp, armpits and extremities, but other parts of the patient's body can also be affected.
The skin most often affected is the scalp, armpits and extremities, but other parts of the patient's body can also be affected.
Patients infected with a fungal infection do not experience any discomfort. If itching, inflammation and burning appear, this indicates that a bacterial infection has joined the underlying disease. The areas affected by sun fungus do not change their color when exposed to ultraviolet radiation and contrast sharply with tanned skin on other parts of the body.
Diagnostic and therapeutic procedures
As a rule, to diagnose the disease, a simple examination of the person by a dermatologist or dermatoscopy of the infected area of the epidermis is sufficient.
If in doubt, the doctor may prescribe:
- testing using the Balzer iodine test;
- Beignet test (lichen spots peel off from light touches);
- examination using a fluorescent lamp (under the rays of such a light source, dark brown, bluish-green or brownish-yellow skin is visible);
- microscopic examination of the scales (fungus will be visible in the particles of the epidermis).
 When making a diagnosis, your doctor will need to rule out other skin diseases, similar in symptoms: vitiligo, secondary hypopigmentation, syphilitic roseola and leucoderma. For this purpose, the patient is prescribed appropriate specific tests.
When making a diagnosis, your doctor will need to rule out other skin diseases, similar in symptoms: vitiligo, secondary hypopigmentation, syphilitic roseola and leucoderma. For this purpose, the patient is prescribed appropriate specific tests.
Once the diagnosis is established, therapeutic procedures are carried out. The disease is treated in outpatient setting for a long time, until all the symptoms of the disease completely disappear. First of all, the patient is prescribed local antifungal substances, with severe course ailments are added various systemic drugs.
Among the most effective and harmless means, used for external treatment of affected areas, are isolated the following medications with antifungal properties:
- salicylic ointment;
- Terbinafine;
- Lamisil;
- Naftifin et al.
They can treat lichen in a child.
It is better to use preparations produced in the form of lotion, liquid solution or spray. Active ingredient thin layer applied to the area infected with the fungus and rubbed into skin with lungs in a circular motion.
 For general treatment pathologists actively use systemic antifungal drugs, for example, they effectively suppress mycotic infection with Orungal or Ketoconazole.
For general treatment pathologists actively use systemic antifungal drugs, for example, they effectively suppress mycotic infection with Orungal or Ketoconazole.
These remedies not only significantly improve the patient’s well-being, speed up recovery, but also prevent recurrence of the disease.
Important! Self-treatment sun lichen using folk remedies not only will not lead to positive result, but can also provoke a significant deterioration in the condition of the sick person. The choice of therapy, the selection of effective antifungal drugs and the preparation of a course of their administration can only be carried out by a competent dermatologist.
If the patient has large areas of pigmented skin, the dermatologist prescribes Cycloserine to restore the normal color of the epidermis.
Preventive measures
Fans of a bronze tan need to think carefully about whether it is worth risking their skin health for this. You can get not only pityriasis versicolor, but also other types of photodermatosis. Following simple recommendations will significantly reduce the risk of contracting a fungal infection.
 Among the main preventive measures, the following should be noted:
Among the main preventive measures, the following should be noted:
- visits to the solarium should be canceled or at least the number of these procedures should be significantly reduced;
- Do not use soap or gel with antibacterial additives every day;
- It is better to be under the sun in the morning or evening; during the day you should try to be more in the shade;
- when going to the beach, you should use a special cream with a UV filter;
- Patients who have had sunburn should avoid wearing synthetic clothing;
- at excessive sweating you should wipe the skin with infusion oak bark;
- failures in immune system eliminated with the help of strengthening drugs and hardening;
- children should take sunbathing only under adult supervision.
If the above recommendations are strictly followed, the risk of contracting sunburn or relapses is reduced to zero. If the disease does begin, do not despair. Today, a dermatologist has a large selection at his disposal. effective drugs for the treatment of fungal skin lesions. If you contact a specialist in a timely manner, you will be able to defeat the pathology in short term.
Solar lichen refers to infectious diseases. Characteristic features diseases serve as flaky age spots on the skin. This lichen is a seasonal disease, and fungal bacteria reach a particular peak of activity in the spring and autumn. The risk category includes men and women under thirty years of age.
Solar lichen can be transmitted from a sick person to a healthy person only with close, prolonged contact. For the development and progression of the disease, the body must have a favorable background and predisposing factors.
Causes of sunburn infection
Fungal dermatological disease, which in medicine is called keratomycosis or multi-colored, spreads only to the hair cuticles and the stratum corneum of the epidermis. Development pathological process The following factors may contribute:

Some dermatologists argue that the manifestation of symptoms of solar lichen may indicate the presence of pulmonary tuberculosis or lymphogranulomatosis.
Solar lichen and its symptoms
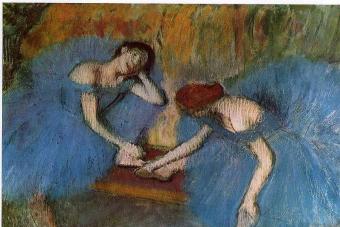
Solar lichen photo
 The appearance on the patient's body of a large amount asymmetrical round spots, as shown in the photo above, with scalloped, uneven or clearly demarcated edges, can be classified as the main signs of solar lichen. The skin of a sick person begins to peel off when scratched and acquires different colors in the affected areas: yellow, dark brown, pinkish brown and coffee shades.
The appearance on the patient's body of a large amount asymmetrical round spots, as shown in the photo above, with scalloped, uneven or clearly demarcated edges, can be classified as the main signs of solar lichen. The skin of a sick person begins to peel off when scratched and acquires different colors in the affected areas: yellow, dark brown, pinkish brown and coffee shades.
Sun spots do not show signs of inflammation and do not rise above skin. Lichen spots do not deliver painful sensations and swelling. As the disease progresses, the lesions are capable of growing and can merge into a single area the size of the palm of an adult. Localization sites most often form on the back, neck, abdomen, chest, and on the sides of the torso.
Sun pigmented areas in children and adolescents may be present on the scalp, on the skin of the arms and legs, and in the armpits. In children, predisposing factors may be considered allergy to sun rays, prolonged exposure to direct sunlight and weakened immunity.
Treatment of solar lichen in children requires avoiding exposure to the sun from 11 to 16 hours of the day, at the most dangerous time days. To strengthen protective forces It is advisable for the child’s body to diversify the child’s menu and give him more vitamin foods or regular multivitamins in the form of tablets.
Pityriasis versicolor does not cause the patient any discomfort. If the sick person experiences such discomfort such as itching, burning and soreness, this may indicate the accession bacterial infection. Areas of skin affected by lichen stand out noticeably against the background of the rest of the tanned skin, because tanning does not apply to these areas.
How to treat solar lichen
A dermatologist, after a visual examination and dermoscopy tests of the affected areas, can easily diagnose pityriasis versicolor. Can also be assigned additional tests in case of doubt by the doctor using a fluorescent lamp, scrapings of the epidermis of the skin and others.
To exclude the presence of other similar diseases, you may need to undergo an RPR test and PCR diagnostics, as well as exclude the presence of Treponema pallidum by ordering a microscopic scraping analysis.
Treatment of solar lichen is carried out on an outpatient basis and is carried out until the symptoms of the disease completely disappear. Treatment of lichen begins with local antifungal agents. If the solar pathological process spreads and relapses, the doctor may prescribe the use of systemic medications.
For local processing foci of lichen lesions are often prescribed:

When choosing a drug for the treatment of lichen, it is better to opt for antimycotics produced in the form of sprays, lotions or solutions. Medicine Apply evenly to sunburn-affected areas of the skin and massage light movements rubbed in.
Treatment with drugs in the form of a cream will not create a greasy film on the skin, which is excellent option for the warm season. Lotions and sprays promote uniform application to the skin surface, regardless of the affected area and location of the focal areas. Treatment is achieved by treating every millimeter of the affected areas with drugs.
To prevent relapses and general treatment of lichen, systemic antifungal agents, such as ketoconazole, itraconazole, orungal. These drugs help improve general well-being the patient and his speedy recovery. To get rid of lichen pigmentation, cycloserine is used.
To avoid complications, you should not self-medicate. Traditional methods treatment for solar lichen do not have the desired effect and most often turn out to be useless. Only an experienced dermatologist can be trusted to draw up a treatment regimen and prescribe the dosage of antifungal drugs taken.
Most often doctors appoint complex treatment depriving according to the following principle:
- Local therapy using traditional medicine.
- Taking general strengthening medications.
- Application preventive measures acceptance.
As a preventative measure can be called the following:

During treatment for lichen and after it It is not recommended to use aggressive agents for cleansing the skin, such as peeling, scrub and others.